
NORTH AMERICAN DIVISION
Healthcare Assistance Plan
Ascend to Wholeness Plans
SUMMARY PLAN DESCRIPTION (SPD)
JANUARY 01, 2021
TO WHOLENESS
HEALTHCARE PLANS
4818-5448-8033.1

2
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
PLAN ADMINISTRATOR
North American Division of Seventh-day Adventists with duties delegated to:
Adventist Risk Management, Inc.
12501 Old Columbia Pike
Silver Spring, MD 20904
www.adventistrisk.org
MEMBER AND PROVIDER SERVICE
1-888-276-4732
benets@adventistrisk.org
PREFERRED PROVIDER ORGANIZATION (PPO) NETWORK (MEDICAL AND DENTAL)
Aetna Signature Administrators PPO by Aetna (except Oakwood University, see App. C)
https://asalookup.aetnasignatureadministrators.com
MEDICAL, DENTAL, AND VISION CLAIMS PROCESSING
WebTPA
P.O. Box 99906
Grapevine, TX 76099-9706
EDI: 75261
1-888-276-4732
PRESCRIPTION CLAIMS PROCESSING
Express Scripts
1-800-841-5396
UTILIZATION REVIEW MANAGER
(MEDICAL NECESSITY, PRE-CERTIFICATION, AND APPEALS)
Adventist Health Benets Administration
2625 SE 98
th
Ave.
Portland, OR 97266
1-888-276-4732
If you (and/or your dependents) have Medicare or will become eligible for Medicare in the
next 12 months, a Federal law gives you more choices about your prescription drug coverage.
Please see page 106 for more details.

3
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Welcome
Translation Services are Available
Key Plan Information
Schedule of Benets
Denitions
Eligibility, Enrollment and End of Coverage
Employee-Share Contribution
Pre-Certication Program
Providers and Facilities Available Under the Plan
General Benet Rules
Benets Description - Medical
Benets Description - Dental
Benets Description - Vision
Benets Description – Prescription Drugs
Benets Description – Complementary and Alternative
Limitations and Exclusions
Claims Procedures
Benets Available from Other Sources
Coordination of Benets
General Plan Information
Health Insurance Portability and Accountability Act Provisions (HIPAA Privacy Policy)
Medicare Part D Notice
Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP)
APPENDIX A – List of Covered Preventive Services
APPENDIX E – Care During the COVID-19 Pandemic
APPENDIX F – Extension of Certain Plan Deadlines During the COVID-19 Pandemic
4
4
5
7
19
30
39
40
47
49
50
60
63
64
69
70
74
89
93
98
102
106
108
111
121
122
TABLE OF CONTENTS

4
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Welcome
This Plan is intended to be, and has been since its establishment, a church plan within the meaning of Internal
Revenue Code Section 414(e) and ERISA Section 3(33). The North American Division of Seventh-day Adventists
established this Plan for its participating employers, which are Seventh-day Adventist Organizations, inclusive of
the General Conference of Seventh-day Adventists and its subsidiaries and aliates, that participate in the Plan
for their eligible employees based in the United States and certain included territories (Guam and the Northern
Mariana Islands), and the employees’ eligible dependents in order to fulll a key tenet of the Seventh-day Adventist
Church (the “Church”) in furthering the healing ministry of Jesus and, through his love and healing power,
promoting prevention, whole-person care, and physical, mental, and spiritual health. As a church plan, the Plan is
exempt from ERISA and is subject to the Church Plan Parity and Entanglement Prevention Act of 1999.
The Plan provides a broad range of benets for medical, vision, dental, and prescription expenses which you
and your eligible dependents may incur in the United States (and, if you are stationed in an included territory, also
provides benets for covered services received in an included territory). The Plan also pays a portion of the cost
of emergency medical expenses incurred anywhere in the world for outpatient care, hospital care, surgery,
preadmission services, and prescription drugs. Non-emergency services received outside of the United States are
excluded from coverage (except if received in an included territory if you are stationed in an included territory).
The Plan is self-funded by means of employer and employee contributions. Each participating employer is
responsible for funding only the claims of its own employees and its own employees’ dependents. Each
participating employer (including your employer) has designated the North American Division of Seventh-day
Adventists to administer the Plan, which it does via its delegate Adventist Risk Management, Inc. (which is part
of the Church). The North American Division of Seventh-day Adventists (the plan administrator of this Plan), its
delegate Adventist Risk Management, Inc. (“ARM”), and ARM’s representatives and delegates administer the Plan.
When the term “plan administrator” is used in this Plan, it generally refers to ARM as the delegate of the North
American Division of Seventh-day Adventists.
This Summary Plan Description (SPD) is designed to provide you with important information about your Plan’s
benets, limitations and procedures. Benets described in this document are eective January 1, 2021. This SPD is
also the Plan document. This SPD describes the benets available to all enrollees of the Plan; however, depending
on your state or territory of residence, you may be entitled to additional benets by state or territory law.
Your benets are aected by certain limitations and conditions, which require you to be a wise consumer of
health services and to use only those services you need. Also, benets are not provided for certain kinds of
treatments or services, even if your health care provider recommends them. Many items are not covered by the
Plan even though they may provide signicant patient convenience or personal comfort. The Plan does not, and
is not intended to, cover all healthcare services and products that are available, particularly treatment that is not
medically necessary.
In order to participate in this Plan, you are required to make “employee-share contributions,” which you may think
of as premiums. However, this Plan is not an insurance program or policy.
In this SPD, the terms, “you” and “your” refer to the covered employee. The terms “we,” “us” and “our” refer to the plan
administrator.
Questions about the Plan should be directed to Customer Service at 888-276-4732 or to your plan administrator by
email at bene[email protected]g. Thank you for choosing us as your healthcare plan.
Translation Services are Available
Spanish (Español): Para obtener asistencia en Español, llame al 888-276-4732.
Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 888-276-4732.
Chinese (中文): 如果需要中文的帮助,请拨打这个号码: 如如如如如如如如如如如如如如如如如 888-276-4732.
Navajo (Dine): Dinek’ehgo shika at’ohwol ninisingo, kwiijigo holne’ 888-276-4732.

5
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Key Plan Information
Plan Name:
Healthcare Assistance Plan for Employees of Seventh-day Adventist Organizations of the North American
Division Aka Ascend To Wholeness Healthcare Plans (the “Plan”)
Plan Sponsor/Plan Administrator:
The Plan is sponsored by the North American Division of Seventh-day Adventists. For the purposes of both
(i) the privacy obligations under Health Insurance Portability and Accountability Act of 1996 (“HIPAA”), and
(ii) Plan nancial liability, your participating employer is the plan sponsor for its piece of the Plan. As such,
any obligation to you as an enrollee arising from this Plan is a general asset obligation of your participating
employer.
The Plan is administered by the North American Division of Seventh-day Adventists, which has delegated its
plan administrative duties to Adventist Risk Management:
Adventist Risk Management, Inc.
12501 Old Columbia Pike
Silver Spring, MD 20904
www.adventistrisk.org
benets@adventistrisk.org
(888) 276-4732
When the term “plan administrator” is used in this Plan, it generally refers to Adventist Risk Management as
the delegate of the North American Division of Seventh-day Adventists.
The plan administrator reserves the right to monitor telephone conversations and e-mail communications
between its employees and its customers for legitimate business purposes as determined by the plan
administrator. The monitoring is to ensure the quality and accuracy of the service provided by employees of
the plan administrator to their customers.
The plan administrator has the discretionary authority to administer the Plan in all of its details, including
determining eligibility for benets and construing all terms of the Plan. The plan administrator has the
discretion to determine all questions of fact and/or law that may arise in connection with the administration
of the Plan. The plan administrator may assign its duties to others, and the plan administrator has assigned its
duties to Adventist Risk Management and has granted Adventist Risk Management the authority to delegate
its plan administrative duties to other entities on its behalf.
Funding Medium and Type of Plan Administration: The Plan is self-funded by means of employer and
employee contributions. The portion the employee pays toward the total contribution is at a rate determined
by the participating employer. Each participating employer funds the Plan only for its own employees and their
dependents. The plan administrator provides claim processing and other administrative services to the Plan.
The plan administrator may delegate its duties to third parties. This is not an insured plan.
Plan Year: January 1 through December 31
Medical, Dental, and Vision Claims Processing:
WebTPA
P.O. Box 99906
Grapevine, TX 76099-9706
EDI: 75261 (888) 276-4732
www.AscendToWholeness.org

6
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Medical Necessity Pre-Certication/Utilization Review/Care Management:
Adventist Health Benets Administration
2625 SE 98th Ave.
Portland, OR 97266
(888) 276-4732
Amendment and Termination
This Plan may be terminated or this SPD may be changed or replaced at any time without notice, by a
resolution of the North American Division Committee of the General Conference of Seventh-day Adventists,
by the North American Division Risk Management Committee, or by the delegate of North American Division
of Seventh-day Adventists, which is Adventist Risk Management, or any authorized representative of the
North American Division of Seventh-day Adventists or its delegate, Adventist Risk Management. The right
to amend/terminate includes the right to curtail or eliminate coverage for any treatment, procedure, or
service, regardless of whether any covered employee is receiving such treatment for an injury, defect, illness,
or disease contracted prior to the eective date of the amendment/termination. Amendments may be made
retroactively.

7
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Schedule of Benets
The tables below summarize your Plan benets under your Plan election (Accelerate Plan or Access Plan),
applicable deductibles, the annual out-of-pocket maximums, and the co-payments and co-insurance
applicable to your coverage. This section only provides a summary of benets available. For a complete
discussion of the services covered under the Plan, as well as applicable benet limitations, exclusions from
coverage, and conditions of service that apply to your coverage, please refer to the subsequent chapters in
this SPD.
If you do not follow the procedures set forth in the Pre-Certication Program section
of the , no benets will be provided. Additionally, the expenses you incur due to not following the
Pre-Certication Program procedures will not be applied to your deductibles or out-of-pocket maximums.
( is not required for routine health care performed in a provider’s oce,
, emergency room, or via .)
Plan Coverage Levels – PPO Network
Generally, the Plan only covers services rendered by PPO facilities and PPO providers. Exceptions to this rule
are detailed in the Schedule of Benets.
Deductibles and Annual Out-of-Pocket Maximum
Deductible
A deductible is the amount of covered service expenses you must pay each year before the Plan will consider
expenses for reimbursement. An additional deductible applies for each enrollee you cover (except as limited
by the Plan’s out-of-pocket maximum). The annual deductible amount for each enrollee is shown in the table
below. Expenses incurred for services that are not covered services, even if received from a PPO provider, do
not count toward your deductible. There is a separate deductible for dental expenses.
There are deductibles for most medical and dental services. Certain benets are not subject to a deductible
and the expenses incurred for such benets do not count toward your deductible. The benets that are not
subject to a deductible are those listed in the Ancillary Medical Benets chart, oce/telehealth visits, urgent
care center visits, emergency room visits that do not result in hospital admission, preventive care services,
hospice, vision, and prescription drug expenses.
Please note that xed dollar co-payments do not apply toward your annual deductible.
The individual deductible is the amount of an individual’s covered expenses for dates of service within the
Plan Year period that must be paid by the enrollee before benets are paid by the Plan for that enrollee. Each
individual enrollee is subject to a separate deductible until the family deductible is reached. The family
deductible is the amount of the family’s collective covered expenses for dates of service within the Plan Year
period that must be paid by the enrollee before benets are paid by the Plan.
Deductible responsibilities are calculated and accrued based on dates of service, not dates paid. Benet
reductions due to non-compliance with the Plan or policy guidelines will not be credited toward the
deductibles.
Annual Out-of-Pocket Maximum
The annual out-of-pocket maximum is the most you pay during the year (January 1 through December 31)
before the Plan begins to pay 100% of the cost of covered services. The Plan maintains separate out-of-
pocket maximums for medical benets and pharmacy benets. Each out-of-pocket maximum is listed in the
Schedules of Benets below.
Generally, payments you make toward Plan coverage and benets, such as co-payments, co-insurance and

8
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
expenses incurred in meeting deductibles, apply toward the applicable annual out-of-pocket maximum.
However, the following amounts do not apply toward the annual out-of-pocket maximums:
• Your required employee-share contributions
• Disallowed charges
• Balance billed charges (that is, amounts above the usual, reasonable, and customary charge
billed by an out-of-network provider directly to an enrollee)
• Amounts paid or credited for SaveonSP specialty drugs, listed at www.saveonsp.com/
adventistrisk (unless you are stationed in an included territory), and any other amounts paid
or credited for any drug under a drug manufacturer patient assistance program; for example,
copay coupons (these are not true out-of-pocket costs)
• Amounts you pay for services listed in the Schedule of Benets under “Ancillary Medical
Benets,” such as alternative therapies, refractive eye surgery, hearing aids, and infertility
treatment
• Amounts you pay for dental and vision benets (except that amounts you pay for an under age
19 pediatric annual eye examination and one pair of standard, clear-lens, prescription glasses
per child will apply toward your out-of-pocket maximum)
• Benet reductions due to non-compliance with policy guidelines and expenses incurred due
to non-compliance with pre-certication.
You will be required to continue paying your employee-share contributions even after the Plan’s annual
out-of-pocket maximums are reached.
Out-of-pocket maximums are applied to each individual, regardless of whether the coverage is self-only or
other than self-only (family coverage). For example, if one individual in a family reaches the individual out-
of-pocket maximum, then the Plan will cover any additional costs for that individual’s covered services for the
remainder of the plan year. The remaining members of the family will still be subject to their own individual
out-of-pocket maximums until the total family out-of-pocket maximum has been reached, at which point the
Plan will cover the costs of covered services for all of the members of the family for the remainder of the plan
year.
Co-Insurance and Co-Payments
For PPO providers and PPO facilities, the usual, reasonable, and customary charge is the negotiated network
rate. For out-of-network providers and out-of-network facilities, there is no negotiated fee. Therefore, if you
use an out-of-network provider or out-of-network facility in one of the limited circumstances in which out-of-
network services are covered, please note that you might be “balance-billed” by the out-of-network provider
or facility (i.e., charged more than the usual, reasonable, and customary charge) and therefore could owe more
than your co-payment plus your co-insurance.
After you pay your deductible, the Plan will pay 100% of the usual, reasonable, and customary charge for
covered services less your required co-insurances and co-payments.
The percentages the Plan pays apply only to covered service expenses that do not exceed usual, reasonable
and customary charges. You are responsible for all non-covered service expenses and any amount that
exceeds the usual, reasonable and customary charge for covered service expenses.
The Schedule of Benets lists your co-insurance percentage of the cost of covered services (up to the usual,
reasonable, and customary charge). Co-insurance percentages are the portions of covered service expenses
paid by you after satisfaction of any applicable deductible. For example, if the listed percentage in the below

9
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
chart is 20%, then for in-network providers your co-insurance would be 20% of the network rate.
Co-payments are xed dollar amounts of covered service expenses to be paid by the enrollee. Co-payments
apply per visit/admission/occurrence. If the usual, reasonable, and customary charge is less than the co-
payment, then the co-payment is usual, reasonable, and customary charge. Please note that xed dollar
co-payments do not apply toward your annual deductible. Co-payments accumulate towards annual
member out-of-pocket annual maximums.
Lifetime and Annual Maximum Dollar Benet Amounts
Lifetime maximum benets are the maximum dollar amount of covered Plan benets for certain categories
of services that will be paid on behalf of each Member by the Plan in the Member’s lifetime while covered by
the Plan. Annual maximum benets are the maximum amount of covered Plan benets for certain categories
of services that will be paid on behalf of each Member by the Plan in the Plan Year while covered by the Plan.
Examples of services that are subject to annual maximums are certain dental and vision benets.
Lifetime and annual maximum benets apply only to the specic benets so stated in the Schedules of
Benets, and they do not apply to essential health benets, as dened by Federal regulations under the
Aordable Care Act of 2010.
Please see the Schedules of Benets for the specic benet categories with lifetime and annual dollar limits
and their respective maximum payable benet amounts.

10
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
SCHEDULE OF BENEFITS
NOTE: For all Plan benets, the following apply:
• Co-payments do not accrue toward deductible and apply only to the oce visit charge.
• All other Usual, Reasonable, & Customary (U&C) charges for covered services apply to
deductible and out-of-pocket maximum unless otherwise noted.
• After you pay your deductible, the Plan will pay 100% of the U&C for covered services less your
required co-insurances and co-payments until you reach the Plan out-of-pocket maximum.
• Pre-certication is required for some services, and expenses incurred due to non-compliance
do not accrue toward deductible or out-of-pocket maximum.
• Out-of-network services are only covered in very limited circumstances. Where the below
chart says “not covered” in the Out-of-Network column, services will not be covered without
an approved Unavailable Service Request Form (“USRF”). The services listed in the “Ancillary
Medical Benets” chart are covered both in-network and out-of-network.
• Charges in excess of the Usual, Reasonable, & Customary Charge are member responsibility.
This means if you get care from an out-of-network provider, you may owe amounts in excess
of your co-payment and co-insurance.
• The Schedule of Benets is only a brief summary. You should read the appropriate Plan
sections for additional information about your coverage.
See the Pre-Certication Program section for details regarding services that require .
For employees stationed in the included U.S. territories and their eligible dependents only, out-of-network services
rendered in the included territories will be covered at the in-network cost sharing level. However, using an out-of-
network provider/facility may expose enrollees to balance billing, so using a provider/facility contracted with the
Plan is still advised, if available. (Please call Customer Service at 888-276-4732 for assistance.)
MEDICAL BENEFITS
Benefits
Accelerate Access
Out-of-Network
Usually Not Covered. Even
If Covered, You May Be
Subject To Balance Billing.
MEMBER RESPONSIBILITY
DEDUCTIBLE
• Individual/Family
• Services subject to deductible are marked with (D)
$300 / $600 $600 / 1200
Coverage level
is same as plan
selected, if
applicable.
CO-INSURANCE (AFTER DEDUCTIBLE) PAID BY
MEMBER
20%, unless
otherwise noted
20%, unless
otherwise noted
Out-of-network services
usually not covered. When
covered, co-insurance will
be 20% unless otherwise
noted (and you may be
subject to balance billing).
OUT-OF-POCKET MAXIMUMS
• Individual/Family
$2,750 / $5,500 $5,600 / $11,200
Same, but applies only
when services are covered;
depends on selected plan
option
PREVENTIVE SERVICES 0% 0% Not covered

11
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benefits
Accelerate Access
Out-of-Network
Usually Not Covered. Even
If Covered, You May Be
Subject To Balance Billing.
MEMBER RESPONSIBILITY
FACILITY / AMBULATORY SERVICES
OUTPATIENT SERVICES (INCLUDES SERVICES/
SUPPLIES RECEIVED AT OFFICE VISITS BEYOND
OFFICE VISIT CHARGE)
• Pre-certication required for some outpatient
services (see the “Services Requiring Pre-
Certication” section)
20%
(D)
20%
(D)
Not covered
INPATIENT / OUTPATIENT HOSPITAL STAYS /
MATERNITY DELIVERY
OFFICE / AMBULATORY SURGICAL PROCEDURES
• Pre-certication required for all inpatient
surgeries/stays (except for observation only
and normal delivery in a PPO facility by a PPO
provider)
• Pre-certication required for most outpatient/
ambulatory procedures (see the “Services
Requiring Pre-Certication” section)
20%
(D)
20%
(D)
Not covered
ORGAN/TISSUE TRANSPLANTS
• Pre-certication required
20%
(D)
20%
(D)
Not covered
PHYSICIAN/PROVIDER SERVICES
OFFICE VISIT (APPLIES ONLY TO OFFICE VISIT
CHARGE)
$25 copay $50 copay Not covered
SURGEON FEES AND PHYSICIAN FEES BEYOND
OFFICE VISIT CHARGE
• Pre-certication required for all inpatient
surgeries
• Pre-certication required for most outpatient/
ambulatory procedures (see the “Services
Requiring Pre-Certication” section)
20%
(D)
20%
(D)
Not covered
THERAPEUTIC SERVICES
Physical Therapy
Occupational Therapy
Speech Therapy
• Maximum of 60 visits for any therapeutic
category per Plan Year
• Maximum of 90 visits collectively for all
therapeutic categories per Plan Year
• Pre-certication required after 12 visits per
condition/incident (but this pre-certication only
needs to be done once per condition being
treated, and does not need to be renewed each
year)
20%
(D)
20%
(D)
Not covered
VISION THERAPY
• Maximum of 30 visits per Plan Year
• Pre-certication required
20%
(D)
20%
(D)
Not covered
TELEHEALTH
• Telehealth may be accessed through the
Plan’s telehealth vendor (Amwell) or from a
PPO provider (as long as the PPO provider is
appropriately licensed and has the appropriate
technology to provide and bill for the covered
service)
$0 copay $0 copay
Any provider who is
neither an Amwell
provider nor a PPO
provider is not covered.
MATERNITY & OBSTETRICS 20%
(D)
20%
(D)
Not covered

12
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benefits
Accelerate Access
Out-of-Network
Usually Not Covered. Even
If Covered, You May Be
Subject To Balance Billing.
MEMBER RESPONSIBILITY
EMERGENCY CARE
EMERGENCY ROOM
• Deductible does not apply if not admitted to the hospital*
• If admitted, deductible applies, but co-payment is
waived
• Emergency room visits are only covered when there is
an emergency medical condition
20% after
$100 copay
(D)*
20% after
$100 copay
(D)*
20% after
$100 copay
(D)*
EMERGENT IN-PATIENT HOSPITAL ADMISSION
• Out-of-network services are only covered until the
patient’s medical condition is stable, at which point
the patient must consent to a transfer to an in-network
facility
20%
(D)
20%
(D)
20% until stable;
then not covered
(D)
AMBULANCE SERVICES
• Pre-certication required for nonemergency ground
transportation and for any air transportation (unless
the utilization review manager determines that ground
transportation would have endangered the life of the
enrollee)
20%
(D)
20%
(D)
20%
(D)
URGENT CARE CENTERS
• May be paid as either an ofce visit or as an
Emergency room visit according to provider
contract
• Deductible does not apply regardless of how billed
• Facility fees for ofce visits are not paid
$25 – Ofce Visit/
UC POS
$100 + 20% – ER
$50 – Ofce Visit/
UC POS
$100 + 20% – ER
$25 or $50 – Ofce Visit/
UC POS, copay
depends on
selected plan option
$100 + 20% – ER
EQUIPMENT / SUPPLIES
DURABLE MEDICAL EQUIPMENT
• Benets include purchase or rental, not to exceed the
purchase price of the equipment.
• Pre-certication required for any CPM devices/machines
and Dynaplints.
• Pre-certication required for other durable medical
equipment or repair with billed charges of $2,000 or more
• Pre-certication required for any custom orthotics and for
orthotics/prosthetics with billed charges of $2,000 or more
20%
(D)
20%
(D)
Not covered
BREAST PUMP
• Pre-certication required for breast pump expenses of
$2,000 or more
0% 0% 0%
WIG AS A RESULT OF RADIATION, CHEMOTHERAPY,
OR PATHOLOGICAL CHANGE IN THE BODY
• Plan year maximum benet $1,000
20%
(D)
20%
(D)
20%
(D)
MENTAL HEALTH / SUBSTANCE ABUSE
MENTAL HEALTH COUNSELING SESSIONS
$25 $50
$25 or $50, copay depends
on selected plan option
MENTAL HEALTH OUTPATIENT SERVICES / PARTIAL
HOSPITALIZATION
• Pre -certication required for intensive outpatient
programs and some other outpatient services (see the
“Services Requiring Pre-Certication” section).
• Pre-certication required for partial hospitalization.
20%
(D)
20%
(D)
Not covered
MENTAL HEALTH INPATIENT SERVICES
• Pre-certication required
20%
(D)
20%
(D)
Not covered
RESIDENTIAL CARE AND TREATMENT
• Pre-certication required
20%
(D)
20%
(D)
Not covered

13
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benefits
Accelerate Access
Out-of-Network
Usually Not Covered. Even
If Covered, You May Be
Subject To Balance Billing.
MEMBER RESPONSIBILITY
SUBSTANCE ABUSE/CHEMICAL DEPENDENCY
COUNSELING SESSIONS $25 $50
$25 or $50, copay,
depends on selected
plan option
SUBSTANCE ABUSE/CHEMICAL DEPENDENCY
OUTPATIENT SERVICES
• Pre-certication required for intensive outpatient
programs and some other outpatient services (see the
“Services Requiring Pre-Certication” section)
20%
(D)
20%
(D)
Not covered
SUBSTANCE ABUSE/CHEMICAL DEPENDENCY
INPATIENT TREATMENT
• Pre-certication required
20%
(D)
20%
(D)
Not covered
TELEHEALTH
• Telehealth counseling sessions for mental health
and substance abuse/chemical dependency may
be accessed through the Plan’s telehealth vendor
(Amwell) or from a PPO provider or an out-of-
network provider (as long as the professional
provider is appropriately licensed and has the
appropriate technology to provide and bill for the
covered service)
$0 copay $0 copay $0 copay
OTHER SERVICES
HEARING CARE PROFESSIONAL TESTING/
SCREENING
20%
(D)
20%
(D)
Not covered
HOME HEALTH CARE
• Maximum of 120 visits per Plan Year
• Pre-certication required
• Home health care plan submission required
20%
(D)
20%
(D)
Not covered
SKILLED NURSING FACILITY
• Pre-certication required
20%
(D)
20%
(D)
Not covered
HOSPICE CARE
• Pre-certication required
• Deductible does not apply
0% 0%
0%, but only covered
with approval from the
plan administrator via a
completed Unavailable
Services Request Form
OUTPATIENT DIABETES SELF-MANAGEMENT
TRAINING (DSMT)
• Up to 10 hours (1 hour private and 9 hours group)
training from a certied DSMT provider in the rst Plan
Year and then up to 2 hours of follow-up training in
subsequent Plan Years
0% 0% 0%
NUTRITIONAL COUNSELING
• Five visit annual limit (additional visits may be
authorized by the utilization review manager)
$0 copay $10 copay
Same, depends on
selected plan option
UNAVAILABLE SERVICES
UNAVAILABLE SERVICES
• Only covered with approved Unavailable Service
Request Form
• Deductible applies if it would apply to the same service if
rendered in-network*
N/A N/A
20% if approved;
otherwise not covered
(D)*
COST SHARING WILL BE WAIVED FOR COVID-19 TESTING AND TREATMENT,
SUBJECT TO THE CONDITIONS IN APPENDIX E

14
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
ANCILLARY MEDICAL BENEFITS
Benefits
Accelerate Access
MEMBER RESPONSIBILITY
(Deductible does not apply)
ALTERNATIVE THERAPIES
For Accelerate Plan, benets are bundled and have a collective limit of 45 alternative therapy visits per Plan Year, with no single therapy
category to exceed 30 visits per Plan Year. For Access Plan, only Chiropractic Services are covered and there is a maximum of 30 visits
per Plan Year.
CHIROPRACTIC SERVICES
• Does not apply to Plan Year deductible or out-of-pocket maximum
20% 50%
ACUPUNCTURE THERAPY
• Does not apply to Plan Year deductible or out-of-pocket maximum
• No acupuncture benets for enrollees under age 18
50% Not covered
MASSAGE THERAPY
• Maximum allowable charge is $90 per visit
• Does not apply to Plan Year deductible or out-of-pocket maximum
• No massage therapy benets for enrollees under age 18
50% Not covered
REFRACTIVE EYE SURGERY
• Lifetime maximum payable benet of $2,400
• Does not apply to Plan Year deductible or out-of-pocket maximum
20% 50%
HEARING AIDS
• Plan Year annual maximum payable benet of $3,200
• Does not apply to Plan Year deductible or out-of-pocket maximum
20% 20%
INFERTILITY TREATMENT
• Lifetime maximum benet $16,000
• Does not apply to Plan Year deductible or out-of-pocket maximum
20% 50%
LIFESTYLE PROGRAMS
• 1 completed session/program per Plan Year
• Physician prescription required with claim submission
• Member will be reimbursed upon producing a receipt for covered service
• Does not apply to Plan Year deductible or out-of-pocket maximum
CHIP (Complete Health Improvement Program)
WEIGHT WATCHERS – GROUP MEETINGS ONLY
0% with proof of
80% completion
Only CHIP is covered
(with 0% member cost-
sharing with proof of
80% completion)
No other lifestyle
programs are covered.

15
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
DENTAL BENEFITS – ACCELERATE PLAN
Benefits
In-Network Out-of-Network
MEMBER RESPONSIBILITY
PLAN YEAR DEDUCTIBLE
• Individual/Family
• Deductibles accumulate separately for in-network and out-of-network services.
$100 / $300 $150 / $450
CO-INSURANCE (AFTER DEDUCTIBLE) 20% 25%
ANNUAL MAXIMUM PAYABLE BENEFIT PER PLAN YEAR
• Individual/Family
$2,500 / $7,500
DENTAL CARE
PREVENTIVE CARE
• Deductible does not apply
• Does apply to Plan Year annual maximum payable benet, except for
pediatric (under age 19) preventive dental care
0% 0%
DENTAL CARE
RESTORATIVE CARE
• Applies to correlating Plan Year deductible
20% 25%
ORTHODONTIC CARE
• $2,300 maximum lifetime payable
• Eligible up to age 26 (through age 25)
50%
VISION BENEFITS – ACCELERATE PLAN
Benefits
NO NETWORK REQUIRED
MEMBER RESPONSIBILITY
VISION CARE
• No deductible
• Plan Year annual maximum payable benet $450 per member
• Annual maximum payable does not apply to pediatric (under age 19) annual
eye examination and one pair of standard, clear-lens, prescription glasses per
Plan Year
20%

16
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
PRESCRIPTION BENEFITS – ACCELERATE PLAN
Prescription Drug
Out-of-Pocket Maximums
Individual/Family
$1,250 / $2,500
Prescription co-payment responsibility*
RETAIL – 30 DAY SUPPLY MAIL ORDER – 90 DAY SUPPLY
(via Walgreen’s Smart90, Express Scripts Home Delivery, or
Accredo Specialty Pharmacy)
Generic – Tier 1 $10
Brand (Preferred) – Tier 2 $20
Non-Formulary – Tier 3 $40
Generic – Tier 1 $20
Brand (Preferred) – Tier 2 $40
Non-Formulary – Tier 3 $80
• This benet only covers services/supplies received from Express Scripts (ESI) or from a pharmacy
contracted with ESI
• Brand (also known as “preferred” or “formulary”) drugs can be obtained from ESI or from a pharmacy
contracted with ESI
• Prescription co-payments apply to the prescription benet out-of-pocket maximum
• Penalties for non-compliance do not apply toward Plan Year out-of-pocket maximum
• The Plan pays 100% (and Members pay $0) for preventive prescription drugs received from ESI
or from a pharmacy contracted with ESI (as described in the section of this document entitled
PREVENTIVE PRESCRIPTION DRUGS)
Out-of-pocket for prescription benets will be tracked by Express Scripts. Your pharmacy will be notied if you
reach the Plan Year out-of-pocket maximum.
Specialty Drugs
Specialty drugs can only be lled via mail order through Accredo Specialty Pharmacy (see www.accredo.
com for details). For most specialty drugs, the co-payments listed in the chart above will apply (but see the
SaveonSP Specialty Drugs Program section below for exceptions). Certain infusion or injectable specialty
drugs are available only through the Medical Channel Management Program (see the Benets Description –
Prescription Drugs chapter for details).
SaveonSP Specialty Drugs Program
A list of SaveonSP Specialty Drugs may be found at www.saveonsp.com/adventistrisk
Co-payments for these drugs will uctuate depending on the amount of drug manufacturer assistance that is
available. However, if you sign up for the SaveonSP Program, your
If you do not sign up for the SaveonSP Program, then you will not have your out-of-pocket cost set by the
Plan at $0, you will have to pay a high co-payment for the drug (which is eligible for assistance from the drug
manufacturer), and any amount you pay will not apply to your Plan deductible or your Plan prescription drug
out-of-pocket maximum (because drugs eligible for the SaveonSP Program are not considered ACA essential
health benets).

17
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
DENTAL BENEFITS – ACCESS PLAN
Benefits
In-Network Out-of-Network
MEMBER RESPONSIBILITY
PLAN YEAR DEDUCTIBLE
• Individual/Family
• Deductibles accumulate separately for in-network and out-of-network services.
$250 / $750 $500 / $1,500
CO-INSURANCE (AFTER DEDUCTIBLE) 20% 50%
ANNUAL MAXIMUM PAYABLE BENEFIT PER PLAN YEAR
• Individual/Family
$2,500 / $7,500
DENTAL CARE
PREVENTIVE CARE
• Does not apply to Plan Year deductible
• Does apply to Plan Year annual maximum payable benet, except for pediat-
ric (under age 19) preventive dental care
0% 0%
DENTAL CARE
RESTORATIVE CARE
• Applies to correlating Plan Year deductible
20% 50%
ORTHODONTIC CARE
• $2,300 maximum lifetime payable
• Eligible up to age 26 (through age 25)
50%
* For employees (and their dependents) stationed in the included U.S. territories, “in-network” includes all dental
professional providers rendering services within the scope of their license within the included territories.
VISION BENEFITS – ACCESS PLAN
Benefits
NO NETWORK REQUIRED
MEMBER RESPONSIBILITY
VISION CARE
• No deductible
• Plan Year annual maximum payable benet $225 per member
• Annual maximum payable does not apply to pediatric (under age 19) annual
eye examination and one pair of standard, clear-lens, prescription glasses per
Plan Year
20%

18
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
PRESCRIPTION BENEFITS – ACCESS PLAN
Prescription Drug
Out-of-Pocket Maximums
Individual/Family
$1,550 / $3,100
Prescription co-payment responsibility*
RETAIL – 30 DAY SUPPLY MAIL ORDER – 90 DAY SUPPLY
(via Walgreen’s Smart90, Express Scripts Home Delivery, or
Accredo Specialty Pharmacy)
Generic – Tier 1 $10
Brand (Preferred) – Tier 2 $50
Non-Formulary – Tier 3 $100
Generic – Tier 1 $20
Brand (Preferred) – Tier 2 $100
Non-Formulary – Tier 3 $200
• This benet only covers services/supplies received from Express Scripts (ESI) or from a pharmacy
contracted with ESI
• Brand (also known as “preferred” or “formulary”) drugs can be obtained from ESI or from a pharmacy
contracted with ESI
• Prescription co-payments apply to the prescription benet out-of-pocket maximum
• Penalties for non-compliance do not apply toward Plan Year out-of-pocket maximum
• The Plan pays 100% (and Members pay $0) for preventive prescription drugs received from ESI
or from a pharmacy contracted with ESI (as described in the section of this document entitled
PREVENTIVE PRESCRIPTION DRUGS)
• See below for co-payments for certain drugs oered through the SaveonSP Specialty Drugs Program
(not applicable to employees stationed in the U.S. territories and their dependents; co-payments in
the chart above will apply to such enrollees)
• The Walgreens Smart90 retail program and SaveonSP Program are not available for employees
stationed in the U.S. territories (and their dependents)
• Mail order through the Accredo Specialty Pharmacy and use of the Medical Channel Management
Program are not required for employees stationed in the U.S. territories (and their dependents)
Out-of-pocket for prescription benets will be tracked by Express Scripts. Your pharmacy will be notied if you
reach the Plan Year out-of-pocket maximum.
Specialty Drugs
Specialty drugs can only be lled via mail order through Accredo Specialty Pharmacy (see www.accredo.
com for details). For most specialty drugs, the co-payments listed in the chart above will apply (but see the
SaveonSP Specialty Drugs Program section below for exceptions). Certain infusion or injectable specialty
drugs are available only through the Medical Channel Management Program (see the Benets Description –
Prescription Drugs chapter for details).
SaveonSP Specialty Drugs Program
A list of SaveonSP Specialty Drugs may be found at www.saveonsp.com/adventistrisk
Co-payments for these drugs will uctuate depending on the amount of drug manufacturer assistance that
is available. However, if you sign up for the SaveonSP Program, your cost will be set by the
at $0 and you will not be required to pay anything for the drug.
If you do not sign up for the SaveonSP Program, then you will not have your out-of-pocket cost set by the
Plan at $0, you will have to pay a high co-payment for the drug (which is eligible for assistance from the drug
manufacturer), and any amount you pay will not apply to your Plan deductible or your Plan prescription drug
out-of-pocket maximum (because drugs eligible for the SaveonSP Program are not considered ACA essential
health benets).

19
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Denitions
The following are denitions of some important terms used in this SPD. Wherever used in this SPD, unless the
context provides otherwise, whether italicized, highlighted, capitalized, or not, the terms have the meaning
set forth in this section.
means The Patient Protection and Aordable Care Act (PPACA) – also known as the
Aordable Care Act or ACA.
means as follows: (1) If you are an ACA ongoing employee, you will be an ACA full-
time employee for the plan year if your hours of service during the applicable standard measurement period
when divided by 12 are equal to or greater than 130. (2) If you are an ACA new variable-hour employee or
an ACA new part-time employee, you will be an ACA full-time employee for your initial stability period, if your
hours of service during your initial measurement period were equal to or greater than 130 hours per month.
This denition applies to all employees, including employees who are classied by their human resources
department as either temporary or per diem.
means an employee who has been continuously employed for at least one complete
standard measurement period.
means a new employee whom, based on the facts and circumstances on
the employee’s rst day of active employment, the employer reasonably expects to be employed by that
participating employer on average less than 130 hours of service per month during the employee’s initial
measurement period.
means a new employee for whom, based on the facts and circumstances
on the employee’s rst day of active employment, the employer cannot determine whether the employee is
reasonably expected to be employed by that participating employer on average at least 130 hours of service
per month during the initial measurement period because the employee’s hours of service are variable or
otherwise uncertain.
. You are considered to be actively at work when performing in the
customary manner all of the regular duties of your occupation with a participating employer, either at one
of the participating employer’s regular places of business or at some location to which the participating
employer’s business requires you to travel to perform your regular duties or other duties assigned by your
participating employer. You are also considered to be actively at work on each day of a regular paid vacation
or non-working day but only if you are performing in the customary manner all of the regular duties of your
occupation with the participating employer on the immediately preceding regularly scheduled work day. You
are also considered to be actively at work if you are absent from work due to your injury, illness, disability or
other medical condition. However, if coverage under the Plan is available from your rst day of employment,
you must actually start work in order for coverage to begin.
is the name of the delegated medical necessity pre-certication
utilization review manager for non-prescription drug benets for the Plan. Adventist Health Benets
Administration also handles non-prescription drug appeals of adverse benet determinations involving medical
judgment.
Adventist Health Benets Administration
2625 SE 98th Ave.
Portland, OR 97266
Phone: (888) 276-4732
Fax: (503) 261-6741

20
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
. An adverse benet determination is any of the following (i) a denial, reduction,
or termination of a Plan benet, (ii) a failure to provide or make payment (in whole or in part) for a Plan benet,
or (iii) a rescission of coverage (whether or not the rescission has an adverse eect on any particular Plan
benet at the time of the rescission).
are support services provided to a patient in the course of care. They include such services
as laboratory and radiology.
means any leave of absence that is approved by your employer. Approved leave includes
summer vacation and other similar vacation periods for an employee working for a participating employer who
is a school, college, university, or other educational institution, until such employee is terminated.
means (i) an individual named on a completed Appointment of Authorized
Representative form that is submitted by a claimant, (ii) a physician or professional provider with knowledge
of the claimant’s medical condition (e.g., the claimant’s treating physician) or the facility where the claimant is/
was treated, unless the claimant provides specic written direction otherwise, and (iii) an employee for his or
her covered dependent who is under age 18. See the Claims Procedures chapter for more information.
means (1) a natural child; (2) a step-child (i.e., the child of an employee’s spouse); (3) a child
who has been legally adopted by the employee or the employee’s spouse, or placed for adoption with the
employee or the employee’s spouse, by either a court of competent jurisdiction or appropriate state agency;
(4) an individual for whom an employee or the employee’s spouse has been awarded legal guardianship by a
court; and (5) an individual for whom the employee is required to provide coverage pursuant to the terms of
a Qualied Medical Child Support Order (“QMCSO”) as dened in applicable federal law originally enacted as
part of the Child Support Performance and Incentives Act of 1998 [PL 105-200, 7/16/1998; Section 401(f)(1)].
means any request for a Plan benet or benets made in accordance with the Claims Procedures. A
communication regarding benets that is not made in accordance with the procedures will not be treated as
a claim.
is an individual who has made a claim in accordance with the Claims Procedures.
means the plan year or portion thereof.
means the Center for Medicare and Medicaid Services, the agency that administers Medicare, Medicaid,
and Child Health Insurance Program.
means the shared percentage cost of covered services that the enrollee pays.
means the xed dollar amounts of covered services to be paid by the enrollee.
means a medical condition.
means services or supplies which are not otherwise benets of the Plan, but
which plan administrator determines, in its sole discretion, to be medically necessary and cost eective.
means an eligible dependent of a covered employee of a participating employer whose
application has been accepted by the plan administrator and who has elected to cover such eligible
dependent.
means an eligible employee of a participating employer who is covered by this Plan
following acceptance by the plan administrator of that person’s application. For new employees, coverage
is contingent upon enrolling within 30 days (or a longer period if required by state law) of the rst day the
employee is eligible to participate in the Plan. (See Waiting Period and Eective Date section.) See the Open
Enrollment section below for the rules applicable to ongoing employees beginning and maintaining coverage.
For both new employees and ongoing employees, if you do not timely enroll in accordance with this SPD, you
will be required to wait until the next open enrollment period unless either the Change in Status section or the

21
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
HIPAA Special Enrollment Rights section applies.
is a service or supply that is specically described as a benet of this Plan.
means care that helps a person conduct such common activities as bathing, eating, dressing
or getting in and out of bed. It is care that can be provided by people without medical or paramedical
certication or license. Custodial care also includes care that is primarily for the purpose of separating a
patient from others, or for preventing a patient from harming himself or herself. Custodial care and services
are services and supplies that are furnished mainly to train or assist a person in personal hygiene and
other activities of daily living rather than to provide therapeutic treatment. Activities of daily living includes
such things as bathing, feeding, dressing, walking, and taking oral medicines and any other services which
can safely and adequately be provided by persons without the technical skills of a nurse or healthcare
professional. Such care is considered to be custodial regardless of who recommends, provides or directs the
care, where the care is provided and whether or not the individual family member can be or is being trained
to care for him or herself. The Plan also considers any care or services to be custodial if they are or would be
considered custodial for Medicare purposes.
, when used in the Claims Procedures, means calendar day.
means a device specially designed to be placed surgically within or on the mandibular
or maxillary bone as a means of providing for dental replacement; endosteal (endosseous); eposteal
(subperiosteal); transosteal (transosseous).
means a judgment (i) of dissolution or annulment of a marriage or (ii) for legal separation
of the spouses in a marriage as ordered by a court of competent jurisdiction. The eective date of a divorce
for purposes of the Plan is the later of the divorce or separation eective date set by the court in its divorce/
separation order or the date on which the order is entered.
is equipment and related supplies which the Plan determines (1) are able to
stand repeated use, and be of a type that could normally be rented and used by successive patients, (2)
are used primarily and customarily to serve a medical purpose (e.g., not items like humidiers, exercise
equipment, gel pads, water mattresses, heat lamps, etc.), (3) are not generally useful to a person in the
absence of an injury or illness, (4) are appropriate for home use, and (5) meet the guidelines used by the CMS.
Examples of durable medical equipment include a wheelchair, a hospital-type bed and oxygen tanks.
means your spouse and/or child who is eligible for coverage under this medical Plan. The
eligibility provisions are set forth in the Eligibility, Enrollment and End of Coverage chapter.
means a literature evangelist who meets the qualications required by his or her
participating employer according to North American Division Working Policy Section FP 70.
means a seminary student who meets the qualications required by his or her
participating employer.
means a medical condition that manifests itself by acute symptoms of sucient
severity, including severe pain, that a prudent layperson possessing an average knowledge of health and
medicine would reasonably expect that failure to receive immediate medical attention would (i) place the
health of the individual (or, with respect to a pregnant woman, the health of the woman or her unborn child)
in serious jeopardy, (ii) cause serious impairment to bodily functions or (iii) cause serious dysfunction of any
bodily organ or part.
means, as provided in 26 CFR §54.9815-2719A, or any successor law or regulation, with
respect to an emergency medical condition, a medical screening examination which is within the capability
of the emergency department of a hospital, including ancillary services routinely available to the emergency
department to evaluate such emergency medical condition, and such further medical examination and
treatment, to the extent they are within the capabilities of the sta and facilities available at the hospital, as
are required to stabilize the patient (including in-patient services). For purposes of this section, the term “to

22
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
stabilize,” with respect to an emergency medical condition, means to provide such medical treatment of the
condition as may be necessary to assure, within reasonable medical probability, that no material deterioration
of the condition is likely to result from or occur during the transfer of the individual from a facility, or, with
respect to a pregnant woman who is having contractions, to deliver (including the placenta).
means an individual who is engaged by the employer to perform services for the employer in a
relationship that the employer characterizes as an employment relationship. The following individuals are not
employees:
• Individuals working for the employer under a lease arrangement.
• Individuals who are engaged by the employer to perform services for the employer in a relationship
that the employer characterizes as other than an employment relationship. For example, individuals
engaged to perform services in a relationship which the employer characterizes as that of an
“independent contractor” with respect to the employer.
• Any individual described in this denition as not an employee is not eligible to participate in the Plan
even if a determination is made by the Internal Revenue Service, the United States Department of
Labor, another governmental agency, a court or other tribunal that the individual is an employee of
the employer. An individual who has not met the denition of employee shall become an employee
eligible to participate in the Plan (subject the individual’s meeting all other eligibility requirements
of the Plan) eective on the date the employer characterizes the individual as an employee in the
employer’s employment records.
means the contribution you must make for coverage under the Plan. This
amount is separate from the deductible and any co-payments or co-insurance you are required to pay for
covered services. See the Employee-Share Contribution chapter for further discussion.
means the participating employer at which you work.
(enrolled, enrolling, enrollment) means to submit, and be accepted by the plan administrator, a complete
and signed application for Plan coverage in accordance with the rules in the Eligibility, Enrollment and End of
Coverage chapter.
means a covered employee or a covered dependent.
means a hospital, hospice facility, skilled nursing facility, or mental health or substance abuse
residential facility.
means the Plan’s adverse benet determination made after
considering the nal internal appeal of a denial of a claim.
means an employee who is classied by his or her employer as a full-time, exempt or
non-exempt, regular employee either working in his or her position or on an approved leave of absence. A
full-time employee also includes regular employees working for two or more participating employers whose
total number of hours equals or exceeds the number of hours per week required to be considered full time.
(Such employees will enroll through one participating employer, but the participating employers will share
the employer portion of the cost of coverage.) The nal determination of whether an employee is a full-time
employee under the terms of the Plan will be made by the plan administrator.
means information about genes, gene products, and inherited characteristics that
may derive from the individual or a family member. This includes information regarding carrier status and
information derived from laboratory tests identify mutations in specic genes or chromosomes, physical
medical examinations, family histories, and direct analysis of genes or chromosomes.
means a program licensed and operated according to the law, which is approved by the
attending physician to provide palliative, supportive and other related care in the home for a covered person

23
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
diagnosed as terminally ill.
a public or private organization, licensed and operated according to the law, primarily
engaged in providing palliative, supportive, and other related care for a covered person diagnosed as
terminally ill. The facility must have an interdisciplinary medical team consisting of at least one physician, one
registered nurse, one social worker, one volunteer and a volunteer program. A hospice facility is not a facility or
part thereof which is primarily a place for rest, custodial care, the aged, drug addicts, alcoholics or a hotel or
similar institution.
means a facility that is licensed as an acute care general hospital and provides in-patient surgical
and medical care to persons who are acutely ill. Additionally, the facility’s services must be under the
supervision of a sta of licensed physicians and must include 24-hour-a-day nursing service by registered
nurses. Facilities that are primarily rest, old age or convalescent homes are not considered to be hospitals.
Facilities operated by agencies of the federal government are not considered hospitals. However, the Plan will
cover expenses incurred in facilities operated by the federal government where benet payment is mandated
by law.
means each hour for which you are paid, or entitled to payment, for the performance of duties
for your employer, any entity that is treated as a single employer with your employer under Internal Revenue
Code section 414(b), (c), (m), or (o), or any other participating employer; and each hour for which you are paid,
or entitled to payment by your employer, any entity that is treated as a single employer with your employer
under Internal Revenue Code section 414(b), (c), (m), or (o), or any other participating employer for a period of
time during which no duties are performed due to vacation, holiday, illness, incapacity (including disability),
layo, jury duty, military duty or leave of absence. Your hours of service during an unpaid leave of absence will
be calculated in accordance with 26 CFR § 54.4980H-3(d)(6)(i). The term “hour of service” will be interpreted in
a manner consistent with Code Section 4980H and its regulations.
means a disease or bodily disorder.
means a material inserted or grafted into tissue.
means any request for Plan benets that is not made in accordance with the Claims
Procedures.
or means the United States territories covered
by this Plan, which are Guam and the Northern Mariana Islands.
means an entity that conducts independent external reviews of
adverse benet determinations in accordance with the Patient Protection and Aordable Care Act of 2010 and
associated regulations and is accredited by URAC or a similar nationally-recognized accrediting organization
to conduct external review.
is the administration of uids, nutrients or medications by means of a catheter or needle into
a vein. Infusion therapy is not the same as an injection.
(except where otherwise dened by your participating employer) means the
2-calendar-month period beginning immediately after an ACA new variable-hour employee’s or ACA new part-
time employee’s initial measurement period. The initial administrative period also includes any days from an
ACA new variable-hour employee’s or ACA new part-time employee’s rst day of active employment to the start
of the employee’s initial measurement period.
(except where otherwise dened by your participating employer) means the
11-calendar-month period beginning on the rst day of the month coincident with or following an ACA new
variable-hour employee’s or ACA new part-time employee’s rst day of active employment.
(except where otherwise dened by your participating employer) means the 12-month
period beginning immediately after an ACA new variable-hour employee’s or ACA new part-time employee’s

24
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
initial administrative period.
means a personal bodily injury to you or your covered dependent.
- The terms network and in-network refer to PPO providers and PPO facilities.
means a hospital, hospice facility, skilled nursing facility, or mental health or substance
abuse residential facility that is a PPO facility.
means a physician or professional provider who is a PPO provider.
means any condition of an enrollee resulting from illness, injury (whether or not the injury is
accidental), pregnancy or congenital malformation. However, genetic information is not a medical condition.
– Determinations involving medical judgment include, but are not limited to, those based
on the Plan’s requirements for medical necessity, appropriateness, health care setting, level of care, or
eectiveness of a covered benet; the Plan’s determination that a treatment is experimental or investigational;
whether an enrollee is entitled to a reasonable alternative standard for a reward under a wellness program;
or whether the Plan is complying with the nonquantitative treatment limitation provisions of Code Section
9812 and Regulation Section 54.9812 (which generally require, among other things, parity in the application of
medical management techniques).
refers to obtaining the utilization review manager’s determination in
advance that proposed medical services requiring pre-certication are medically necessary, appropriate, and
neither Experimental nor Investigational Procedures as dened in the Limitations and Exclusions chapter.
means those services and supplies that are required for diagnosis or
treatment of illness or injury and which, in the judgment of the utilization review manager, are:
• Appropriate and consistent with the symptoms or diagnosis of the enrollee’s condition.
• Appropriate with regard to standards of good medical practice in the area in which they are provided
as supported by peer reviewed medical literature.
• Not primarily for the convenience of the enrollee or a physician or provider of services or supplies.
• The least costly of the alternative supplies or levels of service that can be safely provided to the
enrollee. This means, for example, that care rendered in a hospital inpatient setting is not medically
necessary if it could have been provided in a less expensive setting, such as a skilled nursing facility,
or by a nurse in the patient’s home without harm to the patient.
• Likely to enable the enrollee to make reasonable progress in treatment.
Please Note: The fact that or provider prescribes, orders, recommends or approves a
service or supply does not, of itself, make the service or a .
Member means enrollee.
for the purposes of this Plan means those conditions listed in the “Diagnostic and
Statistical Manual of Mental Disorders Fifth Edition” (DSM-5), or any successor volumes, except as stated
herein, and no other conditions. Mental health conditions include Severe Mental Illness and Serious Emotional
Disturbances of a child but do not include any services related to the following:
(i) Diagnosis or treatment of conditions represented by V codes in the DSM-5 (i.e., diagnoses related to
family problems, illegal behavior, low income, loneliness, abuse, neglect, deployment, imprisonment,
discrimination, lifestyle, etc.), or any successor volumes.

25
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
(ii) Diagnosis or the treatment of any conditions with the following ICD-10 Classication of Mental and
Behavioral Disorders codes: F06.0, F06.8, F60.9, F65.4, F65.1, F65.2, F64.2, R37, F52.0, F52.21, F528,
F52.31, F52.32, F52.4, F52.6, F52.1, F65.0, F65.3, F65.51, F65.52, F64.1, F65.81, F66, F65.9, F98.4, F63.3,
R45.1, F91.9, F63.9, F63.0, F63.2, F63.1, F63.81, F81.0, F81.2, F81.81, F81.89, F80.89, F54.
means services provided to treat a mental health condition.
– The terms network and in-network refer to PPO providers and PPO facilities.
– The network rate is the negotiated amount for each service/supply that is pre-contracted and
agreed upon between the PPO Network and its participating providers and facilities. A network rate is also
known as a “negotiated rate.”
means an approved leave that is not a protected
leave. See the Reinstatement of Coverage and Special Situations, Extension of Coverage sections in the
Eligibility, Enrollment and End of Coverage chapter for special rules pertaining to coverage during and
following a non-protected leave.
refers to any health care facility that is not an in-network facility. With the exception
of emergency services, urgent care, and approved Unavailable Service Request Form services, care received
at out-of-network facilities is not covered.
refers to physicians and professional providers that are not in-network providers.
Except for the following exceptions, services received from out-of-network providers are not covered:
(i) Emergency services including emergency ground ambulance transportation, and including
emergency air ambulance transportation (but only with pre-certication or when ground transportation
would endanger the life of the member),
(ii) Urgent care,
(iii) Approved Unavailable Service Request Form (“USRF”) services, and
(iv) Service received at an in-network facility that is prescribed by a PPO provider (in which case the
service will be covered at the PPO level even if performed by an out-of-network provider).
(v) Service received in an included territory by an employee stationed in an included territory (or the
employee’s eligible dependent).
The Plan recognizes at times the Medical/Dental PPO Networks may not have PPO Providers accessible
to members that deliver needed medical/dental care. There are times members through the Unavailable
Services Request Form (USRF) Pre-Certication process will receive approval for medical services from
an Out-of-Network Provider or Out-of-Network Facility. Similarly, the USRF process may be used to
obtain approval to use an Out-of-Network dental provider with In-Network cost sharing-requirements.
While the following is not an exhaustive list, these are guidelines the Plan will use in determining
approval of USRF.
• Medical Necessity
• Availability of providers who are in the PPO relative to the members home or work address
o For rural areas the distances of Medical/Dental PPO Network Providers within
approximately 25 miles, or approximately 35-40 minutes driving.
o For metropolitan areas the distance of Medical/Dental PPO Network Providers within
approximately 10 miles or approximately 35-40 minutes of driving.
means surgery that does not require an inpatient admission or overnight stay.
means an employee who is not a full-time employee. The nal determination of whether
an employee is a part-time employee will be made by the plan administrator.

26
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
means the Seventh-day Adventist Organizations, inclusive of the General Conference
of Seventh-day Adventists and its subsidiaries and aliates, that participate in the Plan. All participating
employers are required to be listed in the most recent version of the Adventist Organizational Directory or the
most recent version of the Seventh-day Adventist Yearbook. Participating employer entities are added and
subtracted from time-to-time by amendment. If you are unsure as to whether your employer is a participating
employer, please call the plan administrator at (888) 276-4732.
means a doctor of medicine or osteopathy.
means this Healthcare Assistance Plan aka Ascend to Wholeness Plans for Employees of the Seventh-day
Adventist Church Organizations based in the United States, Guam, and the Northern Mariana Islands.
means the North American Division of Seventh-day Adventists. The plan administrator
shall have full discretionary power to administer the Plan and to interpret, construe, and apply all of its
provisions, determine eligibility, and adjudicate claims as provided herein. The plan administrator may
delegate any of these duties as it deems reasonable and appropriate, and the plan administrator has
delegated its plan administrative duties to Adventist Risk Management (“ARM”) and has authorized ARM to
further delegate plan administrative duties to other entities. In administering the Plan, the plan administrator
(including its delegate, ARM, and ARM’s delegates) shall be guided by and adhere to the teachings and tenets
of the Seventh-day Adventist Church. When the term “plan administrator” is used in this Plan, it generally
refers to ARM in its role as the delegate of the North American Division of Seventh-day Adventists.
is the North American Division of Seventh-day Adventists; however, for the purposes of both (i)
the privacy obligations under the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”), and (ii)
Plan nancial liability, your participating employer is the plan sponsor for its piece of the Plan.
means a calendar year (January 1 through December 31) or portion thereof. See denition for Claim
Determination Period.
means a hospital, hospice facility, skilled nursing facility, or mental health or substance abuse
residential facility that is a participating provider in the PPO Network.
means the preferred provider networks arranged by Aetna Signature Administrators PPO for
medical services and Aetna Dental Administrators for your Plan (for a list of contracted providers and facilities,
please go to www.aetna.com/asa or call 888-276-4732). (Employees of Oakwood University refer to Appendix
C for PPO Network information.) For employees (and their dependents) stationed in the included territories (and
for other enrollees receiving emergency services in the included territories), the term “PPO Network” includes
providers and facilities with which the Plan has contracted directly to provide covered services to Plan
enrollees (for help locating such providers and facilities, please call 888-276-4732 or go to
www.ascendtowholeness.org).
means a physician or professional provider who is in the PPO Network.
refers to obtaining approval
from the utilization review manager prior to the date of service for services that have been ordered by a
physician or professional provider.
means a licensed professional, when providing medically necessary services within
the scope of their license. In all cases, the services must be covered services under this Plan to be eligible for
benets.
means an approved leave during which your employer is required by state or federal law
to continue to oer you health plan coverage for a statutorily specied period of time. A leave is a protected
leave only during the time period during which health plan coverage is statutorily required to be maintained.
See the Reinstatement of Coverage and Special Situations, Extension of Coverage sections in the Eligibility,
Enrollment and End of Coverage chapter for special rules pertaining to coverage during and following
a protected leave. A workers’ compensation leave of absence does not meet the denition of protected

27
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
leave. However, an employee who is o on a workers’ compensation leave is treated exactly the same as an
employee who is o on a comparable non-workers’ compensation leave.
refers to one of the following events:
• Marital Status: Your legal marital status changes for reasons of marriage, death of a spouse, divorce,
legal separation, or annulment.
• Dependents: Your number of eligible dependents changes due to birth, adoption, placement for
adoption, or death of an eligible dependent.
• Employment Status: You or your eligible dependent experience a change in employment status,
including: commencement or termination of employment, a change from part-time to full-time, or
full-time to part-time status, commencement or return from an unpaid leave of absence, or any other
change in employment status that aects benets eligibility.
• Change in Dependent Status: Your dependent satises or ceases to satisfy the eligibility requirements
for coverage.
• Residence: You or your eligible dependent change geographic residence provided that the change in
residence aects your or your eligible dependent’s eligibility for coverage under this Plan or another
plan or policy.
• Change in Coverage of Eligible Dependents. Your eligible dependent is entitled to make a change
to his or her coverage (or the coverage of another of your eligible dependents) under his or her
employer’s plan due to a permitted election change or during his or her plan’s annual enrollment
period, if dierent from the Plan’s annual enrollment period.
• Overall Reduction in Benets: You or your eligible dependent experience a signicant overall reduction
or termination of benets under the Plan or under another employer’s plan, as determined in the sole
discretion of the plan administrator. In general, for a group health plan, a signicant overall reduction
includes a signicant increase in the deductible, co-payment, or out-of-pocket maximum, but does
not include your physician or provider ceasing to be an in-network provider.
• Signicant Reduction in Coverage: Your or your eligible dependent’s coverage under this Plan or
another employer’s plan is signicantly reduced or limited causing you or the eligible dependent
to lose coverage, as determined at the sole discretion of the plan administrator. An example of a
signicant reduction in coverage is if there is a substantial reduction in providers available under your
or your eligible dependent’s elected benet option.
• Signicant Change in Cost: The cost of coverage for you and/or your eligible dependents signicantly
increases or decreases under the Plan or another employer’s plan.
• Addition of Benet Options: A new benet package option or coverage option is added to the Plan or
to another employer’s plan under which you or one of your eligible dependents is covered.
• Medicare or Medicaid Entitlement: You or your eligible dependent gain or lose entitlement for
Medicare or Medicaid.
is temporary relief for the usual family caregiver of a covered Plan member who is receiving pre-
certied hospice care at home so long as the services constitute “medical care” within the meaning of Code
Section 213(d) which can include such things as medication administration, changing dressings, bathing, and
grooming but not general household services, such as doing dishes and laundry.
means Summary Plan Description. See the Welcome chapter.
means your opposite sex lawful spouse under the applicable law of the state in which the

28
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
participating employer facility at which you work is located (or if you are not assigned to a specic facility, then
the state of employer). Some states allow common law marriage, which is a legally recognized marriage that
lacks formal marriage proceedings; spouse does not include a spouse through common law marriage.
(except where otherwise dened by your participating employer) means, for
a given plan year, the period beginning on the rst day of the pay period that includes October 4 of the year
that is two years prior to the plan year and ending on the last day of the pay period that ends before October 4
of the year preceding the plan year. For example, for the 2015 plan year, the standard measurement period is
the period beginning on the rst day of pay period #21 for the year 2013 (which includes October 4, 2013) and
ending on the last day of pay period #20 for the year 2014 (which is the last pay period ending before October
4, 2014).
means assigned to work in a physical geographic location by your participating employer with the
intention that you will work in that physical geographic location for at least six months.
means substance abuse as dened in the most recent version of the Diagnostic and
Statistical Manual, as published by the American Psychological Association. For purposes of this Plan,
substance abuse does not include addiction to, or dependency on, foods, tobacco or tobacco products.
benet provides access to board-certied doctors through the Plan’s contracted vendor, Amwell.
Amwell provides in-network benets for covered services, and their providers are available 24 hours a day
using your phone, tablet, or computer. Telehealth benets are also available through any PPO provider,
and, in the case of mental health services only, out-of-network providers (as long as the PPO provider, or,
in the case of mental health services only, out-of-network provider, is appropriately licensed and has the
appropriate technology to provide and bill for the covered service). A telehealth visit is a substitute for an in-
person oce visit with a provider using electronic information and telecommunications technologies such
as videoconferencing, internet, streaming media, and terrestrial and wireless communications. Telephone
consultations and routine phone calls with your provider (for example, follow-up calls with your doctor to go
over lab test results or to request prescription drug rells) are not telehealth visits and are not a covered service
of the Plan. For more information, go to ascendtowholeness.org.
means a person who has been determined to be disabled by the Social
Security Administration. The Social Security Administration currently denes disability as an illness or injury
expected to result in death or that has lasted or is expected to last for a continuous period of at least 12
months, and makes the individual unable to engage in any employment or occupation, even with training,
education, and experience (or, for children, makes the child unable to substantially engage in any of the
normal activities of children in good health of like age). Physician certication of continued total disability,
based on the Social Security Administration standard, is required upon request from the plan administrator.
Additionally, the plan administrator reserves the right to require at its expense an independent medical,
psychiatric, or psychological evaluation to verify an individual’s continued total disability.
means the provision of immediate, short-term medical care for minor but urgent medical
conditions that do not pose a signicant threat to life or health at the time the services are rendered.
means:
i. For out-of-network providers/facilities, the normal and necessary charges submitted or made for similar
services or supplies provided by other providers of medical or dental services with like experience,
education and training in the same geographical area. The term “geographic area” as it applies to any
particular service, medicine, or supply means a county or such greater area as is necessary to obtain a
statistically representative cross-section of the level of charges.
Determination of the U&C for a medicine, service, or supply shall be made by the U&C contract
administrator, using the 80th percentile of all charges for the same service or supply in the geographic
area based on survey data collected and maintained by the U&C contract administrator (except that
the U&C for anesthesia will be a at rate of $95 per unit in the 2021 plan year). The “U&C contract
administrator” is the entity with which the plan administrator or PPO Network has contracted to provide

29
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
usual and customary rate services and access to usual and customary rate databases.
In the event a claim is received from an out-of-network facility/provider and there is no U&C for the
services provided, the claim will pay at no more than 120% of Medicare.
For unlisted CPT codes ending in “99” for which there is no U&C for the service provided and no
Medicare rate, the U&C will be 50% of billed charges.
In the event a claim is received for emergency services rendered outside of the United States, the
billed charges will be considered the U&C for the services rendered unless the plan administrator
or its delegate determines that the billed charges are unreasonable when compared to the charges
submitted or made for similar services or supplies provided by other providers with like experience,
education and training in the same country.
Notwithstanding the above, if a dierent rate is negotiated between an out-of-network provider/facility
and the plan administrator, the PPO Network, or their delegates, then that negotiated rate will be used
and will be considered the U&C for the services rendered that are subject to such dierent negotiated
rates.
For purposes of emergency services rendered in the United States, if either the median network rate
for an emergency service or the amount that would be paid under Medicare (Part A or B) (the “Medicare
Rate”) for the emergency service is higher than the U&C as determined under this section, then such
higher network rate or Medicare Rate, as applicable, will be the U&C for the emergency service.
ii. For in-network providers, the network rate. If no network rate is in place for the service or supply, the
U&C will be determined as though it was provided by an out-of-network provider.
iii. After hours surcharges in any 24-hour facility are not U&C and will not be covered by this Plan. This
applies to both in-network providers and out-of-network providers.
iv. Note on alternative phraseology: In some Plan materials, the usual, reasonable, & customary
charge may be referred to as the Usual and Customary Charge, the Usual and Customary Rate, the
Reasonable and Customary Charge, the Reasonable and Customary Rate, the UCR, or some other,
similar phrase.
means Adventist Health Benets Administration’s in-
house utilization review department, which is responsible for determining whether requested medical care
is medically necessary. However, for all prescription drug benets, the utilization review manager is Express
Scripts and for dental benets the utilization review manager is Aetna Dental. Adventist Health Benets
Administration also hears non-prescription drug appeals of adverse benet determinations involving medical
judgment.

30
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Eligibility, Enrollment and End of Coverage
ELIGIBILITY FOR THE ACCELERATE AND ACCESS PLAN OPTIONS
Both Plan options encourage active participation in wellness, health coaching and care coordination. For
this purpose, all enrollees age 18 and older are eligible to use the wellness platform (but the wellness
requirements/rewards described below apply only to employees and their spouses).
If you are enrolled in the Plan in 2021, then in order to enroll in the Accelerate option of this Plan for 2022, you
and your enrolled spouse dependent (if applicable) must each earn 10,000 wellness participation points during
the period of September 1, 2020 through July 31, 2021. (Points will be prorated if you initially enroll in this Plan
on April 1, 2021 or later; and the point requirement will be waived if you initially enroll in this Plan on July 1,
2021 or later.) Wellness participation points may be earned by engaging in participatory activities, such as
healthy lifestyle habits (e.g., tracking your calories or water intake), participating in general health education
opportunities via the wellness portal, or obtaining preventive care (e.g., dental cleanings or vaccinations).
You may also earn points in additional ways, such as walking, but this is not required in order to earn enough
points for an incentive or to enroll in the Accelerate option.
Additionally, the following wellness resources are made available to all members and you may earn points for
participating (but participation is not required in order to earn enough points for an incentive or to enroll in the
Accelerate option):
1. Wellness Assessment; You may complete a free online wellness assessment. The online Wellness
Assessment is a secure online tool that you use to provide information about your health and can be
accessed at the Wellness Portal at www.ascendtowholeness.org. After you complete the Wellness
Assessment, you will receive a summary report that identies areas you are doing well in and areas of
potential health risks as well as what you can do to reduce those risks.
2. Biometric Screening; You can complete your free Biometric Screening with a physician and in-
network lab. The condential Biometric Screening will provide you with vital numbers (such as
cholesterol, blood glucose, blood pressure, and more) that you can compare to recommended
healthy guidelines to help determine your risk for disease and chronic health conditions.
You do not need to undergo a wellness assessment or biometric screening in order to enroll in the
Accelerate option. And if you choose to do a wellness assessment or biometric screening, you
will not be required to take any further action based on the results of your wellness assessment or
biometric screening.
Who is Eligible
Full-time employees, eligible literature evangelists, eligible seminary students, and any employee not tting
within these categories who is an ACA full-time employee are eligible to participate in this Plan if based in the
United States or one of its included territories, and will have an eective date of coverage as explained in the
“Waiting Period and Eective Date” section. However, except for any ACA full-time employee, any employee
who is classied by his or her employer’s human resources department as either temporary or per diem is
not eligible to participate in this Plan. The determination of whether you are a full-time employee, part-time
employee, or neither is usually determined initially by your employer, but ultimately the plan administrator
may make a dierent determination. (Some determinations, such as disability determinations, may be made
initially by the plan administrator.)
If it is determined that your status (full-time, part-time, or neither) has changed, your employer will provide
you with a notice of the change in status and the change in status will take eect on the date stated in the

31
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
notice. Review of employee status (full-time, part-time, or neither) will be performed monthly. If you are
miscategorized as not a full-time employee, you will not be treated as an employee or enrollee for purposes
of the Plan until after you enroll in the Plan (even if a court, the IRS, or other administrative agency later
determines that you were miscategorized).
Eligible Dependents
If you are eligible for and elect coverage under the Plan, your eligible dependents may also participate in the
Plan. Eligible dependents include:
• Your unemployed spouse (or your employed spouse if your employer so allows) who is living with you.
A spouse who is not living with you may continue to be covered (1) for up to six months during a trial
separation, (2) if you and your spouse are living at separate locations because of a job, or (3) if you
have a court order to provide coverage for your spouse.
• Your child from birth to attainment of age 26. Children are eligible to participate in the Plan until
the date on which they turn 26 years of age. This maximum child coverage age supersedes any
inconsistent provisions in the Plan.
• Your unmarried child of any age so long as the child is totally disabled, the total disability commenced
before the child reached age 26, and the child is primarily dependent on you for support and
maintenance. In order to obtain coverage for such a child, you must submit evidence of total disability
within 31 days of the child’s 26th birthday.
The term eligible dependent does not include any dependent who is on active full-time military duty in the
armed forces of any country.
The term eligible dependent does not include parents of enrollees regardless of whether the enrollee has
assumed legal guardianship of the parent.
No person may be covered as both an employee and as a dependent, nor can a person be covered as a
dependent of two employees.
You will be required to obtain and provide your employer with a Social Security number for each covered
dependent. The Plan will not pay any claims incurred by a covered dependent unless and until the Social
Security number is provided. There are, however, three exceptions to this rule:
(i) If your dependent is a newborn baby, you will have until the child’s rst birthday to provide the child’s
Social Security number;
(ii) If a child is placed in your care for purposes of adoption, you have one year from that date to provide
the child’s Social Security number; and
(iii) If your dependent does not have a Social Security Number (for example, this might occur because
you are working in the United States on a visa/work permit) or you refuse to disclose the dependent’s
Social Security number to the Plan, you can obtain coverage for the dependent by (i) annually
completing the Center for Medicare and Medicaid Services HICN/SSN form (or any successor form),
and (ii) executing a form wherein you both certify to the Plan that the dependent does not have a
Social Security number or that you are refusing to disclose the dependent’s Social Security number
and agree to indemnify the Plan for any losses sustained due to your inaccurately or incompletely
lling out the HICN/SSN form.
If the plan administrator determines that your separated or divorced spouse or any state child support or
Medicaid agency has obtained a qualied medical child support order (“QMCSO”), and your current plan
oers dependent coverage, you will be required to provide coverage for any child(ren) named in the QMCSO
directed specically at you. A QMCSO directed at your spouse but not at you will not be applicable nor
sucient. If a QMCSO requires that you provide health coverage for your child(ren) and you do not enroll the

32
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
child(ren), your employer must enroll the child(ren) upon application from your separated/divorced spouse, the
state child support agency, or Medicaid agency, and withhold from your pay your share of the cost of such
coverage. Although the Plan does not normally provide dependent-only coverage, dependent-only coverage
is allowed if you are required to provide coverage for one or more child and you are not currently enrolled in
the Plan. You may not drop coverage for the child(ren) unless you submit written evidence to your employer
that the child support order is no longer in eect. The Plan may make benet payments for the child(ren)
covered by a QMCSO directly to the custodial parent or legal guardian of such child(ren).
Waiting Period and Eective Date
New employees have an eective date for coverage to start as of their rst day of employment (unless their
employer has a waiting period, in which case the maximum waiting period is 90 days and the latest date
that coverage would start would be the rst day of the fourth full calendar month following the rst day of
employment). To enroll, an employee must be actively at work and enrollment must be completed no later
than 30 days (or a longer period if required by state law) after this eective date. Coverage for your eligible
dependents begins on the later of when your coverage begins or the rst day an eligible dependent is legally
acquired if properly enrolled.
Depending on your employer’s policy, a shorter waiting period or no waiting period may apply for an employee
who transfers from the employ of another Seventh-day Adventist entity. Please call your new employer’s
human resources department for details. For these purposes, “Seventh-day Adventist entity” means any
participating employer or other United States based entity that is listed in either the most recent version of the
Adventist Organizational Directory or the most recent version of the Seventh-day Adventist Yearbook.
The waiting period may be waived in certain other instances as determined by the plan administrator.
During a waiting period, new employees may be able to elect short-term medical plan coverage at their own
expense. Such employees should contact the human resources oce of their employer. Certain conditions
may apply.
If your status changes to full-time, your employer will provide you with a notice of the change in status and
you will be oered coverage that begins on the date stated in the notice.
If you are determined to be an ACA full-time employee following your initial measurement period, you will be
oered coverage that begins on the rst day of your initial stability period.
Initial Enrollment Requirements
You must enroll within 30 days (or a longer period if required by state law) of the date you are rst eligible
for the Plan. You are rst eligible for the Plan as of the rst day of your employment (if you enroll within the
30-day period) unless your employer has a waiting or probationary period. (The maximum waiting period
is 90 days and the latest your coverage would start would be the rst day of the fourth full calendar month
following your date of hire.)
If you also desire coverage for your eligible dependent(s), you must enroll your eligible dependent(s) at this time.
When you enroll your dependents, you will be required to provide documentation, within the 30-day period,
verifying dependent status. If you do not enroll within the time requirement set forth in this paragraph, you will
be required to wait until the next open enrollment period unless either the Change in Status section or the
HIPAA Special Enrollment Rights section applies.
If you and your meet the eligibility requirements for the and wish to enroll in the ,
you either must complete and sign a paper enrollment form or submit a completed electronic form to
your . When enrolling, you must give accurate and complete information. If you do not, your benets
will be adjusted, and you will be required to refund the Plan any benets you and your dependents should not
have received. Once you are enrolled, you will receive your health plan identication card in the mail to your
home address.

33
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
If you do not have any eligible dependents at the time of initial enrollment, but acquire eligible dependents at
a later date, you must enroll the eligible dependent(s) within 30 days (or a longer period if required by state
law) of the date you acquire them. Coverage for newly-acquired eligible dependents will be eective on the
rst day an eligible dependent is legally acquired if you enroll them for coverage within the 30-day period
and provide the required dependent verication documentation. Contact your employer to determine what
documents are required to verify dependent status.
THE ENROLLMENT DEADLINES FOR NEW ELIGIBLE DEPENDENTS ACQUIRED VIA MARRIAGE, BIRTH,
ADOPTION, OR PLACEMENT FOR ADOPTION ARE TEMPORARILY EXTENDED DUE TO THE COVID-19
PANDEMIC, PER THE TERMS IN APPENDIX F.
If you are enrolled for coverage under the Plan as a participating employee or spouse, your newborn or adopted
child will be retroactively covered to the date of birth (or adoption or placement for adoption) if you notify your
employer of the birth/adoption, complete an enrollment form, pay the increased employee-share contribution
amount, and provide the required dependent verication documentation within 30 days of the date of birth (or
adoption or placement for adoption). If notice is not provided, you do not pay your employee-share contribution,
you do not complete an enrollment form, or you do not provide the required dependent verication
documentation within 30 days (or a longer period if required by state law), then your newborn or adopted child
will not be covered. Your (or your spouse’s) claim for maternity expenses is not considered as notication to
your employer. Placement for adoption means you have assumed and retained a legal obligation for full or
partial support of the child in anticipation of adoption. Placement for adoption is evidenced by a fully executed
adoption placement agreement.
Notication regarding the addition of the new eligible dependent should be made to your employer’s human
resources department as soon as possible.
Change in Status
If you have a qualifying change in status, you may change your enrollment decision regarding yourself and/or
eligible dependents within 30 days (or such longer period as provided by state law) of the qualifying change in
status. You can only change your benet elections if the requested change is on account of and corresponds
with the permitted election change event you experience.
If application is made on a timely basis and is accepted by the plan administrator as a qualifying change in
status, medical coverage will become eective on the date provided by your employer, except that in the case
enrollments due to HIPAA Special Enrollment Rights, coverage will be eective on the date of the event as
described in the below section. If application is not made within 30 days (or such longer period as provided by
state law) of the qualifying change in status, you will be required to wait until the next open enrollment period
unless you experience another qualifying change in status or the HIPAA Special Enrollment Rights section
applies.
If you and your spouse are both eligible employees and are enrolled as such in the Plan and one of
you terminates employment, the terminating spouse and any covered dependents will be permitted to
immediately enroll under the remaining spouse employee’s coverage. The new coverage will be a continuation
of prior coverage and any waiting period will not apply.
It is your responsibility to report changes in eligibility or general family or other status changes to
your . This includes divorces and turning age 26. It is considered fraud on the
if you fail to report events that result in an individual ceasing to be eligible for the and, in such
cases, you would be required to repay to the any benets that were erroneously paid.

34
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
HIPAA Special Enrollment Rights
HIPAA SPECIAL ENROLLMENT DEADLINES ARE TEMPORARILY EXTENDED DUE TO THE COVID-19
PANDEMIC, PER THE TERMS IN APPENDIX F.
As required by federal law, the Plan provides a special enrollment right in the following two circumstances:
A. Loss of Other Coverage: If you decline coverage under this Plan for yourself or your eligible
dependents because of other health plan coverage, and provide written notice to the Plan that you are
declining coverage due to the existence of other coverage, and such other health plan coverage is
later terminated because of:
• A loss of eligibility for such coverage (loss of eligibility does not include a loss because of: failure
to pay premiums when due; failure to exhaust COBRA continuation coverage, if elected; or cases
such as making a fraudulent claim or misrepresentation); or
• Termination of any company contributions for such coverage;
Then you and/or your eligible dependents that have lost such coverage may enroll in the Plan.
B. New Dependents. If you acquire a new eligible dependent as a result of marriage, birth, adoption or
placement for adoption, you and/or your newly eligible dependents may enroll in this Plan. In the case
of the birth, adoption, or placement for adoption of a child, your spouse may also enroll if he/she is
otherwise eligible for coverage.
To enroll under either of these special enrollment rights, you must notify your employer’s human resources
department and complete and return any required forms within 30 days of the underlying event (e.g., loss of
other coverage, date of the marriage, birth, adoption or placement for adoption). If you do so, then coverage
will begin on the date of the loss of other coverage, or for a new dependent child, the date of birth, adoption
or placement for adoption, or for a new spouse, the date of marriage.
Federal law also provides special enrollment rights in the following two circumstances:
(i) Loss of eligibility under Medicaid or a State Child Health Insurance Program (CHIP). If you or an eligible
dependent is covered under a Medicaid plan or a state CHIP plan, and that coverage is terminated
because you are no longer eligible, then you and your eligible dependent may enroll in the Plan if you
are otherwise eligible for coverage.
(ii) Becoming eligible under a State CHIP Premium Subsidy Program. If you or an eligible dependent are
determined to be eligible for a state CHIP premium assistance program, then you and your eligible
dependent may enroll in the Plan if you are otherwise eligible for coverage.
To enroll under either of these two latter special enrollment rights, you must notify your employer’s human
resources department and complete and return any required forms within 60 days of the date you lose
coverage under the Medicaid or state CHIP plan, or the date you are determined to be eligible for a premium
assistance program. If you do so, then coverage will begin on the date of loss of Medicaid/CHIP eligibility or
on the date you are determined to be eligible for a premium assistance program.
Open Enrollment
Open enrollment occurs once a year on dates to be determined by the plan administrator. Typically, open
enrollment for a plan year occurs in the fall of the prior plan year. During open enrollment, eligible employees
who are not covered may elect to begin coverage eective the rst day of the upcoming plan year and
covered employees may change their coverage eective the rst day of the upcoming plan year.
An employee who participates in the Plan in the 2021 plan year, may only elect the Accelerate option of this
Plan for 2022 if the employee and the employee’s enrolled dependent spouse (if applicable) each earned 10,000

35
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
wellness participation points during the period of September 1, 2020 through July 31, 2021. (Points will be
prorated if you initially enroll in this Plan on April 1, 2021 or later; and the point requirement will be waived if
you initially enroll in this Plan on July 1, 2021 or later.)
If you do not timely enroll in accordance with this SPD, you will be required to wait until the next open
enrollment period unless either the Change in Status section or the HIPAA Special Enrollment Rights section
applies.
Pre-Existing Conditions
This Plan does not have any exclusions for pre-existing conditions.
Dual Coverage
If you and/or your spouse are both enrolled as employees under this Plan, you and/or your spouse have
the option to enroll your eligible dependents for coverage. However, no person may be covered as both an
employee and as a dependent, nor can a person be covered as a dependent of two employees. And in no
event may the combined maximum benets for you and/or your spouse and your dependents exceed 100% of
the usual, reasonable, and customary charge for eligible expenses.
Reinstatement of Coverage
If you are called to active duty by any of the armed forces of the United States of America, released under
honorable conditions and return to employment with your employer: (1) on the rst full business day following
completion of your military service of 30 days or less, (2) within 14 days of completing military service of
31 to 180 days, or (3) within 90 days of completing military service of more than 180 days, coverage will be
reinstated. You will not be subject to any new waiting period; however, all accumulated annual and lifetime
maximums will apply.
If coverage ends while you are on a protected leave, coverage for you and your eligible dependents will be
reinstated on the day you return to work as long as you return immediately upon the end of the protected
leave. When coverage is reinstated, your prior permission for salary reductions to pay the employee-share
contribution will be resurrected. If coverage ends while you are on a non-protected approved leave, coverage
for you and your eligible dependents will be reinstated on the rst of the month following the month in which
you return to active employment as long as you timely re-enroll for reinstatement upon your return from the
non-protected approved leave. You will not be subject to any new waiting period; however, all accumulated
annual and lifetime maximums will apply.
If you are in an eligible status, but coverage had never become eective or had terminated because of failure
to make the required employee-share contribution, you will be required to wait until the next open enrollment
period unless either the Change in Status section or the HIPAA Special Enrollment Rights section applies.
If you have a termination of employment and are rehired by and are credited with an hour of service with your
employer or any other participating employer within 13 weeks of your termination of employment, then (1)
your ACA full-time employee status will be determined upon rehire as if you did not incur such termination of
employment, (2) you will receive credit for your pre-termination hours of service, and (3) your period with no
hours of service is taken into account as a period of zero hours of service during the measurement period. If
you transfer from one participating employer to another participating employer, for purposes of determining of
your ACA full-time employee status, you will be treated as continuously employed and will continue to receive
credit for your pre-transfer hours of service.
Special Situations, Extension of Coverage
Coverage of Adult Children with Disabilities
If a child is unmarried, is totally disabled, and is primarily dependent on the employee parent for support and
maintenance, the child’s eligibility will be extended past attainment of age 26 for as long as the employee

36
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
parent is covered under this Plan, the total disability continues, and the child continues to qualify for coverage
in all aspects other than age. You must provide evidence of total disability within 31 days of the child’s 26th
birthday, and annually threafter if requested by the plan administrator. In no event will coverage under this
section extend beyond the last day of the month of the child’s marriage.
Leaves of Absence
The following provisions apply to coverage during a period when you are absent from work:
i. Paid time o. If you were covered under the Plan on the day before you began taking paid time
o (PTO) (including paid sick leave and paid vacation leave), you (and any covered dependents) will
continue to be eligible for Plan coverage during the PTO and you will be required to pay the same
employee-share contribution during the PTO that you were paying the day before the PTO began.
ii. other than USERRA leave. If you qualify for a protected leave of absence (other than
USERRA, see below) and you are covered under the Plan on the day before the leave begins, you will
be eligible to continue your coverage (and the coverage of any covered dependents) for the duration
of the protected leave at the employee-share contribution rate you were paying the day before the
protected leave began (if so required by the relevant statute). You should talk to your human resources
department to determine how to pay your employee-share contribution during your protected leave.
Subject to certain exceptions, if you fail to return to work after the protected leave, your employer has
the right to recover from you any contributions toward the cost of coverage made on your behalf
during the leave. The rules for dierent types of protected leaves vary and some are dealt with under
state law and within participating employer policies.
iii. Uniformed Services Employment and Reemployment Rights Act of 1994 (“USERRA”) leave.
Notwithstanding any other provision of the Plan, for USERRA continuation coverage, enrollees
can receive up to 30 days of coverage at the active-employee rate followed by up to 24 months
of USERRA continuation coverage at 102% of the total cost of coverage (which is the employer
contribution plus the employee-share contribution). Coverage will end sooner if you (1) are required
to apply for or return to a position of employment and fail to do so; or (2) fail to make the required
contributions for Plan coverage. In most cases, USERRA requires election of coverage within 30 days
of the beginning of leave and requires that you give advance notice of your leave. If you are unable
to give advance notice and/or complete the election within 30 days, you must make an election for
retroactive coverage within 30 days of the date that giving the notice is possible, reasonable, or nor
longer precluded by military necessity and the election must be accompanied by (1) a statement
of the reason(s) why you were unable to give advance notice, and (2) payment in full for the unpaid
contribution amounts due for each month of coverage beginning as of the date you were rst absent
from work due to the USERRA leave and including the contribution amount due for the month of the
election. If the election is given after the maximum USERRA period has elapsed, coverage will be only
for the USERRA period and payment must be for the entire period. Your rst payment for USERRA
coverage is due no later than the last day of the month the plan administrator or your employer
receives your USERRA election, and if full payment is not received by the due date, then USERAA
continuation coverage will cease retroactively eective as of the last day of the month for which a
payment was received in a timely manner. Dependents who join the military are ineligible for USERRA
coverage under this Plan.
iv. All. You may continue to participate in the Plan during an approved leave. If you take
a paid approved leave, any employee-share contributions you are required to make to the Plan will be
made by payroll deduction. If you take an unpaid, non-protected approved leave, you will be required
to pay any required employee-share contribution by the last day of each month or your coverage
under the Plan will end. You should talk to your human resources department to determine how to
pay your employee-share contribution during your approved leave. If you use PTO while on a non-
protected approved leave, the Paid time o paragraph above will apply. An employee on an approved
leave may add dependents to the Plan under the same rules and at the same time as employees
who are not on leaves of absences. Dependents are ineligible to participate in the Plan unless the
employee elects to participate. There is no waiting period to enroll in the Plan for employees returning

37
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
from an approved leave of absence and their dependents, even if coverage under the Plan terminated
during the approved leave of absence. Unless specied elsewhere in the Plan, a failure to pay your
employee-share contribution within 30 days of the due date established by your employer will result
in termination of the coverage as of the last day of the month in which occurs the 30th day after such
due date. (For protected leaves, termination of coverage will not occur until after the payment is 30
days late and a 15-day notice of termination of coverage is mailed to the employee.)
When Coverage Ends
Your coverage ends the earliest of:
• the latter of (a) the end of the month in which your employment with your employer ends, or(b) the
end of the month in which you cease to be paid for full-time work;
• the end of the period for which your last required employee-share contribution was made; or as state
law permits, the day your employment ends with a pro rata return of employee-share contributions
already collected;
• the date your employment with your employer ends, if so elected by your employer and your coverage
has been fully employer paid; or
• the end of the month in which you are no longer eligible to participate in this Plan. (See “Special
Situations, Extension of Coverage” for additional information.)
Coverage for your covered dependents ends the earliest of:
• the date your coverage ends;
• the date the covered dependent no longer meets the eligibility requirements, including, if applicable,
the date you are no longer legally required to provide medical coverage for the covered dependent;
• the end of the month for which the last employee-share contribution was made; and
• the date the covered dependent enters into active military service or obtains permanent residence
outside the United States (and outside of the territory in which you are stationed, if you are stationed
within an included U.S. territory). (See “Special Situations, Extension of Coverage” for additional
information.)
Following one of the events listed above, your covered dependents may be eligible for Continuation Coverage.
See the Coverage Continuation Options section for more information.
If the Plan is terminated, coverage ends for you and your covered dependents on the date the Plan ends
unless an extension of coverage in required under state law. Expenses incurred prior to the Plan termination
will be paid as provided under the terms of the Plan prior to its termination.
See the Special Situations, Extension of Coverage section above for the end of coverage provisions that will
apply while you are on an approved leave. Also, see the Reinstatement of Coverage section above for special
rules for employees whose coverage ends while on a protected leave or a non-protected approved leave.
If this SPD otherwise allows you to terminate your coverage or coverage for any covered dependents, you may
do so by giving written notice to your employer’s human resources department. If you terminate your own
coverage, coverage for your covered dependents also ends at the same time.
Continuation Coverage
The Plan does not generally provide continuation coverage, such as coverage under COBRA. As a church
plan, the Plan is not required by law to provide COBRA coverage. However, the Plan may provide limited

38
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
continuation coverage in the following situations:
A. Short-Term Post-Termination Coverage
• If other healthcare coverage is not available at the time coverage terminates for an employee, the
former employee and covered dependents of the former employee may be eligible for continued
benets under this Plan for a short period after coverage terminates, provided that the employer oers
such coverage. The coverage may be granted for a period of up to two months (60 days) or until the
former employee has obtained other health coverage (including Medicare), whichever comes rst.
• The employer may require the former employee to pay a contribution for the cost of providing such
coverage. In lieu of this coverage, an employer may choose to oer the former Member short-term
medical plan coverage at his or her expense or may not oer either type of coverage.
B. Certain Divorce Situations
• The employer may, in its sole discretion, allow the spouse or ex-spouse of employee or ex-employee
and certain children to remain on the Plan after legal separation or divorce from the employee or ex-
employee, if the separation or divorce was due to unlawful actions of the employee or ex-employee
or to circumstances beyond the control of the spouse or ex-spouse of the employee or ex-employee
or in other situations approved by the employer. The following persons who were participating in
the Plan prior to the divorce or separation may continue to participate in the Plan for a period not
to exceed twelve (12) months if allowed to do so by the employer and they would otherwise meet
the eligibility rules for the Plan if the separation or divorce and, if applicable, the ex-employee’s
termination of employment, had not occurred: (1) the spouse or ex-spouse of the employee or ex-
employee; (2) children of the spouse or ex-spouse of the employee or ex-employee; and/or (3) children
of the employee or ex-employee. The employer, however, is not obligated to extend coverage under
this provision and the employer may charge a contribution for participation.
C. Disability
• If you are no longer eligible for coverage under this Plan due to your total disability (such as your
employment is terminated due to your disability or you are no longer on an approved leave of
absence due to your disability), and you and/or your covered dependents are not eligible for coverage
under another plan, coverage under this Plan for you and/or your covered dependents in eect at the
time of your loss of eligibility for the Plan may continue for up to 24 months following the date you lost
eligibility for the Plan.
• Your continuation coverage for you and your covered dependents will cease under this paragraph
prior to such periods as soon as any other healthcare coverage (including Medicare) is available to
you. The right to continuation coverage for your covered dependents will cease under this paragraph
prior to the end of such 24-month period as soon as your dependents are eligible for other healthcare
coverage (including Medicare).
• If you have applied for a Social Security Administration determination of disability, you may request
coverage under this section while the determination is pending and the plan administrator, in its sole
discretion, may allow you to continue coverage under this Plan until the determination is received.
In no event will the entire period of coverage under this Disability continuation coverage period be
greater than a total of 24 months.
D. Death
• If you die and your covered dependents are not eligible for coverage under another plan, coverage
under this Plan that is in eect at the time of your death will continue for your covered dependents for
up to six months following the date of your death. The right to continuation coverage will cease under
this paragraph prior to the end of such six-month period as soon as your covered dependents are
eligible for other healthcare coverage (including Medicare).

39
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Notwithstanding the above, if any required contribution for continuation coverage is not paid within 30 days of
the due date for such contribution, continuation coverage will terminate immediately.
Marketplace Coverage Continuation Option
You may be eligible to buy an individual plan through the Health Insurance Marketplace when you lose
group health coverage. By enrolling in coverage through the Marketplace, you may qualify for lower costs
on your monthly premiums and lower out-of-pocket costs. Additionally, you may qualify for a 30-day special
enrollment period for another group health plan for which you are eligible (such as a spouse’s plan), even if
that plan generally doesn’t accept late enrollees.
Depending on your state or of residence, the provisions of this Continuation Coverage section
may be superseded by law, and you may be entitled to additional benets.
Employee-Share Contribution
The Plan is self-funded by means of employer and employee contributions. The contribution enrolled
employees are required to make is called the employee-share contribution. Your employer is responsible for
paying all of the benets due to you under this Plan that are not covered by your employee-share contributions
and other required cost-sharing. This Plan is not insured, and neither the plan administrator nor any other
participating employer is responsible for paying any part of your benets.
Your employee-share contribution is based on the number of enrollees you elect to cover. Each additional
enrollee will require an increase in your employee-share contribution.
The employee-share contribution may be dierent for full-time employees, for those employees who are not
categorized by their employer as full time (but are ACA full-time employees), and for those employees on
certain leaves of absence or continuation coverage.
The employee-share contribution amount is determined by your employer. You may contact your human
resources department for information on the employee-share contribution.

40
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Pre-Certication Program
The Plan has certain procedures that must be followed to reduce the cost of Plan benets, such as a pre-
admission/pre-service review process called pre-certication, which is performed by the Plan’s utilization
review manager. The Plan’s utilization review manager can be reached by calling Customer Service at (888)
276-4732.
The purpose of pre-certication is to contain the cost of Plan benets by encouraging prudent and reasonable
use of health care and health care facilities. These measures are only decisions as to whether a particular
treatment or service is medically necessary within the meaning of the Plan (and not, for example, what course
of medical treatment may be appropriate or desired, whether a patient is eligible for or enrolled in the Plan, or
whether the services are subject to Plan limitations or exclusions).
The Plan does not provide medical advice and is not to be considered a substitute for the medical judgment
of your attending physician or other health care provider. In all instances, the nal and ultimate decisions
concerning appropriate and desired medical treatments are up to you and the physician or other professional
providing your treatment. The Plan only decides whether a particular admission, treatment or service is
medically necessary within the meaning of the Plan. If the Plan determines that an admission, treatment or
service is not medically necessary, then the admission, treatment or service will not be covered.
Your employer, the Plan, the plan administrator, and their employees, members, agents and representatives,
are not liable for any act or omission by any hospital, physician, other providers or suppliers, their agents or
employees, in caring for a person covered by this Plan, and no responsibility attaches under this Plan for any
error or inability of any provider or supplier to furnish accommodations, services or supplies to you.
The performs only; it does not guarantee
benets or payment for services rendered, nor does it validate participating status of the
provider or facility.
Medical Necessity Pre-Certication
Medical necessity pre-certication is a process that takes place when a physician or other provider
recommends hospitalization or other types of medical services/supplies and the Plan requires that pre-
certication sta members evaluate a proposed hospital admission or other services/supplies in order to
verify whether the proposed admission or service/supply is medically necessary within the meaning of the
Plan and/or to analyze and discuss other care options that may exist.
Your Responsibility
You do not need to obtain medical necessity pre-certication for routine in-network health care performed in a
provider’s oce, urgent care center, emergency room, or via telehealth
It is your responsibility to obtain medical necessity pre-certication for diagnostic testing, out-patient
procedures, non-emergency hospitalizations, surgeries, etc., in accordance with the below list. Your provider
can request medical necessity pre-certication by calling the number on your benet card. If your emergency
care results in a hospital admission, your provider must call the utilization review manager no later than the
next business day after the admission.
When you know in advance that you or a covered dependent needs to be hospitalized, you or your provider
must contact the utilization review manager via Customer Service at 888-276-4732 before the hospitalization.
In the case of an emergency hospital admission or other urgent situation that did not allow the provider to
contact the utilization review manager in advance of the admission and/or treatment, you or your provider
must notify the utilization review manager within 24 hours of the admission/treatment or on the next business
day. The utilization review manager will carry out retrospective medical necessity pre-certication.

41
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Services Requiring Pre-Certication
There are services under the Plan for which you will not receive benets if you fail to obtain pre-certication
before obtaining the service or incurring the expense. This means that if you do not receive pre-certication
for such service, you and/or your provider will not receive payment and so you will be responsible for any
expense incurred.
You or your provider should call the utilization review manager at the phone number on your benet card to
fulll any pre-certication requirements and obtain pre-certication or guidance for those services. The Plan’s
utilization review manager handles all pre-certications and generally follows the guidelines set forth by the
MCG Health and Aetna in determining medical necessity and appropriateness of services. However, in so
doing, the Plan’s utilization review manager has discretionary authority to use other resources in addition to
those already mentioned in determining medical necessity.
The following services requires pre-certication, but this list is not inclusive of all services that require pre-
certication; the list is subject to additions or deletions at the discretion of the plan administrator; additional
services are listed in this SPD and may change at the Plan’s discretion.
1. All inpatient admissions and services (except for observation only in a PPO facility by a PPO provider and
normal delivery in a PPO facility by a PPO provider);
2. All inpatient surgeries;
3. Specialty provider consultations and oce visits with a non-PPO provider and/or in a non-PPO facility;
4. Maternity and pregnancy related care that is not preventive (as specied in Appendix A), routine
pregnancy care (as specied at https://www.guideline.gov/summaries/summary/38256), or
delivery with a hospital stay of up to 48 hours following a normal vaginal delivery or 96 hours following a
cesarean delivery (normal delivery requires pre-certication if by a non-PPO provider and/or in a non-
PPO facility);
5. Athletic training assessment;
6. Articial implantable cardiac-debrillator (AICD), wearable (external) cardiac debrillator, and implantable
cardioverter debrillator;
7. Articial pancreas device system and supplies;
8. Cardiac event recorder (implantable);
9. Cardiac Center of Excellence (CCOE) benets (including surgery, related services, and travel/lodging);
10. Ventricular assist devices (including left ventricular assistive device (LVAD));
11. Articial heart procedure and accessories
12. Treatment for temporomandibular disorders (non-surgical);
13. Hyperthermic Intraperitoneal Chemotherapy Administration (HIPCA);
14. Photochemotherapy (PUVA);
15. Autologous chondrocyte implantation, autologous chondrocyte transplantation, or osteochondral
allograft;
16. High cost/specialty medications billed by the provider through the medical benet require pre-
certication though the utilization review manager (Adventist Health Benets Administration). Examples
of high cost/specialty medications commonly billed though the medical benet by the provider are
oce-administered injectable medications, infusion therapy, chemotherapy, and home infusion therapy.

42
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
(Some selected therapies intended for acute use, such as IV hydration and IV antibiotics, do not require
pre-certication.) High cost/specialty medications processed through the pharmacy benet (such as
self-injectable, oral medications, and certain infusion medications) require pre-certication through
pharmacy benet manager (Express Scripts);
17. Implantable infusion pumps for pain/spasms;
18. Genetic testing;
19. Intensity-modulated radiation therapy (IMRT); stereotactic radiosurgery (gamma knife, cyberknife, linear
accelerator); proton beam;
20. Hyperthermia in conjunction with chemotherapy or radiotherapy for treatment of cancer;
21. Endobronchial brachytherapy;
22. Transcranial magnetic stimulation (TMS) as treatment of depression and other psychiatric/neurologic
disorders;
23. All plastic, cosmetic, or reconstructive surgery, including orthognathic surgery, and cosmetic procedures
except initial breast reconstruction following medically necessary mastectomy;
24. Removal of breast implants or other prosthetic implants that were implanted for cosmetic purposes;
25. Nail debridement;
26. Pectus deformity repair;
27. Scar revision;
28. Varicose vein procedures (e.g., sclerotherapy, echosclerotherapy, endovenous ablation RF or laser,
ligation, stab phlebectomy);
29. Pneumatic compression devices and garments;
30. Laser treatment for inammatory skin disease (such as psoriasis, dermatitis, vitiligo;
31. Capsule endoscopy;
32. Continuous glucose monitoring receivers and supplies when exceeding manufacturer recommended
quantity limits;
33. Insulin pumps;
34. Assistive listening devices, FM/DM systems;
35. Cranial remolding helmet;
36. Bath/shower chairs, rails, transfer benches, hospital beds;
37. Spinal cord stimulation;
38. Kyphoplasty or vertebroplasty;
39. Liquid nutrition and total parenteral nutrition; enteral feeding pumps, supplies, and formulas;
40. Articial discs, cervical and lumbar;
41. Transplants (including workup);
42. Acute inpatient rehabilitation and/or skilled nursing facility admissions;

43
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
43. Cognitive rehabilitation;
44. Applied behavioral analysis therapy;
45. Developmental, behavioral, neuropsychological, neuroCl testing – outside of a pediatrician’s oce;
46. Outpatient Physical Therapy (PT), Occupational Therapy (OT), and Speech Therapy (ST), after the initial 12
visits per condition or incident (but this pre-certication only needs to be done once per condition being
treated, and does not need to be renewed each year);
47. Electroencephalogram, if performed as an inpatient, multi-day test;
48. External counterpulsation (EECP);
49. Oscillatory devices for respiratory disease (The Vest);
50. UV light therapy (including light therapy for Seasonal Aective Disorder); home UV light systems, and
light boxes;
51. All inpatient behavioral health services, including psychiatric, detoxication and substance use
disorder treatment. All partial hospitalization programs; residential psychiatric, substance use disorder
or concurring psychiatric and substance use disorder treatment facilities; and intensive outpatient
programs;
52. Durable medical equipment or repair with billed charges of $2,000 or more, all CPM devices/machines,
and Dynasplints (regardless of cost);
53. Orthotics/prosthetics with billed charges over $2,000 and/or custom orthotics;
54. Radiofrequency ablation, except for pain management; microwave tumor ablation and radioembolization
of tumors;
55. Mammography 3D Tomosynthesis screening if under the age of 40;
56. RESERVED;
57. RESERVED;
58. RESERVED;
59. Sacral nerve stimulation (implanted) for pelvic oor dysfunction;
60. Sacroiliac joint fusion;
61. Sacrocolpopexy;
62. Vagus nerve stimulation;
63. Implantable intrastromal corneal ring;
64. Cochlear implants (including supplies and replacements) and bone-anchored hearing aids;
65. Wound vacuum therapy and supplies;
66. Non-emergency ground ambulance transportation and any air transportation (unless the utilization
review manager determines that ground transportation would have endangered the life of the enrollee);
67. Any nonspecic codes (procedures and HCPCS codes ending in 99);
68. Surgical treatment of snoring and obstructive sleep apnea; laser-assisted uvulopaltoplasty (UPPP);

44
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
69. Back surgery (all);
70. Bariatric, bowel, or gastric surgeries (all), including lap band surgery;
71. BiPAP devices
72. Oral devices for sleep apnea if charges exceed $2,000;
73. Botox injections; dermal ller injections;
74. Spinal column or spinal cord procedures, decompression surgery (posterior fossa decompression), or
Chiari malformation procedures; image-guided minimally invasive lumbar decompression for spinal
stenosis; neurostimulator or neuromuscular stimulator (implantable) receiver or transmitter, generator,
and supplies; discectomy (anterior approach lumbar spine);
75. Dialysis;
76. Dental anesthesia when covered as a medical service (except for pediatric sedation);
77. Home health services (will require submission of a home health care plan);
78. Hospice services;
79. Hyperbaric oxygen therapy;
80. Corneal collagen cross linking;
81. Vision therapy (orthoptics);
82. Abortion (also referred to as termination of pregnancy) will be reviewed for consistency with the
coverage requirements set forth in the Benets Description chapter which are based on Seventh-day
Adventist Church teachings, and a Care Manager may be assigned to conduct a consultation;
83. Elective surgery for the prevention of cancer.
If you are not sure whether your provider has requested , you should call the
via Customer Service at 888-276-4732 to verify that
has been initiated.
Failure to Obtain Pre-Certication
If services or supplies that require are not , the will not reimburse you
for expenses incurred. The expenses you incur due to not receiving will not be applied to
your deductible or out-of-pocket maximums. If medical services that require pre-certication are not pre-
certied, the Plan will also not reimburse you for any associated services. (For example, if a surgery requiring
pre-certication is denied, associated anesthesia fees will not be covered and the expense you incur will not
be applied to your deductible or out-of-pocket maximums.)
It is your responsibility to follow the Pre-Certication Program procedure and it is your responsibility to
make sure is successfully obtained prior to hospital admission or other treatment.
Eect on Deductibles and Out-of-Pocket Limit
If you assume additional expenses due to your failure to adhere to the pre-certication requirements in this
SPD, any additional expenses you assume will not be applied toward your deductibles and out-of-pocket
maximums.

45
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Required Second Surgical Opinion
The Plan may require that you or your covered dependent be examined by another physician to determine that
the surgery proposed by your own physician is medically necessary. The Plan pays the full cost of this required
second surgical opinion with the co-payment waived.
Care Management
Special care management is designed to help manage the care of patients who have special or extended
care illnesses or injuries.
The primary objective of special care management is to identify and coordinate cost-eective medical care
alternatives meeting accepted standards of medical practice. Special care management also monitors the
care of the patient, oers emotional support to the family, and coordinates communications among health
care providers, patients and others. Patients are identied as possible candidates for care management using
the following criteria:
i. Patients with diagnoses including cancer, HIV/acquired immunodeciency, degenerative nerve
diseases, burns, major trauma, cystic brosis, high risk pregnancy and birth, depression, COPD,
diabetes, infectious processes, GI disorders and complex co-morbidities;
ii. Patients with very high-cost medical expense; or
iii. Patients identied through the utilization management process, by their provider, or by themselves.
The Care Manager will contact enrollees to talk about the patient’s condition, to oer educational information, and
to identify available medical resources. The Care Manager will complete a comprehensive health assessment
and enroll the enrollee in care management if appropriate. The Care Manager will work with the enrollee, family,
physicians, and professional providers to optimize the enrollee’s use of medical benets and help the enrollee
and family take charge of the enrollee’s health and medical care. An individualized Care Management plan will
be developed for the enrollee in collaboration with the enrollee, the Care Manager, Medical Director and/or
Medical Advisor. The Care Manager follows the care and treatment of the patient enrolled in care management
to verify that: recommendations to physicians and professional providers are followed, medical appointments
are kept, the patient receives all necessary and appropriate medical treatment timely, the treatment is medically
necessary and appropriate, that medical treatment is received in-network whenever possible (out-of-network
providers and/or out-of-network facilities may be utilized as part of the treatment on an exception basis, but
only with prior authorization and an approved Unavailable Service Request Form); and facilitates the provision
of necessary and appropriate treatment of the patient. The Care Manager is available to talk with the patient and
family to answer their questions and to facilitate the provision of needed support.
Facilitation of Patient Transfer to Participating Facilities Following Medical Emergency
The utilization review manager will facilitate the medical transfer of patients who were hospitalized at an out-
of-network hospital or other facility as a result of an emergency medical condition. Transfer of the patient to an
in-network facility will only be initiated once the patient’s medical condition is stabilized.
If the patient refuses medical transfer once the determines that the transfer is
safe and appropriate, benets for subsequent services provided by will not be
provided. The expenses you incur for refusing medical transfer will not be applied to your deductible or
out-of-pocket maximums.
Determination of Where Needed Medical Services are Available
The utilization review manager sta is very knowledgeable about the availability of medical services from in-
network providers and in-network facilities.
If you or your provider believes that needed medical services are not available from an in-network provider

46
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
or in-network facility, you or your provider can call the utilization review manager at 1-888-276-4732. The
utilization review manager sta will obtain medical information from your provider describing the condition
of you or your covered dependent and the needed medical services. If it is determined that covered services
are not available within the network, you may make application to the utilization review manager to apply the
special Unavailable Services coverage level listed in the Schedule of Benets to covered services provided by
the out-of-network providers by using the Unavailable Service Request Form and procedure as outlined in the
Unavailable Services section of the Physician and Provider System chapter.
UNAVAILABLE SERVICES REQUEST PRIOR-AUTHORIZATION PROCESS
• Member must contact the via Customer Service at 888-276-4732 and
request an Unavailable Service Request Form.
• Member should work with Provider to complete and return form.
• Approval of the Unavailable Service Request Form (letter of agreement) may take up to 30
calendar days.
• Final determination and meeting response time above is contingent on timely responses from the
Provider and member.
Pre-Certication for Prescription Drugs
Pre-certication is required for some prescription drugs. Express Scripts manages pre-certication for
prescription drugs. Your doctor or pharmacist will request pre-certication through the Express Scripts Contact
Center, which is available 24 hours a day, seven days a week. Contact information is below:
Express Scripts
Member Services: 800-841-5396
Pharmacists: 800-922-1557

47
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Providers and Facilities Available Under the Plan
Choice of Providers and Facilities
You have a choice of obtaining provider services (physician and other licensed professional providers) from
any PPO provider. You have a choice of obtaining facility services (including hospital, outpatient laboratory,
radiology, home health care, and mental health inpatient and outpatient) and supplies from any PPO facility.
Your choice of providers/facilities may be subject to case management. See the Case Management
section for details.
In the case of an emergency, benets will apply as discussed in the Emergency Services section of the
Benets Description chapter.
Employees stationed in the included U.S. territories and their eligible dependents may choose to receive
provider and facility medical services from any providers/facilities in the included U.S. territories. (But note that
the use of pharmacies contracted with ESI is still required in the territories.)
Primary Care Provider
The Plan does not require you or your covered dependents to designate a primary care provider (PCP).
Membership Card
After enrolling, you and your covered dependents will receive your benet ID card which will include your
employer and identication numbers, and instructions for medical necessity pre-certication. You will need to
present your card each time you receive services from a physician or professional provider. If you lose your
benet ID card, we will issue a replacement. Contact the plan administrator at 888-276-4732, or by requesting
through the www.Ascendtowholeness.org website.
Unavailable Services
If covered services cannot be rendered at a PPO facility or by a PPO provider due to the unavailability of the
service needed, a request may be made for coverage at a non-PPO facility or with a non-PPO provider at the
special Unavailable Services coverage level listed in the Schedule of Benets. Your personal physician not
being part of the PPO Network or on the medical sta at a PPO facility, or your PPO provider leaving the PPO
Network will not be considered valid unavailable services situations.
Unless the is urgent or emergent, a coverage request must be made and approved (via an
Unavailable Service Request Form) prior to services being rendered. If the service is urgent or emergent
the coverage request should be submitted as soon as possible after the service has been provided. The
must approve the request.
Emergency Care and Hospitalization due to an Emergency Medical Condition
Claims for emergency care that are ultimately determined by the utilization review manager to be medically
necessary will be paid even without medical necessity pre-certication by the Plan. However, you or your
provider must notify the Plan of your hospital admission within 24 hours or the next business day of your
emergent in-patient hospital admission following a hospital emergency department visit. Upon notication,
the utilization review manager will work with the hospital and your physician to facilitate transfer, as
appropriate, to an in-network facility as soon as you are stabilized and able to be transferred.
It is your responsibility to make sure that the pre-certication process elaborated in this section has been
followed.

48
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Hospitalization not due to an emergency medical condition
For care not due to an emergency medical condition, should your physician determine that hospitalization is
needed, arrangements will be made for you to be admitted to a hospital if, and after, medical necessity pre-
certication has been granted by the utilization review manager. The utilization review manager will review
elective admissions and work with the physician to assure that the patient avoids unnecessary time in the
hospital.
It is your responsibility to make sure that the pre-admission process elaborated in the Pre-Certication
Program section has been followed.
Cost-Eectiveness Services
At our sole discretion and under unique and unusual circumstances, the plan administrator may approve
benets for cost eectiveness services not otherwise covered by the Plan.
Payment of benets for cost eectiveness services shall be at the sole discretion of the plan administrator
based on its evaluation of the individual case. The fact that the Plan has paid benets for cost eectiveness
services for a covered person shall not obligate the Plan to pay such benets for any other covered person,
nor shall it obligate the Plan to pay benets for continued or additional cost eectiveness services for the
same covered person. All amounts paid for cost eectiveness services under this provision shall be included in
computing any benets, limitations, co-payments or co-insurance under the Plan.

49
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
General Benet Rules
When all of the provisions of this Plan are satised, the Plan will provide benets as outlined on the Schedule
of Benets for the services and supplies listed in this section. As to all benets described herein, only
medically necessary services are covered up to the usual, reasonable, and customary charge, when provided,
ordered, or referred by a physician or professional provider practicing within the scope of their licenses.
The Plan only pays for expenses covered by the Plan if the expenses:
1. are medically necessary or are for preventive services (listed in Appendix A) covered by the Plan;
2. represent a commonly accepted form of treatment and meet professionally recognized national
standards of quality;
3. are recognized as generally accepted by the American medical community;
4. result from a non-occupational illness, injury or other event or cause;
5. are of a type specically listed in the Benets Description sections of this document;
6. are a type of expense for which the Plan does not otherwise limit or exclude payment; and
7. do not exceed Plan Year or Lifetime Maximum limits.
All covered services, other than preventive care services, must be medically necessary. The Plan determines
what is medically necessary and the decision is nal and conclusive. Even though your provider may
recommend a procedure, service or supply, the recommendation does not always mean the care is medically
necessary. (See Denitions section for denition of medically necessary.)
Failure to obtain required pre-certication will result in non-payment by the Plan.
Any services performed by a provider must be performed by a physician or professional provider.
There may be alternative procedures, services, or supplies that meet medical necessity criteria for diagnosis
and treatment of your condition. If the alternatives are substantially equal in clinical eectiveness and use
similar therapeutic agents or regimens, the Plan reserves the right to approve the least costly alternative.
Many items are not covered by the Plan even though they may provide signicant patient convenience or
personal comfort. Such items may include raised toilet seats or sauna baths. Such items do not meet the
medical necessity requirement that the item be expected to make a meaningful contribution to the treatment
of the illness or injury.
In addition, expenses must be incurred while the coverage is in eect. All expenses are treated as being
incurred on the date that the service or supply is provided to the patient, not on the date the bill was sent
or paid. Expenses incurred before your Plan coverage becomes eective or after your Plan coverage has
terminated will not be covered.

50
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Description - Medical
NOTE: It is possible that you may receive additional benets based on your employer and the location of your
employment due to:
1. Specications in the PPO Network contract with your provider; and/or
2. State, territory or local laws that apply in your state, territory, or city (if applicable to the Plan).
ABORTION
Abortion (also referred to as termination of pregnancy) will be covered where the pregnancy poses signicant
threats to the pregnant woman’s life or serious jeopardy to her health, where there are severe congenital
defects incompatible with life carefully diagnosed in the fetus, or where the pregnancy resulted from rape or
incest. Consistent with Seventh-day Adventist Church teachings, abortions for reasons of birth control, gender
selection, or convenience are not condoned by or covered by the Plan. Care management sta are available
to consult with a pregnant member and her physician about these issues and to ensure that these Plan
requirements for coverage are met in any given situation.
AMBULANCE SERVICES
The Plan pays a percentage of the charges for necessary professional emergency ambulance transportation
to the hospital for inpatient treatment or outpatient treatment of an accident, and any medical services
provided en route. It is expected that ambulance services will be used only when medically necessary and
involving life threatening conditions such as severe bleeding, severe breathing diculty, unconsciousness or
serious injury.
Your Plan will cover Ambulance Transport Services (professional air or ground) to the nearest adequate
hospital, urgent care center, or nursing facility to treat your illness or injury. Local air and ground ambulance
means that you or your eligible dependents are transported to a hospital, urgent care center, or nursing
facility in the surrounding area where your ambulance transportation began.
The Plan will cover your ambulance transport provided the following criteria are met:
1. No other method of transportation is appropriate.
2. The services necessary to treat this illness or injury are not available in the hospital or nursing facility
where you are an inpatient.
3. The hospital or other facility is nearby and the hospital or facility is adequate and available to treat
your medical condition.
4. Coverage for air ambulance services has been pre-certied by the utilization review manager or, if
not pre-certied, the utilization review manager determined that ground transportation would have
endangered the life of the enrollee.
5. Any ambulance transportation other than to a facility for emergency treatment must have pre-
certication or it will not be paid.
CARDIAC CENTER OF EXCELLENCE (CCOE) SURGERY BENEFIT
When non-emergency cardiac services may be needed by a Member, the Plan allows a Member access to a
nationwide Cardiac Center of Excellence network through the Plan’s pre-certication process. This benet is
only available to those Members who have primary coverage under the Plan and who have been approved
by the CCOE based on a review of the Member’s diagnosis and medical history. (See Coordination of Benets
section for determination of primary versus secondary coverage.)

51
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
The Plan will pay 100% of your CCOE Surgery Benet (no deductible, co-payments or co-insurance will apply)
for approved services. CCOE Surgery Benet expenses include all medical costs incurred under the CCOE
Surgery Benet as well Travel Expenses.
While at the CCOE the pre-operative visits and post-operative visits are included in the CCOE Surgery Benet.
Once the Member is transitioned from the Cardiac Center of Excellence networks care, future claims for
services will be handled according to the provisions of the Plan.
If a change in surgery date is requested by the Member, the Member will be responsible for the cost
associated with the change, including any transportation cancellation fees and/or higher costs.
To be eligible for Travel Related Expenses the Member must travel at least 50 miles one-way from home to
the CCOE Provider.
Travel Related Expenses means;
Airfare: Plan will provide airfare (economy/coach class tickets, and up to one checked bag per
person) for patient and one traveling companion. Airline reservations must be made by
WebTPA. WebTPA will make any approved changes to ight schedules. The Plan will not pay
for additional costs associated with non-approved changes in airfare unless approved by
WebTPA.
Airport Parking
Personal vehicles will be covered for actual cost up to $15/day.
Alternate transportation to/from the airport, will be covered for actual cost up to a total of $100
round-trip.
Driving to/from CCOE Facility
Rental Car: Only one car rental, economy/standard class vehicle will be covered. Car rental insurance
and liability are the responsibility of the member.
Personal Car: Members will be reimbursed at the IRS standard mileage rate (medical purposes).
Mileage will be paid for travel to and from primary residence and the CCOE facility. Mileage
incurred to transport patient to hospital, companion traveling to/from hospital while member
is hospitalized will also be covered.
Lodging: The Plan will provide accommodations made by WebTPA for one room at a mid-market
chain hotel. Lodging will include nights for the timeframe of pre-operative testing through
initial recovery as determined by WebTPA. All additional charges are the responsibility of the
Patient.
Miscellaneous Expenses: The plan will provide Member $50.00 per diem (each full or part day) while
not admitted to the hospital.
Traveling Companion: $50.00 per diem (each full or part day) they are accompanying the Member
while receiving services from the CCOE.
Taxable Expenses: Some of the Travel Related Expenses are taxable income to the Member and/or
travel companion. The plan administrator will determine the taxable amount and report it to
your employer, and your employer will report the taxable amount on your Form W-2.
Documentation: In order for the plan administrator to accurately determine covered travel expense amounts
and taxation, you will be asked to submit receipts and, if traveling with a companion, you will be asked to
produce a Travel Companion Medical Necessity Form completed by your physician.

52
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
ALL OTHER TRAVEL RELATED EXPENSES ARE MEMBER RESPONSIBILITY
DIABETIC EDUCATION
The Plan provides outpatient diabetes self-management training (DSMT) to teach you to cope with and
manage your diabetes. The Plan may cover up to ten hours of initial DSMT by a certied DSMT provider. This
training may include one hour of individual training and up to nine hours of group training. You may also
qualify for up to two hours of follow-up training each year if it takes place in a calendar year after the year you
got your initial training.
This training is for covered enrollees who are at risk for complications from diabetes. You must have a written
order from a physician or other healthcare provider.
DIALYSIS
DURABLE MEDICAL EQUIPMENT
Durable medical equipment, supplies, and appliances include:
• Diabetic Supplies. If diabetic supplies are obtained through an in-network pharmacy, they will be
covered under the pharmacy/Prescription Drugs benet as described in the Prescription Benets
tables of the Schedule of Benets. If not, they will be covered as provided under the Durable Medical
Equipment section in the Schedule of Benets.
• Foot orthotics are covered for the treatment of diabetic foot disease and severe peripheral vascular
disease only. Foot orthotics are not covered in any other situations. Arch supportsare not covered.
• Original tting, adjustment and placement of orthopedic braces, casts, splints, crutches, cervical
collars, head halters, traction apparatus, orthotics, sleep apnea equipment or prosthetic appliances
to replace lost body parts or to aid in their function when impaired.
• Articial limbs, eyes, or other prosthetic appliances required for replacing natural limbs, eyes or other
body parts lost or removed while the person is covered by this Plan. Replacement of articial eyes,
limbs or other prosthetic appliances if required due to a pathological change in patient’s physical
condition; or if required due to the growth of a child; or if replacement is less expensive than repair of
existing prosthetic appliances.
• Initial prescription contact lenses or eyeglasses, including the examination and tting of thelenses,
to replace the human lens lost through intraocular surgery performed while covered under the Plan.
• Wigs and articial hairpieces following radiation or chemotherapy, or when due to a pathological
change in the body, covered under the Wig section of the Schedule of Benets and subject to a
$1,000 annual maximum.
• Blood or other uids injected into the circulatory system. Expenses for blood salvage (i.e., blood
donated by a covered person for his/her own use) will also be covered only if a surgery is scheduled
for which there is reasonable chance that blood will be required.
• Sterile surgical supplies after surgery.
• Maternity support hose, only when prescribed by a physician.
• Jobst garments.
• Oxygen and rental of equipment required for its use.
• Colostomy supplies.
• Orthopedic shoes are covered if they are an integral part of a leg brace or if a physician or
professional provider has ordered that orthopedic shoes be individually designed for correction or
support of a deformity. If such correction or support is accomplished by modication of a mass-
produced shoe, then the covered expense will be limited to the cost of the modication. The
covered expense will not include the original cost of the shoe.
• Diabetic shoes are covered if the member has a diagnosis of diabetes and has any of the following:

53
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
foot deformity; (2) history of pre-ulcerative calluses; (3) history of previous ulceration; (4) peripheral
neuropathy with evidence of callus formation; (5) poor circulation; or (6) previous amputation of the
foot or part of the foot. Limit is 1 pair per year.
Rental Charges
The Plan covers a portion of the charges for the rental of medically necessary durable medical and surgical
equipment and accessories needed to operate it (not to exceed the purchase price of the equipment). See
Schedule of Benets for more complete information.
Purchase Charges
The Plan will pay a percentage of the cost of the initial purchase of durable medical equipment and
accessories needed to operate it if the utilization review manager determines that long-term use is planned
and the equipment cannot be rented, or purchase is more cost eective than rental.
Repair and Replacement
The Plan covers charges for repair of purchased equipment and accessories. Replacement of purchased
equipment is covered only if the utilization review manager determines that it is warranted due to changes in
an enrollee’s physical condition or if it is more cost eective than repair or rental of like equipment.
Specic Limitations
Pre-certication required for all durable medical equipment or repair with billed charges of $2,000 or
more, and all CPM devices, and Dynasplints (regardless of cost).
The Plan covers durable medical and surgical equipment that meets all of the following requirements. The
equipment must:
1. be recommended for you by your physician;
2. be able to stand repeated use, and be of a type that could normally be rented and used by
successive patients;
3. be primarily and customarily used to serve a medical purpose (examples of items that do not
primarily and customarily provide a “medical purpose” include, for example, humidiers, exercise
equipment, gel pads, water mattresses, heat lamps);
4. generally not be useful to a person in the absence of an injury or illness;
5. be appropriate for home use; and
6. meet the guidelines used by the Center for Medicare and Medicaid Services (CMS), the agency that
administers the Medicare, Medicaid and Child Health Insurance Programs.
The does not cover charges for more than one item of durable medical equipment for the same or
similar purpose.
EMERGENCY/URGENT CARE SERVICES
If an enrollee receives emergency medical care for an accidental injury or medical emergency the Plan will
cover physician services in the emergency room, urgent care center, oce, or hospital outpatient department
including x-rays, MRIs, laboratory, and machine diagnostic tests. Emergency room visits are only covered
when there is an emergency medical condition. Please refer to the Schedule of Benets section of this
document for the amount of coverage provided and deductible provision for emergency care. If an Urgent
Care Center is available and you choose to use its services for your care, the physician charges may be

54
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
paid as oce visits, or as an ER visit. This is dependent on the facility and its billing process, the treatment
diagnosis and services rendered. Facility charges for oce visits are not covered.
GENETIC TESTING
Genetic panel testing for hereditary breast and ovarian cancer risk may include one or more of any
combination of the following genes: ATM, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6,
NBN, NF1, PALB2, PMS2, PTEN, RAD51C, RAD51D, STK11, TP53. The Plan does not cover genetic testing
panels for hereditary breast and ovarian cancer risk that include any genes outside of those listed genes.
Genetic testing for hereditary breast and/or ovarian cancer gene mutation(s) is not covered in members who
have received an allogeneic bone marrow transplant if only blood or buccal samples are available (but may
be covered if broblast culture is available).
HEARING CARE
Services for hearing care assistance include:
1. audiometricians;
2. hearing specialists;
3. hearing aids and repairs (does not require PPO Network utilization but is subject to separate limits, see
Schedule of Benets); and
4. surgically placed devices such as cochlear implants upon pre-certication by the Plan’s utilization
review manager.
HOME HEALTH CARE
The Plan provides benets for Home Health Care if provided by an appropriately licensed entity staed by
licensed and credentialed home health care professionals meeting all state and Federal requirements.
The Home Health Care benet provides for medically warranted continued care and treatment after
discharge from a hospital and must be in lieu of hospitalization.
Specic Limitations
Limited to 120 visits per Plan Year.
Home Health Care does not include charges made for:
1. services or supplies that are not a part of the Home Health Care Plan;
2. services of a person who usually lives with you or is a member of you or your spouse’s family;
3. transportation; or
4. custodial care.
HOSPICE CARE
Hospice care is an alternative to hospitalization. It is care that oers a coordinated program of home care
and inpatient care for a terminally ill patient and the patient’s family. The program provides supportive
care to meet the special needs from physical, psychological, spiritual, social, and economic stresses often
experienced during the nal stages of life and during dying and bereavement. For purposes of this Plan, a
“terminally ill patient” is someone who has a life expectancy of approximately six months or less, as certied
in writing by the physician in charge of the patient’s care and treatment, the hospice physician can approve

55
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
further care beyond the initial certied approval.
The Plan provides benets for covered charges for:
1. services of a physician; and
2. healthcare services as an inpatient or at home, including part-time nursing care, part-time or
intermittent home health care aid, use of medical equipment, rental of wheelchairs, and hospital- type
beds; and
3. emotional support services and physical and chemical therapies.
4. Respite Care:
• up to 5 days, may be taken intermittently
• care can be at a certied hospice care facility or via in-home care.
Specic Limitations
The Plan only covers those services provided by a qualied hospice program that meets the standards of the
National Hospice Organization (NHO) and applicable state licensing requirements.
Hospice benets will not be provided for:
• Private duty nursing care
• Care performed by family members, relatives and friends
• Treatment to cure the member’s underlying illness
HOSPITAL, SKILLED NURSING FACILITY, AMBULATORY SURGERY CENTER
When this Plan refers to an inpatient, it means a person admitted as a bed patient to a hospital or skilled
nursing facility for treatment and charges made for room and board to the enrollee as a result of such
treatment. An outpatient is an enrollee who receives treatment while not admitted as a bed patient in a
hospital.
Payment for inpatient care is limited to semi-private room rate charges. If you voluntarily elect to occupy a
private room instead of a semi-private room, you are responsible for paying the dierence in cost between
the private room rate and the hospital’s most common semi-private room rate. There is one exception to
this rule: isolation or private room charges will be covered if a private room is essential due to the patient’s
severely compromised defenses against infection, due to a contagious disease, or otherwise medically
necessary to protect the patient’s life.
In order for the Plan to cover charges as those of a hospital, the institution must meet state and Federal
regulatory and credentialing guidelines.
INFERTILITY TREATMENT BENEFITS
This benet is only available to enrollees who are legally married to a person of the opposite sex. If sterilization
and/or tubal ligation procedures have been reversed, infertility treatment and associated medication are not
covered under the Plan. There is a lifetime maximum payable benet for infertility benets that is set forth in
the Schedule of Benets.
Infertility treatment benets are provided only to employees and their spouses. Infertility treatment benets
are not provided for dependent children regardless of the marital status of that dependent child.

56
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
MATERNITY AND OBSTETRIC BENEFITS
Under the Plan, pregnancy-related and obstetric expenses are covered in the same way as medical expenses
for illness or injury, except that full coverage is provided only to employees and their spouses. There is no
coverage for maternity benets or complications due to pregnancy for dependent daughters regardless of
their marital status.
Preventive benets (including those specic to maternity) are covered based on Federal guidelines of the
Aordable Care Act. Preventive benets are covered for dependent daughters the same as for employees and
spouses. See Preventive Care Services section.
The Plan provides coverage for in-network midwives (or with an Unavailable Services Request Form approved
by the plan administrator) who are certied nurse midwives who have met the graduate training standards of
the American College of Nurse Midwives and are licensed to practice in that state. The majority of qualied
midwives practice in a hospital, or in a free standing or hospital based facility that provides a “home-like”
atmosphere for childbirth. A midwife often attends childbirth, or a physician may assist a midwife. The midwife
must meet all state licensing requirements and provide proof of liability insurance that must be submitted
with the claim to WebTPA. The Plan will not pay for nor reimburse for midwife services if no proof of
liability insurance is provided even if the state does not require liability insurance.
The Plan provides facility coverage for delivery in PPO facilities only. The only exception is for emergency
deliveries in facilities that conform to American Medical Association (“AMA”) guidelines.
The Plan provides coverage for the covered employee’s delivery complications or the employee’s covered
spouse’s delivery complications, regardless of who delivers the child and/or the location of the birth.
Inpatient expenses that are incurred by a newborn child during hospitalization for delivery will be considered
incurred by the newborn and thus subject to a separate deductible and out-of-pocket maximum at birth of
the baby. A newborn child who is an eligible dependent must be enrolled in the Plan within 30 days of the date
of birth (as extended by the temporary HIPAA special enrollment deadline extension due to the COVID-19
pandemic described in Appendix F) in order to be covered under the Plan and in order to have the child’s
incurred expenses be eligible for coverage by the Plan.
MENTAL HEALTH SERVICES
The Plan covers physician and other authorized professional provider charges for inpatient and partial
hospitalization of mental health disorders, and for counseling services for marital and family conicts, and
social adjustment.
Residential care and treatment are not covered unless treatment is considered in-patient, is in-network, and
approved through the utilization review manager. Intensive outpatient programs and partial hospitalization
programs are not covered unless treatment is in-network and approved through the utilization review manager
(except if service is not available in-network and member has an Unavailable Services Request Form approved
by the plan administrator).
NUTRITIONAL COUNSELING
Five visit annual limit applies to all plan options. Additional visits may be authorized by the utilization review
manager.
ONCOLOGY
ORGAN/TISSUE TRANSPLANT
A “recipient” is a person who receives a body organ or tissue transplant. A “donor” is a person, either living or
deceased, who donates tissue or a body organ for transplant.
In order to receive benets under this provision, the type of transplant must not be experimental or

57
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
investigative and must be from a human donor.
Enrollees may pursue listing at multiple sites. Evaluations are based on medical appropriateness reviews
and are generally limited to one, and so the Plan will only pay for one evaluation and the enrollee would be
responsible for any additional evaluations (unless the medical appropriateness review specically allows
coverage of an additional evaluation).
Recipient Benets
If an enrollee is receiving a transplant, the Plan covers inpatient hospital and professional services and
supplies furnished to the recipient during the hospital stay in which the transplant is performed.
Benets for bone marrow/stem cell transfer transplants include coverage for chemotherapy and radiation
therapy that is a part of the inpatient care under this provision.
Donor Costs for Enrollees
The Plan also provides benets for the medical expenses of enrollees in this Plan who act as organ or tissue
donors or are evaluated as a potential donor, but only if the recipient is an enrollee. The Plan will cover the
evaluation, removal and transport of the donor organ or tissue, including expenses of the surgical/harvesting
team. The Plan will also cover donor testing and typing of a potential donor, if the potential donor is an
enrollee in the Plan. The Plan covers medically necessary expenses of a donor who is not an enrollee in the
Plan who donates to a covered enrollee. Pre-certied services and charges are paid only on the matched
donor.
PREVENTIVE HEALTH CARE
• All preventive items and services (collectively referred to as “preventive services” below) listed in
26 CFR §54.9815-2713T, or any successor regulation or statute. Such preventive services include the
following:
(i) Evidence-based items or services that have in eect a rating of A or B in the current
recommendations of the United States Preventive Services Task Force with respect to the
individual involved;
(ii) Immunizations for routine use in children, adolescents and adults that have in eect a
recommendation from the Advisory Committee on Immunization Practices of the Centers
for Disease Control and Prevention with respect to the individual involved (for this purpose,
a recommendation from the Advisory Committee on Immunization Practices of the Centers
for Disease Control and Prevention is considered in eect after it has been adopted by
the Director of the Centers for Disease Control and Prevention, and a recommendation is
considered to be for routine use if it is listed on the Immunization Schedules of the Centers for
Disease Control and Prevention);
(iii) With respect to infants, children and adolescents, evidence-informed preventive care and
screenings provided for in comprehensive guidelines supported by the Health Resources and
Services Administration; and
(iv) With respect to women, to the extent not described in (1) above, evidence informed
preventive care and screenings provided for in comprehensive guidelines supported by the
Health Resources and Services Administration (“HRSA”).
Preventive services do not include any items or services specied in any recommendation or
guideline described in (i)-(iv) above after the recommendation or guideline is no longer described
in (i)-(iv) above. Preventive health care may be subject to the same pre-certication, utilization
review, and care management techniques as other Plan covered services.

58
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
A list of the preventive services that are covered by the Plan can be found at https://www.
healthcare.gov/preventive-care-benets/ and in Appendix A. Appendix A reects the
preventive services available as of the date listed in Appendix A. If there is any conict between
the list in Appendix A and the provisions of this Preventive Health Care (Wellness) section, the
provisions of this section are followed.
If received from an in-network provider, the preventive services covered under this section are
covered with no cost-sharing required on your part (that is, no co-payment, no co-insurance,
and no deductible; this is often referred to as “rst-dollar coverage”). If a preventive service is
provided as part of an oce visit and the oce visit is not itself a preventive service covered
under this section, the following rules apply: (1) if the preventive service is billed separately from
the oce visit, then any applicable cost-sharing requirements will apply to the oce visit (such
as a copayment); (2) if the preventive service is not billed separately from the oce visit and the
primary purpose of the oce visit is the delivery of such preventive service, then no cost-sharing
will be imposed; and (3) if the preventive service is not billed separately from the oce visit and
the primary purpose of the oce visit is not the delivery of such preventive service, then any
applicable cost-sharing requirements will apply to the oce visit.
Contraceptive management: As provided in (iv) above, the Plan provides rst-dollar coverage for
preventive care and screenings provided for in the HRSA guidelines for women’s preventive care.
The HRSA guidelines include annual well-woman visits and FDA- approved contraceptives. Thus,
rst-dollar coverage is provided for an annual well-woman visit and FDA-approved contraceptives
(including insertion and removal of implantable contraceptives). Oce visits for contraceptive
management, generally, will not be covered as preventive services and, thus, will be subject to
any applicable copayment (as set forth in the Schedule of Benets).
• Colorectal cancer screening for adults age 45 and over at the screening intervals recommended by
the US Preventive Services Task Force based on test type and individual risk level: colonoscopy or
sigmoidoscopy (including bowel prep kit, anesthesia, any required specialist consultation prior to the
screening procedure, and any pathology exam on a polyp biopsy); or fecal occult blood testing. Colon
cancer testing for diagnostic purposes, as opposed to general screening, is not preventive care
and so cost-sharing requirements will apply.
SKILLED NURSING FACILITIES
In order for the charges to be covered under the Plan, the Skilled Nursing Facility must meet all of the
following requirements:
1. The Skilled Nursing Facility must be licensed to provide and be engaged in providing 24- hour- per-
day professional nursing services on an inpatient basis for persons recovering from injury or disease
by a registered nurse (R.N.) or by a licensed practical nurse (L.P.N.) under the direction of an R.N.
2. Physical restoration services must be provided to assist patients to reach a degree of body
functioning to permit self-care in essential daily living activities.
3. A Skilled Nursing Facility connement must take place within 14 days from a hospital discharge and
must represent care for the same condition for which the hospitalization was required.
4. The care provided must not be custodial in nature.
5. The Skilled Nursing Facility must maintain a complete record on each patient.
6. The Skilled Nursing Facility must have an eective utilization review plan.
SUBSTANCE ABUSE AND CHEMICAL DEPENDENCY TREATMENT
The Plan covers physician and other authorized professional provider charges for substance abuse and

59
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
chemical dependency treatment.
Residential care and treatment are not covered unless treatment is considered in-patient, is in-network, and
approved through the utilization review manager.
SURGICAL SERVICES
THERAPEUTIC CARE
Physical Therapy
The Plan provides coverage for Physical Therapy within certain limitations stated in the Schedule of Benets
section of this document.
A prescription from your MD/DO is required.
Registered Physical Therapist services are covered whether performed in a clinical or home setting.
Occupational Therapy
The Plan provides coverage for Occupational Therapy within certain limitations stated in the Schedule of
Benets section of this document. Occupational Therapy may be covered whether performed in a home or
clinical setting if the provider of such services is a Registered Occupational Therapist (OTR) or a Certied
Occupational Therapy Assistant (COTA). Sensorimotor therapy, cognitive therapy, and psychosocial therapy
are services under the umbrella of Occupational Therapy. Services that are recreational in nature are not
covered.
A prescription from your MD/DO is required.
OTR and COTA services are covered whether performed in a clinical or home setting.
Speech and Language Pathology Therapy
The Plan provides coverage for Speech Therapy with certain visit limitations stated in the Schedule of
Benets contained in this document. Attempting to improve public presentation skills with the assistance of a
Speech and Language Pathologist is not considered a covered expense under this Plan.
A prescription from your MD/DO is required.
Vision Therapy
The Plan provides coverage for orthoptic/pleoptic training.
A prescription from your MD/DO is required.

60
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Description - Dental
Aetna Dental is the preferred provider organization (PPO) for all dental benet services. To avoid a reduction
in benets and potential excess charges of U&C (Usual, Reasonable, and Customary), you must use an in-
network provider. By utilizing in-network providers of the dental PPO Network, dental costs will be lower to both
the Plan and to you.
By choosing not to use an to which you have access, your benets are similar to the
participating provider program except for three major dierences:
1. For in-network, preventive care is paid at 100% of charges with no deductible applied. U&C applies
when using out-of-network providers.
2. There is a separate and additional deductible for services obtained from out-of-network providers.
See the Schedule of Benets for specic deductible limits for in-network providers and out-of-network
providers.
3. After deductibles have been met, charges for restorative dental care will be paid at the percentage
identied in the Schedule of Benets. This percentage of payment is lower for out-of-network
providers.
If you elect to utilize the services of an out-of-network provider, your covered benets will be paid at a lower
percentage rate than with participating providers. Also, you will be responsible for charges in excess of U&C.
The dental plan pays up to a maximum amount based on U&C per Plan Year for individual coverage and
family coverage. Please refer to the Schedule of Benets in this document for the Plan’s percentage of
coverage.
Dental Care expenses are paid in accordance with the Schedule of Benets as follows:
Preventive Care
1. Routine oral examinations and prophylaxis (cleaning of teeth), but not more than two times in a Plan
Year;
2. One set of bitewing x-rays per Plan Year;
3. Topical application of uoride, but not more than two times per Plan Year; and
4. Full-mouth x-rays or panorex limited to once every three Plan Years.
Restorative Care
1. Amalgam, silicate, acrylic, resin, synthetic porcelain and composite lling restorations to restore
diseased or fractured teeth;
2. Root canal therapy;
3. Diagnostic x-rays;
4. Pit and ssure sealant on permanent molars and bicuspids without prior restorations;
5. Space maintainers that replace prematurely lost teeth for dependent children under age 19;
6. Periodontal scaling and root planning;

61
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
7. Extractions;
8. Periodontal procedures (other than scaling and root planning);
9. Oral surgery;
10. General anesthesia when medically necessary;
11. Installation of crowns or xed bridgework (including inlays and crowns as abutments);
12. Initial partial or full removable denture (to include any adjustments during the six month period
following installation);
13. Replacement of an existing partial or full removable denture or xed bridgework by a new denture or
by new bridgework, or the addition of teeth to an existing partial removable denture or to bridgework;
and
14. Dental implants.
Dental Pre-Certication Requirements
Pre-certication requirements must be conrmed with the dental PPO Network provider. In-network provider
utilization and appropriate pre-certication protocol must be followed to minimize member responsibility
for these services. The Plan will defer to the PPO Network’s benet policies concerning pre-certication,
supporting documentation required in claim adjudication, and U&C amounts. For pre-certication please
contact Customer Service at 888-276-4732.
Payment Limits
There are annual individual and family limits on the amount of dental expenses covered under the Plan.
Please refer to the Schedule of Benets for the maximum payable benets and coverage percentages per
Plan Year.
Coverage Limits and Exclusions
The Plan does not cover, or limits coverage, for the following types of dental services:
1. Any dental charges in which treatment is started before the enrollee was participating in this Plan are
not covered.
2. Fees charged for infection control are not covered as a dental expense.
3. Temporary crowns or bridges are not covered.
4. Services or supplies that do not meet accepted standards of dental practice, including charges for
services or supplies that are experimental in nature are not covered.
5. Oral hygiene instruction and oral hygiene aids are not covered.
6. Cosmetic services, including teeth whitening and veneers are not covered.
See the Limitations and Exclusions section of this document for additional information.

62
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
ORTHODONTIA TREATMENT
The Plan provides coverage for orthodontia expenses as a percentage rate of the provider’s charges up to
a maximum stated amount per Plan Year as outlined in the Schedule of Benets. Payment for Orthodontia
services is also subject to the limitations outlined below.
Payment and Other Limitations
1. Payment by the Plan will begin when the dental PPO Network is notied of the banding date.
Subsequent payments will be made on a monthly basis as services are rendered and provider billing
is received during the course of treatment.
2. Enrollees are not eligible for Orthodontia benets after attaining 26 years of age.
3. The orthodontic lifetime maximum in eect at the time of banding is the orthodontic lifetime
maximum benet that will apply for these services.
4. If a person becomes ineligible for coverage under the Plan during the course of his or her treatment,
payments will end when the person is no longer eligible for coverage regardless of whether the
treatment is complete.
5. Payments by the Plan are on a monthly basis as services are rendered during the course of treatment
subject to age and benet limitations.
See the Limitation and Exclusions section of this document for additional information.

63
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Description - Vision
The Plan provides coverage for vision related diagnoses and treatments, including routine diagnostic
procedures, and the following necessary vision care services and expenses:
1. Eye examination;
2. Prescription eye glasses; and
3. Contact lenses.
Limitations
Vision care benets are covered at the same percentage rate as other medical benets, but there is a
maximum benet amount in each Plan Year. The Plan’s percentage rate of payment and maximum amount
payable for each covered enrollee is specied in the Schedule of Benets. (Annual maximum payable does
not apply to pediatric (under age 19) annual eye examination and one pair of standard, clear-lens, prescription
glasses per plan year per child.) The vision care benets do not include payment for non-prescription lenses.
Refractive Eye Surgery
Refractive eye surgery reshapes the cornea to redirect light rays so that they focus accurately on the retina,
reducing or eliminating the need for corrective lenses. Refractive surgery is used to correct myopia (near
sightedness), hyperopia (farsightedness), astigmatism (distorted vision). Refractive eye surgical procedures
are covered up to a lifetime maximum amount set forth in the Schedule of Benets. In order to be covered,
procedures must meet federal Food and Drug Administration (FDA) approval and guidelines. Covered
procedures include Radial Keratotomy (RK), Photorefractive Keratotomy (PRK), Laser In Situ Keratomileusis
(LASIK), and intracorneal rings.
Medical Vision/Eye Services
Medical diagnoses and treatments of the eye(s), including diagnostic procedures and retinal exams, apply to
the medical plan benets. By using a provider participating in the medical PPO Network, medical costs will be
lower to both the Plan and to you.

64
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Description – Prescription Drugs
This benet only covers services/supplies received directly from Express Scripts, Inc.
or from a pharmacy contracted with Express Scripts, Inc.
This section describes the prescription benets provided by your Plan. Please refer to the Schedule of
Benets for the specic payment percentages, maximum amounts payable, and co-payment requirements.
The following are covered:
• Prescription drugs, which under applicable state law, may only be dispensed by written prescription
of a physician or dentist and are included in the formulary of your pharmacy benet manager (see
below).
• Diabetic supplies, including syringes and test strips.
• Compounds with National Drug Code (NDC) ingredients. (Compounds without NDC ingredients are
not covered.)
Pharmacy Benet Manager
The Plan uses Express Scripts, Inc., (ESI) as its pharmacy benet manager (PBM) for the Plan’s prescription
drug benet.
Formulary, Pharmacy Levels and Drug Tiers
ESI uses a national preferred formulary. The formulary encourages patients to use clinically appropriate
medications while helping to manage costs. A formulary is a list of medications in dierent therapy classes
used to categorize or group the drugs on the formulary. The classes group drugs which are considered
similar by the disease they treat or by the eect they have on the body. Prescription drug coverage under the
Plan is oered through two dierent pharmacy levels: 30-day Retail; and 90-day Mail Order and Walgreens
Smart90 retail program. Your copayments will be lowest if you use 90-day Mail Order or the Walgreens
Smart90 retail program. (The Walgreens Smart90 retail program is not available for employees (and their
dependents) stationed in the U.S. territories.)
If you choose to purchase long-term maintenance medication at retail pharmacies rather than via mail order,
after three purchases of the medication, you will have to pay the dierence in the cost between the price
of the medication at the retail pharmacy and the price of the medication charged by the mail order home
delivery program (and this dierence will not accrue toward your Plan Year out-of-pocket maximums or
deductibles). For a list of long-term maintenance drugs that are subject to this rule, please contact the ESI
Member Services Department at 800-841-5396. (The extra charge for using a retail pharmacy for a long-term
maintenance medication will be waived for employees (and their dependents) stationed in the included U.S.
territories.)
Within each category, there are three drug tiers, or levels:
Generic (Tier 1): A generic drug is a safe, eective drug approved by the U.S. Food and Drug Adminis-
tration (FDA) that also costs less. You pay the lowest copayment for generic drugs.
Brand (Tier 2): Formulary brand (or preferred) drugs are brand name drugs. The copayment for for-
mulary brand drugs is higher than it is for generic drugs.

65
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Non-formulary
(Tier 3):
Non-formulary (or non-preferred) drugs are brand name drugs that are not covered
under the ESI national preferred formulary. The copayment for non-formulary drugs is
higher than it is for formulary brand (preferred) or generic drugs.
The ESI formularies are developed to be clinically sound and cost eective. Clinical appropriateness is the
foremost consideration; however, the prescribing has the nal decision regarding a patient’s drug
therapy.
If your prescribing physician has allowed a generic substitution and you nevertheless choose the brand name
drug, you may be required to pay the cost dierence between the generic and the brand (in addition to your
co-payment).
Prescription Drug Pre-Certication Requirement
Some drugs require pre-certication through the PBM (ESI) when obtaining prescription medication through
your retail pharmacies or mail order program. Select medications in the following therapeutic categories are
subject to review, pre-certication, and/or restrictions by the Plan:
1. Anti-emetics
2. Anti-infectives (such as for hepatitis C, etc.)
3. Benign prostatic hyperplasia therapy
4. Blood modifying agents (such as for myeloid stimulants, immune globulins, etc.)
5. Bone conditions therapy
6. Cancer therapy
7. Cardiovascular agents (such as for cholesterol, heart failure, etc.)
8. Chelating agents (such as for iron overload, lead toxicity, etc.)
9. Diabetes therapy
10. Duchenne Muscular Dystrophy therapy
11. Endocrine disorders therapy (such as growth hormones, androgens/anabolic steroids, etc.)
12. Eye conditions therapy (such as for glaucoma, etc.)
13. Fabry disease therapy
14. Fertility agents
15. Gastrointestinal agents
16. Gout therapy
17. Hemophilia therapy
18. Hereditary angioedema therapy
19. Inammatory/Immune disorders therapy (such as for lupus, multiple sclerosis, rheumatoid arthritis, etc.)
20. Inherited rare disease therapy
21. Kidney disease therapy
22. Mental/neurological disorder therapy
23. Metabolic disorders therapy
24. Migraine headaches therapy
25. Muscle relaxants
26. Narcolepsy therapy (such as CNS stimulants)
27. Neuromuscular conditions therapy (such as Botox)
28. Osteoarthritis therapy

66
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
29. Overactive bladder therapy
30. Pain medications (such as opioid analgesics)
31. Pulmonary medications (such as for asthma, COPD, allergy, etc.)
32. Sexual disorder therapy (such as for erectile dysfunction)
33. Sickle cell disease therapy
34. Skin conditions therapy
35. Sleep disorder therapy (such as hypnotic agents)
36. Substance abuse therapy
37. Transplant related agents
38. Weight loss therapy (such as appetite suppressants)
39. Wilson’s disease therapy
40. Women’s health therapy
41. Wound care agents
The above list is subject to change at any time. Please call Express Scripts’ Member Services, (800) 841-5396,
or visit Express Scripts’ website www.express-scripts.com for further details.
Step Therapy Program
The Plan participates in Express Scripts’ Step Therapy program under which certain high cost or brand name
drugs (“Step-Therapy Drugs”) are not covered by the Plan unless:
1. You rst try one or more less costly drugs (which may include over-the-counter drugs) that
are normally available and used to treat a particular medical condition, and your doctor
certies that these less costly drugs are not eectively treating your condition or other
medical reasons why the less costly drugs cannot or should not be used to treat your medical
condition; or
2. Your doctor certies to the Plan the medical reasons for your use of the Step-Therapy Drugs in
lieu of less costly drugs that are normally available and used to treat this condition.
If you are taking a Step-Therapy Drug, you or your doctor will receive a letter explaining this program. If you
receive a letter, consult with your doctor immediately concerning your use of Step-Therapy Drugs. Do not
stop taking any medication prescribed by your doctor without rst consulting your doctor.
Please call Express Scripts’ Member Services, (800) 841-5396, or visit Express Scripts’ website
www.express-scripts.com for further details.
Medical Channel Management Program
Certain infusion or injectable specialty drugs are available through the Medical Channel Management
Program and are only accessible through the pharmacy benet and are subject to pre-certication
requirements administered by Express Scripts. Accredo Specialty Pharmacy will contact all members
impacted by letter and by phone call to educate them about the coverage of these drugs.
If your provider ordered an infusion or injectable drug for you that qualies for the Medical Channel
Management Program through Express Scripts and you do not obtain the drug through Accredo Specialty
Pharmacy, you will be required to transfer the prescription to Accredo Specialty Pharmacy. If you continue
to purchase your specialty drugs from your provider’s oce, infusion center, or another pharmacy, you may
be responsible for their full cost. When you or your provider order a covered specialty drug through Accredo,
your out-of-pocket cost will be limited to the applicable prescription drug co-payment instead of the 20% co-

67
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
insurance applicable through the medical benet for outpatient services. (This program also includes drugs
that might qualify for $0 SaveonSP Specialty Drugs Program oered by Express Scripts).
In order to provide you with sucient time to transfer your prescription to Accredo Specialty Pharmacy, you or
your provider may submit a pre-certication request through the utilization review manager (Adventist Health
Benet Administration) for coverage of one additional prescription from your current provider through the
medical benet. In addition, if you have an extenuating medical condition that prevents you from transitioning
the prescription to Accredo Specialty Pharmacy, you may be granted an override and continue on your
coverage through the medical benet as long as there is an approved medical reason to not transition.
Services such as infusion drugs or injectables accessed through the medical benet are subject to 20% co-
insurance and the pre-certication requirements through Adventist Health Benets Administration, and these
services would not qualify for the $0 SaveonSP Specialty Drugs Program oered by Express Scripts.
The list of drugs subject to the Express Scripts’ Medical Channel Management Program may change, and
you or your provider should contact Accredo Specialty Pharmacy to check a drug’s availability before you ll a
prescription for a specialty drug.
If you have questions about this program or need support transitioning your prescription to Accredo Specialty
Pharmacy, please reach out to Adventist Health Benets Administration at 888-276-4732 for guidance.
(The Medical Channel Management Program is not available for employees (and their dependents) stationed
in the U.S. territories. If you are stationed in an included U.S. territory, then you and your eligible dependents
may purchase covered infusion or injectable specialty drugs from your medical provider or infusion center,
but such drugs will be subject to the cost sharing described in the Medical Benets Schedule of Benets for
medical outpatient services.)
Preventive Prescription Drugs
Preventive prescription drugs include the prescription drugs listed in (or included in the services listed in)
26 CFR § 54.9815-2713, or any successor regulation or statute. Such preventive prescription drugs include
prescription drugs included in the following:
(i) Evidence-based items or services that have in eect a rating of A or B in the current recommendations
of the United States Preventive Services Task Force with respect to the individual involved;
(ii) Immunizations for routine use in children, adolescents and adults that have in eect a
recommendation from the Advisory Committee on Immunization Practices of the Centers for Disease
Control and Prevention with respect to the individual involved (for this purpose, a recommendation
from the Advisory Committee on Immunization Practices of the Centers for Disease Control and
Prevention is considered in eect after it has been adopted by the Director of the Centers for Disease
Control and Prevention, and a recommendation is considered to be for routine use if it is listed on the
Immunization Schedules of the Centers for Disease Control and Prevention);
(iii) With respect to infants, children and adolescents, evidence-informed preventive care and screenings
provided for in comprehensive guidelines supported by the Health Resources and Services
Administration; and
(iv) With respect to women, to the extent not described in (i) above, evidence informed preventive care
and screenings provided for in comprehensive guidelines supported by the Health Resources and
Services Administration.
Preventive prescription drugs will not include any items or services specied in any recommendation or
guideline described in (i)-(iv) above after the recommendation or guideline is no longer described in (i)-
(iv) above. See Appendix A for additional information about specic preventive care services and drugs.
Preventive prescription drugs may be subject to the same pre-certication and step therapy requirements as
other covered prescription drugs (described above).

68
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Smoking cessation drugs that are prescribed by a physician and approved by the plan administrator are
covered with no copay and no deductible (if received from an in-network pharmacy).
If prescribed by a physician and received directly from ESI or a pharmacy contracted with ESI, the preventive
services covered under this section are covered with no cost-sharing required on your part (that is, no co-
payment, no co-insurance, and no deductible; this is often referred to as “rst-dollar coverage”).

69
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Description – Complementary and Alternative
The Plan recognizes the National Center for Complementary and Integrative Health (NCCIH) as the authority
in dening complementary and alternative medicines (CAM). CAM, as dened by the NCCIH, is a group of
diverse medical and healthcare systems, practices, and products that are not presently considered part of
conventional medicine. Coverage for CAM is limited under the Plan. Coverage under the Accelerate Plan
is limited to Chiropractic Treatment, Therapeutic Massage Therapy, and Acupuncture Treatment. Coverage
under the Access Plan is limited to Chiropractic Treatment. All other CAM therapies, services, tests, laboratory
tests, procedures, products, and practices are not covered under the Plan.
Chiropractic Treatment
The Plan limits chiropractic treatment coverage to manipulation (subluxation, whether performed manually
or mechanically) of the spine. Certain maximums are stated in the Schedule of Benets section of this
document.
Services other than chiropractic manipulative treatment (i.e. hot or cold packs or supplies, muscle stimulation)
are not covered. Patient is responsible for these charges. Covered oce visit and x-ray charges during
chiropractic treatment sessions are limited to one eligible charge per Plan Year.
Enrollees under the age of 10 are not eligible for chiropractic benets.
Massage Therapy
Based on Benet Plan Election, Massage Therapy may not be a covered benet.
Massage therapy has both a maximum allowable charge and a maximum number of visits. Claims will not
be considered for payment unless they include Rendering Provider name, address and phone; Tax ID; a copy
of the therapist’s current license if not already on le; procedure code; patient name and enrollee’s Plan ID
number; length of visit (number of minutes); and date of service. CPT 97124 is the only allowable procedure
recognized under the massage therapy benet. A qualifying therapeutic massage will be a minimum of 30
minutes with services rendered in a private clinical setting. Please see the Schedule of Benets for specic
coverage and limitations.
Massage therapy must be provided by a licensed massage therapist (LMT) per regulatory requirements of the
state in which services were rendered. If your massage therapist is a new provider, your submitted charges
will be denied unless you provide a copy of the therapist’s current license. If your massage therapist practices
in a state, county, and/or city which does not have licensing requirements, the Plan may require additional or
alternative information concerning the massage therapist as a condition prior to paying Plan benets.
Enrollees under the age of 18 are not eligible for massage therapy benets.
Acupuncture Treatment
Based on Benet Plan Election, Acupuncture Treatment may not be a covered benet.
The Plan provides coverage for acupuncture treatment within certain limitations stated in the Schedule of
Benets section of this document. Acupuncture treatment may be covered when performed in a clinical
setting and by recognized providers including physicians, osteopaths, and non-physician acupuncturists who
have met all state license requirements. See the Schedule of Benets that describes the applicable visit limits
and co-insurance amounts.
Enrollees under the age of 18 are not eligible for acupuncture benets.

70
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Limitations and Exclusions
In addition to the exclusions described elsewhere in this Plan, the following services, procedures and
conditions are not covered by the Plan, even if otherwise medically necessary, even if they relate to a
condition that is otherwise covered by the Plan, or even if they are recommended, referred, prescribed or
provided by a physician, professional provider, including an in-network provider and/or in-network facility.
Coverage is not provided for the following charges or expenses:
1. Abortion (also referred to as termination of pregnancy), except where the pregnancy poses signicant
threats to the pregnant woman’s life or serious jeopardy to her health, where there are severe
congenital defects incompatible with life carefully diagnosed in the fetus, or where the pregnancy
resulted from rape or incest. Consistent with Seventh-day Adventist Church teachings, abortions for
reasons of birth control, gender selection, or convenience are not condoned by or covered by the
Plan. Care management sta are available to consult with a pregnant member and her physician
about these issues and to ensure that these Plan requirements for coverage are met in any given
situation.
2. Apolipoprotein E for Risk Assessment and Management of CV Disease
3. Biofeedback.
4. Career or Financial Counseling Services (wellness program participants can access goal setting,
tracking, educational content and fee-based nancial services via the wellness platform).
5. Charges for Missed Appointments.
6. Complementary and Alternative Medicine that is not specically and expressly covered by the Plan.
The Plan recognizes the National Center for Complementary and Integrative Health (NCCHI as the
authority in dening complementary and alternative medicines (CAM). CAM, as dened by the NCCHI,
is a group of diverse medical and healthcare systems, practices, and products that are not presently
considered part of conventional medicine. Coverage for CAM is limited under the Plan. The exceptions
are limited to acupuncture therapy, massage therapy, and chiropractic treatment in the Accelerate
Plan and limited to chiropractic treatment in the Access Plan. All other CAM therapies, services, tests,
laboratory tests, procedures, products, and practices are not covered under the Plan.
7. Complications from, or expenses incidental to or incurred as a direct consequence of, a treatment,
service, or supply that is excluded from coverage under this Plan.
8. Custodial Care and Services. The Plan does not cover custodial care and services related to custodial
care.
9. Dopamine Transporter Imaging Single-Photon Emission Computed Technology (DAT-SPECT)
10. Elective surgeries for preventive reasons (there are exceptions for prevention of certain cancers with
pre-certication).
11. Electrostimulation and electromagnetic therapy for wound care.
12. Experimental Services and Procedures. Except as permitted by participation in an approved clinical
trial, the Plan does not cover procedures, services, drugs or other supplies that are experimental or
still under clinical investigation. A procedure is considered to be experimental if it is generally deemed
so by medical professionals, the Food and Drug Administration, the National Institutes of Health or by
Medicare and/or Medicaid guidelines.
13. Extracorporeal shock wave therapy for plantar fasciitis.

71
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
14. First Aid Supplies.
15. Genetic testing panels. The Plan does not cover genetic testing panels for hereditary breast and
ovarian cancer risk that include any genes outside of the following genes: ATM, BRCA1, BRCA2, BRIP1,
CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PALB2, PMS2, PTEN, RAD51C, RAD51D, STK11,
TP53. Examples of genetic testing panels that are always excluded from coverage under the Plan
include, but are not limited to, the following: Ambry Genetics BreastNext panel test; Ambry Genetics
OvaNext panel test; GeneDx Breast/Ovarian Cancer panel test; and Myriad MyRisk Hereditary Cancer
panel test. Genetic testing for hereditary breast and/or ovarian cancer gene mutation(s) is not
covered in members who have received an allogeneic bone marrow transplant if only blood or buccal
samples are available.
16. Governmental Treatment. Except as otherwise provided by law, the Plan does not cover services
or supplies for care or treatment provided by the United States Government or any state or local
government when, without Plan coverage, the person would not be required to make payment.
17. Habilitative services.
18. Health Enhancement Programs, Life Style Center Programs, or any regimen designed to prevent
future health problems or to inuence adoption of a healthier lifestyle with a secondary objective of
providing necessary medical treatment, except as specically outlined in Lifestyle Programs section
of the Schedule of Benets. The Plan would encourage you to engage in relevant and appropriate
educational classes through your Health and Wellness benet.
19. High cost and specialty medications provided and billed by providers directly to the medical benet
that are available through the pharmacy benet’s Medical Channel Management program with
Express Scripts are not covered (except for the induction of therapy and those meeting site of care
medical necessity policy and approved by Adventist Health Benets Administration).
20. In Vivo Analysis of Colorectal Polyps
21. Job-related or immigration-related immunizations that are not considered preventive (see Appendix A
for details regarding preventive immunizations). Immunizations specic to mission trips and vacations
are not excluded.
22. Joint lubricant injections.
23. Late Claims. The Plan does not cover claims submitted more than one year after the date of the
service (as extended by the temporary deadline extension due to the COVID-19 pandemic described
in Appendix F).
24. Licensing Exams. The Plan does not cover physical examinations for the purpose of licensing or
regulatory requirements.
25. Medical Necessity. Coverage is not provided for services and supplies that are not medically
necessary. This rule does not apply to the Plan’s benets for preventive care. See specic preventive
care services in the addendum following the Schedule of Benets.
26. Military Injuries. The Plan does not provide benets for the illnesses and injuries of employees
returning from military leave under Uniformed Services Employment and Reemployment Rights
Act of 1994 (“USERRA”), if the Secretary of Veterans Aairs determines that the illness or injury was
incurred in, or aggravated during, performance of service in the Uniformed Services (as that term is
dened by USERRA).
27. Nail Debridement. The Plan does not cover nail debridement, except for enrollee with the diagnosis of
diabetes.

72
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
28. Non-emergency services/supplies received outside of the United States (except that employees
(and their dependents) stationed in the included U.S. territories may receive non-emergency covered
services/supplies in the included U.S. territories).
29. Non-prescription glasses or sunglasses.
30. Occupational Illness and Injury, The Plan does not provide coverage for charges or expenses for
injuries or sicknesses which are job, employment or work related, or for which benets are provided or
payable under any Workers’ Compensation or Occupational Disease Act or Law; or for which coverage
was available under any Worker’s Compensation or Occupational Disease Act or Law, regardless
of whether such coverage was actually applied for. If benets are paid and it is determined that an
enrollee is eligible to receive Workers’ Compensation for the same incident, illness or injury, the Plan
has a right to recover the benets paid under this Plan as described in the Recovery Rights provision.
As a condition of receiving benets on a contested Workers’ Compensation claim, enrollees must
consent to reimburse the Plan when entering into any settlement and compromise agreement or
at any Workers’ Compensation Division Hearing. The Plan reserves its right to exercise this right to
recover against a Member even though:
a. The Workers’ Compensation benets are in dispute or are made by means of settlement or
compromise or
b. No nal determination is made that the injury of illness was sustained in the course of or resulted
from employment or
c. The amount of Workers’ Compensation due is not agreed upon or dened by the Member or the
Workers’ Compensation carrier or
d. The medical or healthcare benets are specically excluded from the Workers’ Compensation
settlement or compromise
An enrollee will not enter into a compromise or hold harmless agreement relating to any work-related
claims paid by the Plan, whether or not such claims are disputed by the workers’ compensation
insurer, without the express written agreement of the Plan.
If satisfactory proof is furnished to the plan administrator that a person covered under a Workers’
Compensation law (or other like law) has made claim under such law in connection with a distinct
disease and no benet, award, settlement or redemption has been or will be made under that law
for such illness or injury, that illness or injury will be considered non-occupational for purposes of the
Plan.
31. Obesity Related Treatment (except as specically outlined in Lifestyle Programs section of the
Schedule of Benets), including Gastric (“Bariatric”) Surgery, or Prescription Drug Therapy for obesity
treatment. Upon review by the Plan’s utilization review manager and/or Express Scripts, exceptions
for those diagnosed with “Clinically Severe Obesity” or a signicantly high weight-to-height ratio
(“Body Mass Index”) and certain co-morbidities may be granted in certain medically necessary
situations. Whether a surgery exception will be granted will be decided by the utilization review
manager upon review of a completed bariatric precertication information request form and based on
the obesity surgery medical clinical policy published by Aetna, which provides the Plan’s PPO network
(contact the utilization review manager to request a copy of the policy). Any approved services will be
limited to in-network providers at the PPO network’s “Institutes of Quality” (IOQ).
32. Pelvic oor stimulation (non-implanted).
33. Plan Limits. The Plan does not cover charges in excess of the Plan limits.
34. Plastic, Reconstructive, Cosmetic Procedures and Surgeries. The Plan does not cover charges for
plastic, reconstructive, or cosmetic procedures, surgeries, services or supplies (whether or not for

73
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
psychological or emotional reasons) for the purpose of enhancing, altering, or improving personal
appearance or comfort. Limited exceptions may be obtained after rst being reviewed by the Plan’s
utilization review manager, to the extent that the surgery or procedure is necessary to: improve the
function of a part of the body that is malformed; or
a. correct a condition resulting from a severe birth defect; or
b. correct a condition that is a direct result of a disease or surgery performed to treat a disease or
injury (for example, breast reconstruction after mastectomy, as described in the Rights Under the
Women’s Health and Cancer Rights Act section); or
c. repair an injury, but only if the surgery is performed within twenty-four months of the accident
causing the injury.
35. Platelet rich plasma.
36. Pregnancies of dependent daughters are not covered, including medical complications resulting from
a pregnancy, except that the Plan provides benets for preventive care as required by federal law.
37. Prenatal and Parent Training Classes. (These are available to you through your Health and Wellness
Benets.)
38. Sexual Transformations and Trans Gender procedures.
39. Stem cell therapy for orthopedic procedures.
40. Surrogate Mothers. The Plan does not cover all services related to surrogate parenting, including
infertility testing and treatment, maternity care, birthing, hospitalization, professional services, etc.
41. Transportation and lodging except for ambulances and as described as part of the Cardiac Center of
Excellence (CCOE) Surgery Benet.
42. Telephone consultations and routine phone calls, except for formal telehealth visits that are a
substitute for an in-person oce visit with a provider and that are covered as described in the
Schedule of Benets.
43. Treatment by Household and/or Immediate Family Members. The Plan does not cover services of a
person who ordinarily resides in the home of the patient or services performed by a patient’s spouse,
parent, stepparent, child, or stepchild.
44. Usual, Reasonable, and Customary (U&C). The Plan does not cover expenses which exceed the Usual,
Reasonable, and Customary Charge (U&C) as determined by the plan administrator.
45. Viscosupplements (injectable).
46. Virtual scans and virtual physicals.
47. Vitamins, (except for physician prescribed vitamin B12 injections, Vitamin D, and prenatal care vitamin
supplements), dietary supplements and foods, herbs, minerals, nutritional supplements.

74
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Claims Procedures
CLAIM, APPEAL, AND EXTERNAL REVIEW DEADLINES ARE TEMPORARILY EXTENDED DUE TO THE
COVID-19 PANDEMIC, PER THE TERMS IN APPENDIX F.
Article 1 GENERAL CLAIM FILING PROCEDURES
Legally-compliant claims and appeals procedures are detailed in the numbered sections below. The
following general summary is oered for your convenience and ease of use: You must refer to the full
language in the numbered sections below for details regarding the claims/appeal process and how to
calculate your deadlines. The main Customer Service phone number is 888-276-4732, and they will route
you to the appropriate decision-maker (listed below). For prescription drug pre-certications, claims, and rst
appeals, please contact Express Scripts directly at 800-841-5396.
For pre-certication before you receive benets or while you are receiving benets:
For pre-certication for medical services Utilization review manager 888-276-4732
For pre-certication for prescription drugs Express Scripts 800-841-5396
For pre-certication for dental services WebTPA 888-276-4732
To submit a claim after you receive benets:
To submit a medical/dental claim WebTPA 888-276-4732
To submit a prescription drug claim Express Scripts 800-841-5396
If your claim is denied:
Deadline to le an appeal: 180 days from your receipt of a denial of the claim
Where to le your rst appeal:
Medical denials
(such as for no medical necessity)
Utilization review manager 888-276-4732
Non-medical denials
(such as for no eligibility for coverage)
WebTPA 888-276-4732
Prescription drug denials Express Scripts 800-841-5396
If your rst appeal is denied:
Deadline to request second review: Four months from your receipt of the denial of the appeal
Where to le your request for review of your denied appeal:
Medical denials
(such as for no medical necessity)
External review
(coordinated by the utilization review
manager)
888-276-4732
Nonmedical denials
(such as for no eligibility for coverage)
Plan administrator 888-276-4732
Prescription drug denials - involving med-
ical judgment (such as for no medical
necessity)
External review
(coordinated by Express Scripts)
800-841-5396
Prescription drug denials - not involving
medical judgment (such as for no eligibility
for coverage)
Plan administrator 888-276-4732

75
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Section 1.01
There usually will be no need for you to submit claims under the Plan because, as described below, your
provider will generally do so for you. When you do need to submit a claim, you must do so in accordance
with these Claims Procedures. This Article 1 discusses some general points regarding claims. The remaining
sections of these Claims Procedures provide the formal Claims Procedures that must be followed in order to
receive benets under the Plan.
The plan administrator reserves the right to decide whether to pay benets to you, to the provider of services,
or to you and the provider jointly.
Failure to follow the below-stated deadlines or to exhaust these Claims Procedures will result in the forfeit of
your right to sue the Plan in State or federal court.
Section 1.02
If you or a covered dependent is hospitalized, you must present your benet ID card to the facility
representative. In most cases, the hospital will bill the Plan directly for the cost of the hospital services, the
Plan will pay the hospital, and you will receive copies of the payment record. A hospital may require you, at
the time of discharge, to pay charges that might not be covered by the Plan. If this happens, you must pay
these amounts yourself. The Plan will reimburse you if any of the charges you pay are later determined to be
covered by the Plan.
You may be billed by the hospital directly. In order to claim your benets for these charges, send a copy of the
itemized bill to the physical address on your ID card, and be sure it includes the information listed in Section
3.03.
Outside of the United States the Plan will only reimburse for emergency care (unless you are stationed in an
included U.S. territory, in which case the Plan will also reimburse for non-emergency covered services rendered
in an included U.S. territory). For emergency care received outside of the United States, you should pay the
hospital, physician, or professional provider at the time services are rendered. In order to claim your benets for
these charges, send a copy of the itemized bill to the physical address on your ID card, and be sure it includes
the information listed in Section 3.03. (If you are stationed in an included U.S. territory and receiving care from
hospital, physician, or professional provider that contracts directly with the Plan to provide covered services,
then you should present your benet ID card and, in most cases, the hospital, physician, or professional
provider will bill the Plan directly.)
Section 1.03
In most cases, your in-network provider will bill charges directly to the Plan via the third party administrator.
You are required to pay any applicable co-payments at the time of service.
If you or your covered dependents see an out-of-network provider for other than emergency or urgent care
you will be responsible for any charges. All out-of-network services must be pre-certied by the
utilization review manager except in the case of an , in which case the must be notied
within 24 hours of the admission/treatment or on the next business day and the patient must consent to
a transfer to an as soon as the patient is stable.
If the treatment is for an accidental injury, include a statement explaining the date, time, place and
circumstances of the accident when you send us the bill.
Section 1.04

76
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Certain prescription drugs require pre-certication. The pre-certication process for prescription drug benets
is administered by ESI. Your doctor or doctor’s oce will need to call ESI to perform a clinical review. To begin
the pre-certication process, your doctor should call 800-841-5396. Pre-certication can be provided over
the phone 24 hours a day, seven days a week. If your request is approved, your prescription may be lled at
any participating pharmacy. Please call ESI at 800-841-5396 or visit www.express-scripts.com to determine
coverage of your medication or if you have any questions.
You should use your ID card at point of service to obtain medications. If you need to submit a manual claim
for prescription drug benets, you should call ESI to receive a claim form. You should complete the claim
form fully and submit a separate claim form for each separate pharmacy used and for each separate enrollee
who received prescription medications. The claim form must include receipts that contain the following
information: (1) date prescription lled, (2) name and address of pharmacy, (3) prescription drug name,
strength and National Drug Code, (4) prescription number, (5) quantity and days’ supply, (6) price, and (7) the
name of the enrollee receiving the medication. Send the claim form, including receipts, to ESI at the address
instructed on the form.
If you have been an enrollee in the Plan for more than 90 days, in order to receive full prescription drug
benets, you must use your ID card at the point of service to obtain medications.
For prescription drug claims, ESI is the claims reviewer and will handle all claims for prescription drug benets
and is responsible for deciding appeals of any adverse benet determinations pertaining to prescription
drug benets. However, the plan administrator has the nal authority in deciding whether an internal claim
or appeal will be approved or denied. External review of claims for prescription drug benets that involve
medical judgment will be performed by the independent review organizations with which ESI has contracted.
The provisions of this Section 1.04 supersede any inconsistent Plan provisions.
Section 1.05
Bills for ambulance service must show where the patient was picked up and where the patient was taken.
This is in addition to the information required under Section 3.03.
Section 1.06
If you have any questions about how to le a claim, the status of a pending claim, or any action taken on a
claim, call WebTPA at 888-276-4732.
Section 1.07
A claimant may appoint an authorized representative in writing to act on his or her behalf with respect to
claims and appeals under these Claims Procedures. Additionally, the Plan shall, even in the absence of a
signed Appointment of Authorized Representative form, recognize a physician or professional provider with
knowledge of the claimant’s medical condition (e.g., the treating physician) or the facility where the claimant
is/was treated as the claimant’s authorized representative unless the claimant provides specic written
direction otherwise, and an employee is automatically deemed to be the authorized representative of his or her
covered dependent who is under age 18. An Appointment of Authorized Representative form may be obtained
from WebTPA by calling 888-276-4732. Completed forms must be submitted to the utilization review manager,
WebTPA, or Express Scripts (depending on the proper recipient of the claim or appeal). An attempted
assignment for purposes of payment does not constitute appointment of an authorized representative under
the Claims Procedures. Once an authorized representative is appointed, recognized, or deemed, the Plan
shall direct all information, notication, etc. regarding the claim to the authorized representative. The claimant
shall be copied on all notications regarding decisions, unless the claimant provides specic written direction
otherwise. Any reference in the Claims Procedures to “claimant” is intended to include the authorized
representative of such claimant appointed in compliance with the above procedures.

77
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Article 2 FOUR TYPES OF CLAIMS
Section 2.01
Whether you le them directly or your provider does so for you, there are, as described below, four categories
of claims that can be made under the Plan, each with somewhat dierent claim and appeal rules. The federal
regulations set dierent requirements based on the type of claim involved. The primary dierence is the
timeframe within which claims and appeals must be determined.
Section 2.02
A claim is a “pre-certication claim” (sometimes known as a pre-service claim) if (1) it is submitted before the
underlying benet is received and (2) the Plan specically conditions receipt of the underlying benet, in
whole or in part, on receiving approval in advance of obtaining the relevant medical care.
Under the Plan, you or your provider must obtain pre-certication of medical necessity for all medical care
(including prescription drug benets) that (1) is not routine care provided by your physician and (2) does not
involve an emergency medical condition.
To receive medical necessity pre-certication you must contact Customer Service at 888-276-4732 before you
receive the medical care. For prescription drug pre-certication, call Express Scripts at 800-841-5396. For
dental pre-certication, call WebTPA via Customer Service at 888-276-4732.
Such pre-certication does not guarantee that the Plan covers the requested services. Plan coverage
decisions are made at the post-service claim level.
Section 2.03
An “urgent pre-certication claim” is a special type of pre-certication claim that involves urgent care. A
pre-certication claim involves urgent care if application of the time periods that otherwise apply to pre-
certication claims (1) could seriously jeopardize the claimant’s life or health or ability to regain maximum
function or (2) would—in the opinion of a physician with knowledge of the claimant’s medical condition—
subject the claimant to severe pain that cannot be adequately managed without the care or treatment that is
the subject of the claim.
On receipt of a pre-certication claim, the Plan will make a determination of whether it involves urgent care,
provided that, if a physician with knowledge of the claimant’s medical condition determines that a claim
involves urgent care, the claim shall be treated as an urgent pre-certication claim.
Throughout these Claims Procedures, when the terms “pre-certication” and “pre-certication claim” are used
without the term “urgent,” they are used to describe non-urgent pre-certication claims.
Section 2.04
A “post-service claim” is any claim that (1) is submitted after the relevant medical care has been received and
(2) is in regard to a determination that the Plan does not require be made in advance of the receipt of medical
care (such as plan coverage determinations or medical necessity determinations for emergency medical
conditions).
Under the Plan, post-service claims are required to determine whether the Plan covers medical care you
receive. Generally, your provider will le post-service claims. If your provider does not le a post-service claim
on your behalf, you should le such claims in accordance with Section 3.03.
Section 2.05
A “concurrent care claim” is a claim that involves a request for an extension of an already approved and

78
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
ongoing course of treatment that is being provided over a period of time or for a specied number of
treatments.
Section 2.06 C
The claim type is determined initially when the claim is led. However, if the nature of the claim changes
as it proceeds through these Claims Procedures, the claim may be re-characterized. For example, a claim
may initially be an urgent pre-certication claim. If the urgency subsides, it may be re-characterized as a pre-
certication claim.
Section 2.07
It is very important to follow the requirements that apply to your particular type of claim. If you have any
questions regarding what type of claim and/or what claims procedure to follow, contact Customer Service at
888-276-4732.
Article 3 HOW TO FILE A CLAIM FOR BENEFITS
Section 3.01
Claims for all medical services must be submitted in accordance with these procedures. See Section 1.04 for
instructions on ling a claim for prescription drug benets. You should keep copies of all of your submitted
claims.
Section 3.02
To le a pre-certication claim or an urgent pre-certication claim (usually to obtain pre-certication of medical
necessity), you or your authorized representative must contact Customer Service at 888-276-4732 before you
receive the medical care.
If you fail to obtain required pre-certication of medical necessity, you may request a retroactive certication
of medical necessity from the utilization review manager. In order to receive retroactive certication of medical
necessity, you must demonstrate reasonable cause (i.e., emergency medical condition) for your failure to
receive pre-certication. If the utilization review manager determines you had reasonable cause for your
failure to receive pre-certication, it will review your claim using the Plan’s usual medical necessity criteria.
The decision to provide retroactive certication of medical necessity will be made in the sole discretion of the
utilization review manager.
Section 3.03
A post-service claim must be led by you or your authorized representative within one year following the date
of service of the medical service, treatment or product to which the claim relates.
For benets received at a PPO facility or through a PPO provider, your provider will, generally, le required
post-service claims. For out-of-network services, your provider may not le post-service claims on your
behalf. All services must be by the except
in the case of an , in which case the must be notied within 24 hours of the admission/
treatment or on the next business day and the patient must consent to a transfer to an
as soon as the patient is stable.
If you receive services for which your provider does not le a post-service claim on your behalf, you should
submit a post-service claim to WebTPA at the address on the second page of this SPD. The appropriate claim
forms may be obtained by contacting Customer Service at 888-276-4732.
The following general steps should be followed in order to le a post-service claim for which your provider did
not le a claim on your behalf:

79
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
(i) Complete the employee portion of the claim form in full. Answer all questions, even if the answer is
“none” or “N/A” (not applicable).
(ii) Attach all necessary documentation of expenses to the claim form. Documentation must include:
• The employee’s name and member ID number;
• The name of the covered person who was treated;
• The date(s) of service, treatment, or purchase;
• The provider’s name, address, phone number and degree;
• The federal tax identication number of the provider;
• The diagnosis;
• The CPT codes related to the services or supplies provided;
• A description of services or supplies provided, detailing the charge for each supply or service (non-
itemized bills are not acceptable).
(iii) Complete a separate claim form for each person for whom benets are being requested.
(iv) If another plan is the primary payer, a copy of the other plan’s Explanation of Benets (EOB) must
accompany the claim form sent to the Plan.
Post-service claims should be submitted in writing to WebTPA at the address on the second page of this SPD.
Section 3.04
These Claims Procedures do not apply to any request for benets that is not made in accordance with these
Claims Procedures, except that (a) in the case of an incorrectly led pre-certication claim, the claimant shall
be notied as soon as possible but no later than 5 days following receipt by the Plan of the incorrectly led
claim; and (b) in the case of an incorrectly led urgent pre-certication claim, the claimant shall be notied as
soon as possible but no later than 24 hours following receipt by the Plan of the incorrectly led claim. The
notice shall explain that the request is not a claim and describe the proper procedures for ling a claim. The
notice may be oral unless written notice is specically requested by the claimant.
Section 3.05
Once a claim has been led, these Claims Procedures will not apply to any substantially identical request
for benets unless the passage of time, change in condition of the enrollee, or change of accepted medical
practice might result in a dierent determination. Whether to accept a substantially identical request for
benets as a new claim is in the sole discretion of the plan administrator. Most such requests will not be
processed as new claims. Rather, in the event of an adverse benet determination, the appeal process
described below will be the only method for pursuit of a dierent determination and the determination will be
nal upon completion of the external review described in Article 12.
Article 4 TIMEFRAME FOR DECIDING INITIAL BENEFIT CLAIMS
Section 4.01
The Plan shall decide an initial pre-certication claim within a reasonable time appropriate to the medical
circumstances, but no later than 15 days after receipt of the claim.
Section 4.02

80
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
The Plan shall decide an initial urgent pre-certication claim as soon as possible, taking into account the
medical exigencies, but no later than 72 hours after receipt of the claim.
Section 4.03
If a claim is a request to extend a concurrent care claim involving urgent care and if the claim is made at least
24 hours prior to the end of the initially approved period of time or number of treatments, the claim shall
be decided within no more than 24 hours after receipt of the claim. Any other concurrent care claim shall be
decided in the otherwise applicable timeframes for pre-certication claims.
Section 4.04
A decision by the Plan to reduce or terminate a previously approved course of treatment is an adverse benet
determination that may be appealed by the claimant under these Claims Procedures, as explained below.
Notication to the claimant of a decision by the Plan to reduce or terminate an initially approved course of
treatment shall be provided suciently in advance of the reduction or termination to allow the claimant to
appeal the adverse decision and receive a decision on review under these procedures prior to the reduction
or termination.
Section 4.05
The Plan shall decide an initial post-service claim within a reasonable time but no later than 30 days after
receipt of the claim.
Section 4.06
If the Plan is not able to decide a pre-certication or post-service claim within the above timeframes, due to
matters beyond its control, one 15-day extension of the applicable timeframe is permitted, provided that
the claimant is notied in writing prior to the expiration of the initial timeframe applicable to the claim. The
extension notice shall include a description of the matters beyond the Plan’s control that justify the extension
and the date by which a decision is expected. No extension is permitted for urgent pre-certication claims.
Despite the specied timeframes, nothing prevents the claimant from voluntarily agreeing to extend the
above timeframes.
Section 4.07
If any information needed to process a claim is missing, the claim shall be treated as an incomplete claim.
Section 4.08
If an urgent pre-certication claim is incomplete, the Plan shall notify the claimant as soon as possible, but
no later than 24 hours following receipt of the incomplete claim. The notication may be made orally to the
claimant, unless the claimant requests written notice, and it shall describe the information necessary to
complete the claim and shall specify a reasonable time, no less than 48 hours, within which the claim must
be completed. The Plan shall decide the claim as soon as possible but not later than 48 hours after the earlier
of (a) receipt of the specied information, or (b) the end of the period of time provided to submit the specied
information.
Section 4.09
If a pre-certication claim or post-service claim is incomplete, the Plan may deny the claim or may take an
extension of time, as described above. If the Plan takes an extension of time, the extension notice shall
include a description of the missing information and shall specify a timeframe, no less than 45 days, in which
the necessary information must be provided. The timeframe for deciding the claim shall be suspended from
the date the extension notice is received by the claimant until the date the missing necessary information
is provided to the Plan. If the requested information is provided, the Plan shall decide the claim within the
extended period specied in the extension notice. If the requested information is not provided within the time

81
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
specied, the claim will be decided without that information.
Article 5 NOTIFICATION OF INITIAL BENEFIT DECISION BY PLAN
Section 5.01
Written notication of the Plan’s decision on a pre-certication claim or urgent pre-certication claim shall be
provided to the claimant whether or not the decision is an adverse benet determination.
Section 5.02
Written notication shall be provided to the claimant of the Plan’s adverse benet determination on a claim and
shall include the following, in a manner calculated to be understood by the claimant:
• information sucient to identify the claim involved, including, if applicable: (i) the date of service,
(ii) the health care provider, (iii) the claim amount, and (iv) a statement describing the availability,
upon request, of the diagnosis code and its corresponding meaning, and the treatment code and its
corresponding meaning;
• a statement of the specic reason(s) for the decision, including (i) the Plan’s denial code and its
corresponding meaning (ii) the Plan’s standard, if any, that was used in denying the appeal; and (iii), for
nal internal adverse benet determinations, a discussion of the decision;
• a reference to the specic Plan provision(s) on which the decision is based;
• a description of any additional material or information necessary for the claimant to perfect the claim/
appeal and an explanation of why such material or information is necessary;
• a description of the Plan’s review procedures and the time limits applicable to such procedures;
• a statement disclosing any internal rule, guidelines, protocol or similar criterion relied on in making the
adverse decision (or a statement that such information will be provided free of charge upon request);
• for adverse benet determinations (including nal internal adverse benet determinations) of appeals, a
statement indicating entitlement to receive on request, and without charge, reasonable access to or
copies of all documents, records or other information relevant to the determination;
• if the decision is based on a medical necessity or experimental treatment or similar exclusion or limit,
disclose either (a) an explanation of the scientic or clinical judgment applying the terms of the Plan
to the claimant’s medical circumstances, or (b) a statement that such explanation will be provided at
no charge on request.
• in the case of an urgent pre-certication claim, an explanation of the expedited review methods
available for such claims/appeals;
• a statement describing any remaining mandatory appeal and information regarding how to initiate any
such remaining appeal;
• a statement of the right to sue in State court; and
• the availability of and contact information for any applicable oce of health insurance consumer
assistance or ombudsman established under PHS Act § 2793 to assist individuals with the internal
claims and appeals and external review processes.
Notication of the Plan’s adverse benet determination on an urgent pre-certication claim may be provided
orally, but written notication shall be furnished no later than three days after the oral notice.

82
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Article 6 HOW TO APPEAL AN ADVERSE BENEFIT DETERMINATION
For a summary of these rules, please see the chart at the beginning of the Claims Procedures chapter.
The chart is oered for your convenience and ease of use: You must refer to the full language in the
numbered sections below for details regarding the appeal process and how to calculate your deadlines.
Section 6.01
A claimant, or the claimant’s authorized representative, has a right to appeal an adverse benet determination
under these Claims Procedures.
Section 6.02
In light of the expedited timeframes for decision of urgent pre-certication claims, an urgent pre-certication
appeal may be submitted to the utilization review manager by phone at 888-276-4732. All necessary
information in connection with an urgent pre-certication appeal shall be transmitted between the Plan and
the claimant by telephone, fax, or e-mail.
Section 6.03
An appeal of an adverse benet determination involving a pre-certication claim should be submitted to
the utilization review manager. Details on how to submit an appeal to the utilization review manager will be
provided by the utilization review manager upon an adverse benet determination. You may call the utilization
review manager at 888-276-4732 for more information.
Section 6.04
A post-service appeal of an adverse benet determination requiring a determination involving medical
judgment should be submitted to the utilization review manager. Details on how to submit an appeal to
the utilization review manager will be provided by the utilization review manager upon an adverse benet
determination. You may call Customer Service at 888-276-4732 for more information. Except in the case of
an appeal relating to prescription drug benets, a post-service appeal of an adverse benet determination
that does not require a determination involving medical judgment is led by submitting a written Request
for Review form to WebTPA. A claimant has the right to submit documents, written comments, or other
information in support of an appeal. Request for Review forms may be obtained by contacting the utilization
review manager or WebTPA via Customer Service at 888-276-4732.
If you are unsure whether the adverse benet determination involved medical judgment, you should contact
the utilization review manager at (888) 276-4732.
Section 6.05
To appeal a denied prescription drug benet claim, follow the instructions on the adverse benet
determination you received from ESI. (See Section 1.04 for more information and for contact information for
ESI.)
Section 6.06
The appeal of an adverse benet determination must be led within 180 days following the claimant’s receipt
of the notication of adverse benet determination, except that the appeal of a decision by the Plan to reduce
or terminate an initially approved course of treatment (see the denition of concurrent care decision) must be
led within 30 days of the claimant’s receipt of the notication of the Plan’s decision to reduce or terminate.
Failure to comply with this important deadline will cause the claimant to forfeit any right to any further review
of an adverse decision under these procedures or in a court of law.

83
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Article 7 HOW YOUR APPEAL WILL BE DECIDED
The following procedures will be followed for all appeal decisions:
Section 7.01
The review will take into account all information submitted by the claimant, whether or not presented or
available at the initial benet decision. Additionally, the claimant will be entitled to present evidence and
testimony pertaining to the claim.
No deference will be given to the initial benet decision, and the person who reviews and decides an appeal
will not be the same person who made the initial benet decision or such person’s subordinate.
Section 7.02
In the case of a claim denied on the grounds of a medical judgment, the reviewer will consult with a health
care professional with appropriate training and experience. The health care professional who is consulted on
appeal will not be the same health care professional who was consulted, if any, regarding the initial benet
decision or a subordinate of that individual.
Section 7.03
A claimant shall have a right to review his or her claim le and, on request and free of charge, be given
reasonable access to, and copies of, all documents, records, and other information relevant to the claimant’s
claim for benets. If the advice of a medical or vocational expert was obtained in connection with the initial
benet decision, the names of each such expert shall be provided on request by the claimant, regardless of
whether the advice was relied on by the Plan.
Section 7.04
The Plan will provide the claimant, free of charge, with any new or additional evidence considered, relied
upon, or generated by the Plan in connection with the claim. Also, before the Plan issues a nal internal
adverse benet determination that is based on a new or additional rationale, the Plan will provide the
claimant, free of charge, with the rationale. Both any new evidence and any new rationale will be provided
to the claimant suciently in advance of the Plan’s nal benet or appeal decision to allow the claimant a
reasonable opportunity to respond to the new evidence and/or rationale.
Article 8 TIMEFRAMES FOR DECIDING BENEFITS APPEALS
Section 8.01
The appeal of an adverse benet determination relating to a pre-certication claim shall be decided within a
reasonable time appropriate to the medical circumstances but no later than thirty (30) days after receipt of the
appeal.
Section 8.02
The appeal of an adverse benet determination relating to an urgent pre-certication claim will be decided as
soon as possible, taking into account the medical exigencies, but no later than seventy-two (72) hours after
receipt of the appeal.
Section 8.03
The appeal of an adverse benet determination relating to a post-service claim shall be decided within a
reasonable period but no later than sixty (60) days after receipt of the appeal.
Section 8.04

84
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
The appeal of a decision by the Plan to reduce or terminate an initially approved course of treatment shall
be decided before the proposed reduction or termination takes place. The appeal of a denied request to
extend any concurrent care shall be decided in the appeal timeframe for pre-certication claims or urgent pre-
certication claims described above, as appropriate to the request.
Article 9 NOTIFICATION OF DECISION ON APPEAL
Written notication of the decision on appeal shall be provided to the claimant whether or not the decision
is an adverse benet determination. If the decision is an adverse benet determination, the written notication
shall include the information in Section 5.02, written in a manner calculated to be understood by the claimant.
Notication of an adverse benet determination on appeal of an urgent pre-certication claim may be provided
orally, but written notication shall be furnished not later than three days after the oral notice.
Article 10 REVIEW OF APPEAL DECISION THAT DOES NOT INVOLVE MEDICAL JUDGMENT
– SECOND APPEAL
Section 10.01
If your appeal did not involve a medical judgment (for example, the appeal involved Plan eligibility), then you
may request a review of the appeal decision by contacting the plan administrator at:
Adventist Risk Management
12501 Old Columbia Pike
Silver Spring, MD 20904
888-276-4732
benets@adventistrisk.org
The plan administrator will assign an appointee to review your second appeal. The appointee will follow the
procedure described in Article 7 when reviewing your second appeal, and you have the rights described in
that article.
The review will take into account all information submitted by the claimant, whether or not presented or
available at the initial benet decision. Additionally, the claimant will be entitled to present evidence and
testimony pertaining to the claim.
No deference will be given to the initial benet decision or the rst appeal, and the person who reviews and
decides the second appeal will not be the same person who made the initial benet decision, the person who
decided the rst appeal, or either person’s subordinate.
Section 10.02
You must submit your request for a second appeal within four months after the date of receipt of the notice
of adverse benet determination from your rst appeal (for example, if the notice is received on March 15, then
the request must be led by July 15). If there is no corresponding date, then the deadline is the rst day of the
fth month following receipt of the notice (for example, if the notice is received on October 30, since there
is no February 30, the request must be led by March 1). If the ling date would fall on a Saturday, Sunday,
or Federal holiday, the last ling date is extended to the next day that is not a Saturday, Sunday, or Federal
holiday.
Section 10.03
The appointee of the plan administrator will provide written notice of the Plan’s decision within 45 days of its
receipt of your request for second appeal, unless the second appeal involves (1) a medical condition where
this timeframe would seriously jeopardize the life or health of the claimant or would jeopardize the claimant’s
ability to regain maximum function, or (2) an admission, availability of care, continued stay, or health care item
of service for which the claimant received emergency services, but has not been discharged, in which case

85
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
the appointee will provide notice within 72 hours (and then, if the notice is not in writing, will provide written
conrmation within 48 hours of the initial verbal notice).
If the decision is an adverse benet determination, the written notication shall include the information in
Section 5.02, written in a manner calculated to be understood by the claimant.
Section 10.04
The Plan will not consider you to have exhausted the administrative remedies available under the Plan until
you have properly led and received a decision on your second appeal, as described in Article 10 of this
Claims Procedure.
If you fail to follow these Claims Procedures, if you miss any of the above-stated deadlines for ling a claim or
an appeal, or if you otherwise fail to exhaust all of the administrative remedies under the Plan, then you will
forfeit any right to pursue any remedies under State or federal law.
Section 10.05
If the appointee of the plan administrator who reviews the second appeal reverses the rst appeal’s adverse
benet determination, the Plan will immediately provide coverage or payment (including immediately
authorizing or immediately paying benets) for the claim.
Article 11 EXHAUSTION AND DEEMED EXHAUSTION OF INTERNAL CLAIMS AND APPEALS
PROCESSES
If you fail to follow these Claims Procedures, if you miss any of the above-stated deadlines for ling a claim or
an appeal, or if you otherwise fail to exhaust all of the administrative remedies under the Plan, then (i) you will
not be eligible for external review unless the completion of an urgent pre-certication appeal would seriously
jeopardize the life or health of the claimant or would jeopardize the claimant’s ability to regain maximum
function, and (ii) you will forfeit any right to pursue any remedies under State or federal law. This means that if
you do not comply with the deadlines and fully exhaust these Claims Procedures, you may not sue the Plan.
If the Plan fails to strictly adhere to these Claims Procedures when reviewing your claim or appeal, you will be
deemed to have exhausted the Plan’s internal claims and appeals process, unless the violation is de minimis,
non-prejudicial, is attributable to good cause or matters beyond the Plan’s control, occurred in the context of
an ongoing, good faith exchange of information between you and the Plan, and is not reective of a pattern
or practice of non-compliance. If the Plan claims that a violation occurred that meets the above exception,
you may request a written explanation of the violation; the Plan will reply within 10 days to such a request and
will include a description of the reasons for asserting that the violation did not cause the Claims Procedures
to be deemed exhausted. If you have been deemed to have exhausted the Plan’s internal claims and appeals
process, you may (i) initiate an external review, or (ii) pursue any remedies available under State law on the
basis that the Plan has failed to provide a reasonable internal claims and appeals process that would yield a
decision on the merits of the claim.
Article 12 EXTERNAL REVIEW (FOR REVIEW OF AN APPEAL DECISION INVOLVING MEDICAL
JUDGMENT)
Section 12.01
As required by the Patient Protection and Aordable Care Act, the Plan complies with the federal external
review process. This means that you are eligible to have certain adverse benet determinations reviewed by an
independent review organization and the decision reached through the external review is binding on the Plan.
The Plan will pay the cost of external reviews.
Section 12.02 E
To be eligible for external review, all nal internal adverse benet determinations must meet requirement (i)

86
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
below and all other adverse benet determinations must meet both requirements (i) and (ii).
Requirements:
(i) The adverse benet determination (including nal internal adverse benet determinations) must involve
medical judgment (including, but not limited to, those based on the Plan’s requirements for medical
necessity, appropriateness, health care setting, level of care, or eectiveness of a covered benet; or
the Plan’s determination that a treatment is experimental or investigational), as determined by the
external reviewer.
(ii) Adverse benet determinations that involve a medical condition of the claimant for which the timeframe
for completion of an urgent pre-certication appeal would seriously jeopardize the life or health of the
claimant or would jeopardize the claimant’s ability to regain maximum function.
The Plan will notify you in writing when you are eligible to le a request for an external review and will provide
you with the necessary information for ling such a request.
Section 12.03
A claimant who is eligible for an external review must le a request for an external review with the Plan within
four months after the date of receipt of a notice of adverse benet determination or nal internal adverse benet
determination (for example, if the notice is received on March 15, then the request must be led by July 15).
If there is no corresponding date, then the deadline is the rst day of the fth month following receipt of the
notice (for example, if the notice is received on October 30, since there is no February 30, the request must
be led by March 1). If the ling date would fall on a Saturday, Sunday, or Federal holiday, the last ling date is
extended to the nest day that is not a Saturday, Sunday, or Federal holiday.
Section 12.04
Within ve business days following the date of receipt of the external review request, the Plan will complete a
preliminary review of the request to determine whether:
(i) The claimant is or was covered under the Plan at the time the health care item or service was
requested or, in the case of a retrospective review, was covered under the Plan at the time the health
care item or service was provided;
(ii) The adverse benet determination or the nal internal adverse benet determination does not relate to
the claimant’s failure to meet the requirements for eligibility under the terms of the Plan (for example,
worker classication or similar determination);
(iii) The claimant has exhausted the Plan’s internal appeal process or if the claimant is deemed to have
exhausted the internal appeals process under Article 11; and
(iv) The claimant has provided all the information and forms required to process an external review.
Within one business day after completion of the preliminary review, the Plan will issue a notication in writing
to the claimant. If the Plan determines the claim is not eligible for external review, the Plan will notify the
claimant and will include in the notication the reasons for the claim’s ineligibility and contact information
for the Employee Benets Security Administration. If the Plan determines the request is not complete, the
notication will describe the information or materials needed to make the request complete and the Plan will
allow the claimant to perfect the request for external review within the ling period described above or within
the 48 hour period following the receipt of the notication, whichever is later.
If the Plan determines the claim request is complete and is eligible for external review, it will forward the
claim to an independent review organization. The Plan will contract (directly or indirectly) with at least three
independent review organizations and will rotate claims assignments among the contracted independent
review organizations. None of the contracted independent review organizations will be eligible for any nancial

87
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
incentives based on the likelihood that they will support the denial of benets.
Section 12.05
A claimant may request an expedited external review if the claimant receives:
(i) An adverse benet determination that involves a medical condition of the claimant for which the
timeframe for completion of an urgent pre-certication appeal would seriously jeopardize the life or
health of the claimant or would jeopardize the claimant’s ability to regain maximum function.
(ii) A nal internal adverse benet determination, (a) if the claimant has a medical condition where the
timeframe for completion of a standard external review would seriously jeopardize the life or health
of the claimant or would jeopardize the claimant’s ability to regain maximum function or (b) if the
nal internal adverse benet determination concerns an admission, availability of care, continued stay,
or health care item of service for which the claimant received emergency services, but has not been
discharged from a facility.
Immediately upon receipt of the request for expedited external review, the Plan will determine whether the
request meets the reviewability requirements set forth in Section 12.04 above for standard external review.
The Plan will immediately send the notice required under Section 12.04 above for standard external review to
the claimant of its eligibility determination.
Section 12.06
Upon a determination that a request is eligible for external review following the preliminary review, the Plan
will assign an independent review organization pursuant to Section 12.04 above for standard review. The Plan
will provide all necessary documents and information considered in making the adverse benet determination
or nal internal adverse benet determination to the assigned independent review organization electronically or
by telephone or facsimile or any other available expeditious method.
The assigned independent review organization, to the extent the information or documents are available and
the independent review organization considers them appropriate, will consider the information or documents
described above under the procedures for standard review. In reaching a decision, the assigned independent
review organization will review the claim de novo and is not bound by any decisions or conclusions reached
during the Plan’s internal claims and appeals process.
Section 12.07
The assigned independent review organization will provide written notice of the nal external review decision
to the Plan and the claimant within 45 days of the independent review organization’s receipt of the request
for external review. In the case of expedited external review, the independent review organization will
provide notice of the nal external review decision as expeditiously as the claimant’s medical condition or
circumstances require, but in no event more than 72 hours after the independent review organization receives
the request for an expedited external review; if the initial notice is not in writing, the independent review
organization will provide written conrmation of the decision to the claimant and Plan within 48 hours of
providing the initial notice.
The notication of a nal external review decision will contain all information required by Department of Labor
guidance, including the following:
(i) A general description of the reason for the request for external review, including information sucient
to identify the claim (including the date or dates of service, the health care provider, the claim
amount (if applicable), the diagnosis code and its corresponding meaning, the treatment code and its
corresponding meaning, and the reason for the previous denial);
(ii) The date the independent review organization received the assignment to conduct the external review
and the date of the independent review organization decision;

88
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
(iii) References to the evidence or documentation, including the specic coverage provisions and
evidence-based standards, considered in reaching its decision;
(iv) A discussion of the principal reason or reasons for its decision, including the rationale for its decision
and any evidence-based standards that were relied on in making its decision;
(v) A statement that the determination is binding except to the extent that other remedies may be
available under State or Federal law to either the Plan or to the claimant;
(vi) A statement that judicial review may be available to the claimant; and
(vii) Current contact information, including phone number, for any applicable oce of health insurance
consumer assistance or ombudsman established under Public Health Service Act Section 2793.
Section 12.08
Upon receipt of a nal external review decision reversing the adverse benet determination, the Plan will
immediately provide coverage or payment (including immediately authorizing or immediately paying benets)
for the claim.
Article 13 AVOIDING CONFLICTS OF INTEREST
The Plan will ensure that all claims and appeals are adjudicated in a manner designed to ensure the
independence and impartiality of the persons involved in making the decision. Accordingly, decisions
regarding hiring, compensation, termination, promotion, or other similar matters with respect to any individual
(such as a claims adjudicator or medical expert) will not be made based upon the likelihood that the individual
will support the denial of Plan benets.
If you have questions about these Claims Procedures, contact the plan administrator.

89
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Benets Available from Other Sources
Situations may arise in which your healthcare expenses may be the responsibility of someone other than this
Plan. Here are descriptions of the situations that may arise.
A. Coordination of Benets (COB)
This provision applies to this Plan when you or your covered dependent has healthcare coverage under more
than one plan. For a complete explanation of COB see the chapter titled Coordination of Benets.
B. Third-Party Liability
An individual covered by us may have a legal right to recover benets or healthcare costs from another
person, organization or entity, or an insurer as a result of an illness or injury for which benets or healthcare
costs were paid by us. For example, an individual who is injured may be able to recover the benets or
healthcare costs from an individual or entity responsible for the injury or from an insurer, including dierent
forms of liability insurance, uninsured motorist coverage or under-insured motorist coverage. As another
example, an individual may become sick or be injured in the course of employment, in which case the
employer or a workers’ compensation insurer may be responsible for healthcare expenses connected with
the illness or injury.
If a covered individual, as dened below, has a right to recover benets or healthcare costs from a third party,
we will pay the covered individuals’ expenses subject to an automatic lien in the Plan’s favor to the extent
of benets paid, upon any compensation received from the other party, up to the sum of the amount paid
by the Plan to perfect the lien and the amount paid by the Plan for your benets. The total lien amount will
not exceed the maximum amount allowable under state law. If you are found by a judge, jury or arbitrator
to be partially at fault then the lien shall be reduced by the same comparative fault percentage by which
your recovery was reduced. The lien amount is also subject to pro rata reduction, commensurate with your
reasonable attorney’s fees and costs, in accordance with common fund doctrine. The above-described
limitations on the total amount of the lien do not apply to liens made against workers’ compensation claims,
liens for Medicaid benets, or liens for hospital services and hospital-aliated health facility services.
If benets have been paid, or payment of benets is pending, we are entitled to recover the amount paid or
the amount pending payment from the proceeds of any recovery made by a covered individual against a third
party.
This Section applies to any covered individual for whom payment of benets is made by us whether or not the
event giving rise to the covered individual’s injuries occurred before the individual became covered by us.
Denitions
For purposes of this Section relating to third party recoveries, the following denitions apply:
• Covered Individual means an individual covered by us, including a dependent of a member. “Covered
individual” also includes the estate, heirs, guardian or conservator of the individual for whom benets
have been paid or may be paid by us, and includes any trust established for the purpose of receiving
“Recovery Funds” and paying for the future income, care or medical expenses of such individual.
• Benets means any amount paid by us, or submitted to us for payment to or on behalf of the covered
individual. Bills, statements or invoices submitted to us by a provider of services, supplies or facilities
to or on behalf of a covered individual are considered requests for payment of “benets” by the
covered individual.
• Third Party Claim means any claim, settlement, award, lawsuit, verdict, judgment, arbitration decision
or other action against a third party (or any right to assert the foregoing) by or on behalf of a covered
individual, regardless of the characterization of the claims or damages of the covered individual,

90
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
and regardless of the characterization of the recovery funds. (For example, a covered individual
who has received payment of medical expenses from us, may le a third party claim against the
party responsible for the covered individual’s injuries, but only seek the recovery of non-economic
damages. In that case, we are still entitled to recover benets as described herein.)
• Third Party means any individual or entity responsible for the injury or illness, or the aggravation of an
injury or illness, of the covered individual. Third party includes any insurer of such individual or entity,
including dierent forms of liability insurance, or any other form of insurance that may pay money to
or on behalf of the covered individual including uninsured motorist coverage, under-insured motorist
coverage, and workers’ compensation insurance.
• Recovery Funds means any amount recovered from a third party.
Under this Section relating to third party recoveries, if we have paid any benets, we will be entitled
to recover the amount we have paid from the proceeds of any recovery made by a covered individual
against a third party. Upon claiming benets, or accepting payment of benets, or claiming or accepting
the provision of benets from us, the covered individual agrees to do whatever is necessary to fully secure
and protect, and to do nothing to prejudice, our right of reimbursement or subrogation as discussed in
this Section. In connection with our rights to obtain reimbursement or exercise our rights as described
below, the covered individual shall do one or more of the following things and agrees that we may do one
or more of the following things, at our discretion:
i. If the covered individual seeks payment by us of any benets for which there may be a
third party claim, the covered individual shall notify us of the potential third party claim. The
covered individual has this responsibility even if the rst request for payment of benets is a
bill or invoice submitted to us by a provider to the covered individual.
ii. Upon request from us, the covered individual shall provide to us all information available to
the covered individual, or any representative, or attorney representing the covered individual,
relating to the potential third party claim. The covered individual and his or her representatives
shall have the obligation to notify us in advance of any claim (written or oral) and/or any
lawsuit made against a third party seeking recovery of any damages from the third party,
whether or not the covered individual is seeking recovery of benets paid by us from the third
party.
iii. In order to receive payment of benets pursuant to this Section, we require that any covered
individual seeking payment of benets by us, and if the covered individual is a minor or legally
incapable of contracting, then the covered person’s parent or guardian, must ll out, sign
and return to WebTPA a third party recovery Agreement that includes a questionnaire about
the accident and the potential third party recovery. This Agreement will include provisions
consistent with the provisions of this Section, including an agreement to repay us for any
benets that we have paid relating to the injuries for which the covered individual is seeking
recovery from a third party. If the covered individual has retained an attorney to represent the
covered individual with respect to a third party claim, then the attorney must sign the third
party recovery Agreement, acknowledging the obligations described in the Agreement.
iv. If the covered individual makes a demand upon a third party, enters into settlement
negotiations or commences litigation, the covered individual must not prejudice, in any way,
our recovery rights under this Section. If a suit is led by the covered individual, the covered
individual agrees that we may cause to be recorded a notice of payment of benets, and such
notice will constitute a lien on any judgment or settlement. We may provide notice to the third
party or its insurer. In the event of settlement, the covered individual must obtain our consent
prior to releasing any third party from liability for payment of any expenses covered, paid
or pending for payment by us. The covered individual will hold the rights of and to recovery
funds in trust for our benet, up to the amount of benets we have paid or which are pending
payment at the time of resolution of the third party claim.

91
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
v. For any benets provided, pending payment, or paid by the Plan, the covered individual shall
promptly reimburse the Plan from any recovery funds, the full value of any such benets.
vi. To secure our rights to reimbursement for any benets paid or provided, the covered
individual, by claiming or accepting payment or the provision of benets by us hereby grants
to us a rst priority lien against the proceeds of any third party claim and assigns to us any
benets the covered individual may have under any insurance coverage’s, such lien and
assignment to apply only to the extent of benets paid, provided, or pending for payment. This
subparagraph (vi) is subject to the limitation in the second paragraph of subsection B above.
vii. The covered individual shall cooperate with us to protect our recovery rights under this
Section, and in addition, but not by way of limitation, shall:
a. Sign and deliver such documents as we reasonably require to protect our rights.
b. Provide any information to us relevant to the application of the provisions of this Section,
including medical information (including doctors’ reports, chart notes, diagnostic
test results, etc.), settlement correspondence, copies of pleadings or demands, and
settlement agreements, releases or judgments.
c. Take such actions as we may reasonably request to assist us in enforcing our rights to be
reimbursed from third party recoveries.
viii. By accepting the payment of benets by us, the covered individual agrees that we have the
right to intervene in any lawsuit or arbitration led by or on behalf of a covered individual
seeking damages from a third party. If we choose to intervene in the third party claim, we shall
not be liable for any attorney fees or costs incurred by the covered individual in connection
with the third party claim, and we shall have no obligation to reimburse the covered individual
for such attorney’s fees or costs.
ix. The covered individual agrees that we may notify any third party, or third party’s
representatives or insurers of our recovery rights set forth herein.
x. Even without your written authorization, we may release to, or obtain from, any other insurer,
organization or person, any information we need to carry out reimbursement from third party
recoveries and the provisions of this Section.
xi. If it is reasonable to expect that the covered individual will incur future expenses for which
benets might be paid by us, the covered individual shall seek recovery of such future
expenses in any third party claim
xii. If the covered individual continues to receive medical treatment for an illness or injury
after obtaining a settlement or recovery from a third party, we will provide benets for the
continuing treatment of that illness or injury pursuant to the terms of this third party claims
Section and only to the extent that the covered individual can establish that any sums that
may have been recovered from the third party for the continuing medical treatment have
been exhausted for that purpose.
xiii. By accepting benets, paid to or on behalf of the covered individual, the covered individual
agrees with the provisions of this Section and instructs his/her legal representatives to
comply with the provisions of this Section.
xiv. If the covered individual or the covered individual’s representatives fail to do any of the
foregoing acts at our request, then we have the right to suspend payment of any benets
for or on behalf of the covered individual related to any sickness, illness, injury or medical
condition arising out of the event giving rise to, or the allegations in, the third party claim. In
exercising this right, we may notify medical providers seeking authorization or pre-certication

92
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
of payment of benets that all payments have been suspended, and may not be paid.
xv. We have the sole discretion to interpret and construe these reimbursement and subrogation
provisions.
xvi. Coordination of benets (where the covered individual has healthcare coverage under more
than one plan or health insurance policy) is not considered a third party claim.
xvii. If any term, provision, agreement or condition of this Section is held by a court of competent
jurisdiction to be invalid or unenforceable, the remainder of the provisions shall remain in full
force and eect and shall in no way be aected, impaired or invalidated.
C. Motor Vehicle Insurance
We will not pay benets for healthcare costs to the extent that a covered individual including a covered
dependent is covered by motor vehicle insurance. But we will advance payment of benets over the amount
covered by the motor vehicle insurance, subject to the Third-Party Liability Section above. If we have paid
benets rst, we are entitled to any reimbursement from the motor vehicle insurer, under the Third-Party
Liability Section above.
You must give us information about any medical insurance payments available to the covered individual or
the covered individual’s covered dependents.
Coverage for injuries sustained in an automobile accident in which you are (or your covered dependent is) the
driver of a vehicle involved in the accident is only provided if you (or your covered dependent) had automobile
insurance, at the time of the accident, that met (or exceeded) your state’s minimum automobile insurance
requirements.
Medicare
Medicare will pay primary, secondary, or last to the extent stated in federal law. When Medicare is to be the
primary payer, this Plan will base its payment upon benets that would have been paid by Medicare under
Parts A and B regardless of whether the person was enrolled under any of these parts. The Plan reserves
the right to coordinate benets with respect to Medicare Part D. The plan administrator will make this
determination based on the information available through CMS.

93
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Coordination of Benets
Coordination Of This Plan’s Benets With Other Benets
The Coordination of Benets (COB) provision applies when you or your dependents have health care
coverage under more than one Plan. Plan, for purposes of this COB section, is dened below.
The order of benet determination rules govern the order in which each Plan will pay a claim for benets. The
Plan that pays rst is called the Primary plan. The Primary plan must pay benets in accordance with its terms
without regard to the possibility that another Plan may cover some expenses. The Plan that pays after the
Primary plan is the Secondary plan. When this plan is the Secondary plan it will reduce the benets it pays so
that payments from all Plans do not exceed 100% of the total Allowable expense.
Denitions
A. A Plan, for purposes of this COB section, is any of the following that provides benets or services for
medical or dental care or treatment. If separate contracts are used to provide coordinated coverage
for members of a group, the separate contracts are considered parts of the same plan and there is no
COB among those separate contracts.
(1) Plan includes self-funded employee health plans, group and nongroup insurance contracts,
health maintenance organization (HMO) contracts, closed panel plans or other forms of group or
group-type coverage (whether insured or uninsured); medical care components of long-term care
contracts, such as skilled nursing care; medical benets under group or individual automobile
contracts; and Medicare or any other federal governmental plan, as permitted by law.
(2) Plan does not include: hospital indemnity coverage or other xed indemnity coverage; accident
only coverage; specied disease or specied accident coverage; limited benet health coverage,
as dened by state law; school accident type coverage; benets for nonmedical components
of long-term care policies; Medicare supplement policies; Medicaid policies; or coverage under
other federal governmental plans unless permitted by law.
Each arrangement for coverage under (1) or (2) is a separate Plan. If a Plan has two parts and COB rules apply
only to one of the two, each of the parts is treated as a separate Plan.
B. Plan means, in a COB provision, the part of the arrangement providing the health care benets to
which the COB provision applies and which may be reduced because of the benets of other plans.
Any other part of the arrangement providing health care benets is separate from this Plan. An
arrangement may apply one COB provision to certain benets, such as dental benets, coordinating
only with similar benets, and may apply another COB provision to coordinate other benets.
C. The order of benet determination rules determine whether this Plan is a Primary plan or Secondary
plan when you and/or your dependent has health care coverage under more than one Plan. When
this Plan is primary, it determines payment for its benets rst before those of any other Plan without
considering any other Plan’s benets. When this Plan is secondary, it determines its benets after
those of another Plan and will reduce the benets it pays so that all Plan benets do not exceed 100%
of the total Allowable expense.
D. Allowable expense is a health care expense, including deductibles, co-insurance and co-payments,
that is covered at least in part by any Plan covering the person. When a Plan provides benets in
the form of services, the reasonable cash value of each service will be considered an Allowable
expense and a benet paid. An expense that is not covered by any Plan covering the person is
not an Allowable expense. In addition, any expense that a provider by law or in accordance with a
contractual agreement is prohibited from charging a covered person is not an Allowable expense.
The following are examples of expenses that are not Allowable expenses:

94
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
(1) The dierence between the cost of a semi-private hospital room and a private hospital room
is not an Allowable expense, unless one of the Plans provides coverage for private hospital
room expenses.
(2) If a person is covered by 2 or more Plans that compute their benet payments on the basis of
usual and customary fees or relative value schedule reimbursement methodology or other
similar reimbursement methodology, any amount in excess of the highest reimbursement
amount for a specic benet is not an Allowable expense.
(3) If a person is covered by 2 or more Plans that provide benets or services on the basis of
negotiated fees, an amount in excess of the highest of the negotiated fees is not an Allowable
expense.
(4) If a person is covered by one Plan that calculates its benets or services on the basis of usual
and customary fees or relative value schedule reimbursement methodology or other similar
reimbursement methodology and another Plan that provides its benets or services on the
basis of negotiated fees, the Primary plan’s payment arrangement shall be the Allowable
expense for all Plans. However, if the provider has contracted with the Secondary plan to
provide the benet or service for a specic negotiated fee or payment amount that is dierent
from the Primary plan’s payment arrangement and if the provider’s contract permits, the
negotiated fee or payment shall be the Allowable expense used by the Secondary plan to
determine its benets.
(5) The amount of any benet reduction by the Primary plan because a covered person has failed
to comply with the Plan provisions is not an Allowable expense. Examples of these types of
Plan provisions include second surgical opinions, pre-certication or prior authorization of
admissions, and preferred provider arrangements.
E. Closed panel plan is a Plan that provides health care benets to covered persons primarily in the form
of services through a panel of providers that have contracted with or are employed by the Plan, and
that excludes coverage for services provided by other providers, except in cases of emergency or
referral by a panel member.
F. Custodial parent is the parent awarded custody by a court decree or, in the absence of a court
decree, is the parent with whom the child resides more than one half of the calendar year excluding
any temporary visitation.
Order of Benet Determination Rules
When you or your dependent are covered by two or more Plans the rules for determining the order of benet
payments are as follows:
A. The Primary plan pays or provides its benets according to its terms of coverage and without regard
to the benets under any other Plan.
B. Except as provided in the following paragraph, a Plan that does not contain a coordination of benets
provision that is consistent with this section is always primary unless the provisions of both Plans state
the complying plan is primary.
Coverage that is obtained by virtue of membership in a group that is designed to supplement a part
of a basic package of benets and provides that this supplementary coverage shall be excess to
any other parts of the Plan provided by the contract holder. Examples of these types of situations
are major medical coverages that are superimposed over base plan hospital and insurance type
coverages that are written in connection with a Closed panel plan to provide out-of-network benets.
C. A Plan may consider the benets paid or provided by another Plan in calculating payment of its
benets only when it is secondary to that other Plan.

95
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
D. Each Plan determines its order of benets using the rst of the following rules that apply:
(1) Non-Dependent or Dependent. The Plan that covers the person other than as a dependent,
for example as an employee, member, policyholder, subscriber or retiree, is the Primary plan
and the Plan that covers the person as a dependent is the Secondary plan. However, if the
person is a Medicare beneciary, and, as a result of federal law, Medicare is secondary to the
Plan covering the person as a dependent; and primary to the Plan covering the person as
other than a dependent (e.g. a retired employee); then the order of benets between the two
Plans is reversed so that the Plan covering the person as an employee, member, policyholder,
subscriber or retiree is the Secondary plan and the other Plan is the Primary plan.
(2) Dependent Child Covered Under More Than One Plan. Unless there is a court decree stating
otherwise, when a dependent child is covered by more than one Plan, the order of benets is
determined as follows:
(a) For a dependent child whose parents are married or are living together, whether or
not they have ever been married:
(i) The Plan of the parent whose birthday falls earlier in the calendar year is the
Primary plan; or
(ii) If both parents have the same birthday, the Plan that has covered the parent
the longest is the Primary plan.
(b) For a dependent child whose parents are divorced or separated or not living together,
whether or not they have ever been married:
(i) If a court decree states that one of the parents is responsible for the
dependent child’s health care expenses or health care coverage and the Plan
of that parent has actual knowledge of those terms, that Plan is primary. This
rule applies to plan years commencing after the Plan is given notice of the
court decree;
(ii) If a court decree states that both parents are responsible for the dependent
child’s health care expenses or health care coverage, the provisions of
Subparagraph (a) above shall determine the order of the benets;
(iii) If a court decree states that the parents have joint custody without specifying
that one parent has responsibility for the health care expenses or health care
coverage of the dependent child, the provisions of Subparagraph (a) above
shall determine the order of benets; or
If there is no court decree allocating responsibility for the dependent child’s health
care expenses or health care coverage, the order of benets for the child are as
follows:
(i) The Plan covering the Custodial parent;
(ii) The Plan covering the spouse of the Custodial parent;
(iii) The Plan covering the non-custodial parent; and then
(iv) The Plan covering the spouse of the non-custodial parent.
(c) For a dependent child covered under more than one Plan of individuals who are
not the parents of the child (nor the stepparents of the child), the provisions of
Subparagraph (a) or (b) above shall determine the order of benets as if those

96
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
individuals were the parents of the child.
(d) For a married dependent child covered under a spouse’s plan:
(i) For a dependent child who has coverage under either or both parents’ plans
and also has his or her own coverage as a dependent under a spouse’s plan, the rule
in Paragraph D(5) (“Longer or Shorter Length of Coverage”) applies.
(ii) In the event the dependent child’s coverage under the spouse’s plan began
on the same date as the dependent child’s coverage under either or both parents’
plans, the order of benets shall be determined by applying the Birthday Rule in
Subparagraph D(2)(a) to the dependent child’s parent(s) and the dependent’s spouse.
(3) Active Employee or Retired or Laid-O Employee. The Plan that covers a person as an active
employee, that is, an employee who is neither laid-o nor retired, is the Primary plan. The Plan
covering that same person as a retired or laid-o employee is the Secondary plan. The same
would hold true if a person is a dependent of an active employee and that same person is a
dependent of a retired or laid-o employee. If the other Plan does not have this rule, and as a
result, the Plans do not agree on the order of benets, this rule is ignored. This rule does not
apply if the rule labeled D(1) can determine the order of benets.
(4) COBRA or State Continuation Coverage. If a person whose coverage is provided pursuant to
COBRA or under a right of continuation provided by state or other federal law, or otherwise
is covered under another Plan, the Plan covering the person as an employee, member,
subscriber, or retiree or covering the person as a dependent of an employee, member,
subscriber or retiree is the Primary plan and the COBRA or state or other federal continuation
coverage is the Secondary plan. If the other Plan does not have this rule, and as a result, the
Plans do not agree on the order of benets, this rule is ignored. This rule does not apply if the
rule labeled D(1) can determine the order of benets.
(5) Longer or Shorter Length of Coverage. The Plan that covered the person as an employee,
member, policyholder, subscriber or retiree longer is the Primary plan and the Plan that
covered the person the shorter period of time is the Secondary plan.
(6) If the preceding rules do not determine the order of benets, the Allowable expenses shall be
shared equally between the Plans meeting the denition of Plan. In addition, this plan will not
pay more than it would have paid had it been the Primary plan.
Eect on the Benets of this Plan
A. When this plan is secondary, it may reduce its benets so that the total benets paid or provided
by all Plans during a plan year are not more than the total Allowable expenses. In determining the
amount to be paid for any claim, the Secondary plan will calculate the benets it would have paid
in the absence of other health care coverage and apply that calculated amount to any Allowable
expense under its Plan that is unpaid by the Primary plan. The Secondary plan may then reduce its
payment by the amount so that, when combined with the amount paid by the Primary plan, the total
benets paid or provided by all Plans for the claim do not exceed the total Allowable expense for that
claim. In addition, the Secondary plan shall credit to its plan deductible any amounts it would have
credited to its deductible in the absence of other health care coverage.
B. If a covered person is enrolled in two or more Closed panel plans and if, for any reason, including the
provisions of service by a non-panel provider, benets are not payable by one Closed panel plan, COB
shall not apply between that Plan and the other Closed panel plans.
Right to Receive and Release Needed Information
Certain facts about health care coverage and services are needed to apply these COB rules and to determine

97
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
benets payable under this plan and other Plans. The plan administrator may get the facts it needs from or
give them to other organizations or persons for the purpose of applying these rules and determining benets
payable under this Plan and other Plans covering the person claiming benets. The plan administrator need
not tell, or get the consent of any person to do this. Each person claiming benets under this plan must give
any facts it needs to apply those rules and determine benets payable.
Facility of Payment
A payment made under another Plan may include an amount that should have been paid under this plan. If it
does, the plan administrator may pay that amount to the organization that made that payment. That amount
will then be treated as though it were a benet paid under this plan. The plan administrator will not have to
pay that amount again. The term “payment made” includes providing benets in the form of services, in which
case “payment made” means the reasonable cash value of the benets provided in the form of services.
Right of Recovery
If the amount of the payments made by this plan is more than it should have paid under this COB provision,
it may recover the excess from one or more of the persons it has paid or for whom it has paid; or any other
person or organization that may be responsible for the benets or services provided for the covered person.
The “amount of the payments made” includes the reasonable cash value of any benets provided in the form
of services.

98
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
General Plan Information
The following describes other procedures and policies in eect when processing your claims.
Right to Receive and Release Necessary Information
The Plan may, without the consent of or notice to any person, release to or obtain from any organization or
person, information needed to implement Plan provisions. When you request benets, you must furnish all
the information required to implement Plan provisions. When necessary to process claims, we may require
that you submit information concerning benets to which you or your covered dependents are entitled. Such
information may include, but is not limited to, medical records pertaining to requested benets. We may also
require that you authorize any physician or provider to provide us with information about a condition for which
you claim benets.
Transfer of Benets
Only you and your covered dependents are entitled to benets under this Plan. You may not assign or transfer
your benets to anyone else, and any attempted assignment or transfer will not be binding on the Plan.
However, under normal conditions, the Plan automatically pays your and your covered dependents’ benets to
any PPO provider or PPO facility used by you or your covered dependents. Furthermore, the Plan may, in its own
discretion, make payment to any individual or organization that has assumed the care or principal support
for you and is equitably entitled to payment. Also, the Plan will make payments to your separated/divorced
spouse, state child support agencies or Medicaid agencies if required by a qualied medical child support
order (QMCSO) or state Medicaid law. The Plan may, in its discretion, honor requests made prior to your death
in relation to remaining benets payable by the Plan.
Any payment made by the in accordance with these provisions will fully release the of its
liability to you.
Recovery of Excess or Mistaken Payments
Whenever payments for services rendered to you or any of your covered dependents have been made in
excess of the amount necessary to satisfy the provisions of this Plan (including payments made by mistake
or due to fraud), the Plan has the right to (i) recover these payments from any individual (including yourself),
insurance company, provider, payer, or other organization to whom the excess payments were made or (ii)
withhold payment on your or your covered dependent’s future benets until the amount withheld equals the
amount of the overpayment.
Responsibility for Quality of Medical Care
In all cases, you or your covered dependents have the exclusive right to choose your physicians and other
providers. The Plan is not responsible for the quality of medical care you receive, since all those who provide
care do so as independent contractors. The Plan cannot be held liable for any claim or damages connected
with injuries you or your covered dependent suer while receiving medical services or supplies.
Governing Law
This Plan is governed by applicable state, territory, and federal laws.
Where Legal Action Must be Filed
Any legal action arising out of this Plan must be served on the plan administrator and must be led in the
Sixth Judicial Circuit of the State of Maryland.

99
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Time Limits for Filing A Lawsuit
Any legal action arising out of, or related to, this Plan and led against the Plan by you, any of your
dependents, any enrollee, or any third party, must be led in court within one year of the time the claim
arose. For example, a claim that benets were not pre-certied for medical necessity, and any and all
damages relating thereto, would arise when the external review process described in Article 12 of the Claims
Procedures section has ended (if an external review is requested) or upon receipt of the nal internal adverse
benet determination (in the event that an external review is not available or requested).
Plan Amendment and Termination
This Plan may be terminated or this SPD may be changed or replaced at any time without notice, by a
resolution of the North American Division Committee of the General Conference of Seventh-day Adventists,
by the North American Division Risk Management Committee, or by the delegate of North American
Division of Seventh-day Adventists, Adventist Risk Management, or any authorized representative of the
North American Division of Seventh-day Adventists or its delegate, Adventist Risk Management. The right
to amend/terminate includes the right to curtail or eliminate coverage for any treatment, procedure, or
service, regardless of whether any covered employee is receiving such treatment for an injury, defect, illness,
or disease contracted prior to the eective date of the amendment/termination. Amendments may be made
retroactively.
Eective Date of Amendment or Termination
All changes to this Plan shall become eective as of a date established by the amendment. Upon termination
or discontinuance, contributions and benets elections relating to the Plan shall terminate.
Special Election for Employees and Spouses Age 65 and Over
If you remain actively employed after reaching age 65, you or your spouse may either (1) remain covered
under this Plan without reduction for Medicare benets or (2) drop coverage under this Plan and designate
Medicare as the primary payer of benets. If you choose to remain covered under this Plan, this Plan will be
the primary payer of benets and Medicare will be secondary.
If you are under age 65 and your spouse is over age 65, this Plan will be the primary payer of benets and
Medicare will be secondary.
Claim Review
The Plan conducts appropriate claim editing procedures to examine all charges for proper billing practices,
including such things as unbundling of procedures for increased charges or wrong sex billing codes.
Health Care Fraud and Abuse
The Plan screens and audits claims for health care fraud. Under HIPAA, fraud is dened as knowingly, and
willfully executing or attempting to execute a scheme or artice (i) to defraud any healthcare benet program
or (ii) to obtain by means of false or fraudulent pretenses, representations, or promises any of the money
or property owned by any healthcare benet program. Abuse is more generally considered acts that are
inconsistent with sound medical or business practice where abuse activities cannot be clearly established as
willful or intentional misrepresentation.
The most common types of fraud, waste or abuse are misrepresentation of services with incorrect Current
Procedural Terminology (CPT) codes; billing for services not rendered; altering claim forms for higher
payments; falsication of information in medical record documents, such as International Classication of
Diseases, Ninth Revision, Clinical Modication (ICD-10-CM) codes and treatment histories; billing for services
that were not performed or misrepresenting the types of services that were provided; billing for supplies not
provided; and providing medical services that are unnecessary based on the patient’s condition.

100
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Any individual who willfully and knowingly engages in activities intended to defraud the health plan may face
consequences up to and including prosecution to the fullest extent of the law.
Health Care Claims Audits
As part of an ongoing program to provide outstanding customer service and cost-eective medical care and
as a supplement to other associated Plan initiatives, such as utilization management, the Plan shall exercise
the right to analyze claims data and carry out audit procedures. The objective of the audit process is to ensure
that the Plan fullls its responsibility to its partners, enrollees, and sponsors by identifying, correcting and
recovering inaccurate claims payments. The audit process shall conrm that claim submissions accurately
represent the services provided to Plan enrollees, and ensure that billing is conducted in accordance with
ocial guidelines and other applicable standards, rules, laws, regulations, contract provisions, policies and
procedures. Items that may be addressed during the audit may include but are not limited to the following:
1. Coding and Billing Audits which may encompass accurate application of many dierent items
such as the following:
A. Diagnosis coding,
B. Procedure coding,
C. Units or keystroke errors,
D. Diagnosis Related Grouping (DRG),
E. Ambulatory Payment Classication (APC),
F. Ambulatory surgery payment groupings (ASC),
G. Discharge disposition,
H. Present on Admission (POA) indicators,
I. HAC, Medical/Surgical Misadventure or Medical Never Event,
J. National Correct Coding Initiative (NCCI) edits,
K. Outpatient Code Editor (OCE) edits,
L. Modiers, etc.
2. Charge Audits may encompass not only accuracy of the charges but appropriateness of
the charges when items may not be consistent with uniform billing practices (for example,
unbundling of items from the room rate such as venipuncture, pulse oximetry, oxygen, oor
stock supplies, etc.).
3. Assessing if services provided were reasonable and necessary (for example, level of care or
setting, experimental and investigational usage of drugs or devices).
4. Covered Services.
5. Readmissions up to 30 days.
6. Eligibility Audits, which may include dependent verication.

101
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
No Waiver
Failure of the plan administrator or your employer to insist upon compliance with any provision of this Plan at
any given time or times or under any given set or sets of circumstances shall not operate to waive or modify
such provision or in any manner whatsoever to render it unenforceable, as to any other time or times or as to
any other occurrence or occurrences, whether the circumstances are, or are not, the same.
Rights Under Newborns’ and Mothers’ Health Protection Act
Under federal law, group health plans such as this Plan generally may not restrict benets for any hospital
length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following a
vaginal delivery, or less than 96 hours following a delivery by cesarean section. However, the plans may pay
for a shorter stay if the attending provider (e.g., your physician, nurse midwife, or physician assistant), after
consultation with the mother, discharges the mother or newborn earlier. Also, under federal law, plans may
not set the level of benets or out-of-pocket costs so that any later portion of the 48 hour (or 96 hour) stay is
treated in a manner less favorable to the mother or newborn than any earlier portion of the stay. In addition, a
plan may not, under federal law, require that a physician or other healthcare provider obtain authorization for
prescribing a length of stay of up to 48 hours (or 96 hours).
Rights Under the Women’s Health and Cancer Rights Act
The Women’s Health and Cancer Rights Act of 1998 requires that health plans cover post-mastectomy
reconstructive breast surgery if they provide medical and surgical coverage for mastectomies. Specically,
health plans must cover:
1. Reconstruction of the breast on which the mastectomy has been performed;
2. Surgery and reconstruction of the other breast to produce a symmetrical appearance; and
3. Prostheses and physical complications of all stages of mastectomy, including lymph edemas.
Benets required under the Women’s Health and Cancer Rights Act will be provided in consultation between
the patient and attending physician. These benets are subject to the Plan’s regular co-payments and
deductibles. These types of benets are provided under this Plan.
Section 125 Cafeteria Plan
Your employer may participate in and oer a Section 125 Cafeteria Plan program at your workplace. (Section
125 refers to the section of the Internal Revenue Code authorizing cafeteria plans.) Section 125 programs may
allow employees to elect to contribute part of their salary to be used to pay, on a pre-tax basis:
1. qualifying out-of-pocket medical expenses not reimbursed by this Plan or any other health plan or
insurance, such as co-payments, deductibles and co-insurance; and
2. contributions or premiums, if any, required to be paid for Plan coverage.
If your employer has a Section 125 program, there are restrictions on when you are allowed to enroll in the
program and when you can change your elections and coverage under the program. Please contact your
employer for more information about these restrictions and other requirements and features of the Section
125 program.

102
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Health Insurance Portability and Accountability Act Provisions
(HIPAA Privacy Policy)
The Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) protects the privacy of certain
types of individual health information, regulates the use of such information by the Plan and imposes certain
security protection measures concerning electronic health information. The Department of Health and
Human Services has issued regulations on this subject that can be found at 45 CFR parts 160 and 164 (“HIPAA
Regulations”). In this HIPAA Privacy Policy, the terms “you” and “your” refer to the Plan member/enrollee. The
individual health information that is protected (“Protected Health Information” or “PHI”) is any information
created or received by the Plan that relates to:
1. Your past, present or future physical or mental health or your past, present or future physical or
mental condition
2. the provision of healthcare to you or
3. past, present, or future payment for healthcare.
However, HIPAA allows medical information, including PHI, to be disclosed by the Plan to the Plan Sponsor
and to be used by the Plan Sponsor. (This Plan limits any such disclosures to the Plan Sponsor’s designated
Benet Coordinator and Controlling Committee.) The permitted disclosures to and uses by the Plan Sponsor
of medical information are as follows:
1. The Plan may disclose summary health information to the Plan Sponsor if the Plan Sponsor requests
the summary information for the purpose of
a. obtaining premium bids for providing insurance coverage; or
b. modifying, amending, or terminating the Plan (“Summary Information”). The Plan Sponsor may use
Summary Information so received from the Plan only for these two listed purposes.
2. The Plan may disclose to the Plan Sponsor, and the Plan Sponsor may use, information on whether an
individual is participating in the Plan or is enrolling or dis-enrolling in the Plan.
3. The Plan may disclose PHI to the Plan Sponsor and/or the Plan Sponsor may use such PHI if you have
specically authorized in writing such disclosure and/or use.
4. The Plan may disclose PHI to the Plan Sponsor, and the Plan Sponsor may use PHI, to carry out plan
administration functions, such as activities relating to:
a. obtaining employee-share contributions or to determining or fullling responsibility for coverage
and provision of benets under the Plan
b. payment for or obtaining or providing reimbursement for healthcare services - Payments under
this Plan generally are made either to the healthcare provider or to the employee. All Members
should be aware that the Plan and the Plan Sponsor will be providing PHI concerning all
dependents of an employee to the employee as part of the Explanation of Benets and when
reimbursing the employee for covered services under the Plan. If there is some reason why a
dependent (spouse or child) of an employee does not want the employee to receive PHI, the
dependent should so inform his or her healthcare provider and should also contact the Plan
Administrator
c. determining eligibility for the Plan or eligibility for one or more types of coverage or benets
provided under the Plan
d. coordination of benets or determinations of co-payments or other cost sharing mechanisms

103
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
e. adjudication and subrogation of claims, billing, claims management, collection activities and
related healthcare data processing
f. payment under a contract for reinsurance
g. review of healthcare services with respect to medical necessity, coverage under the health plan,
appropriateness of care, or justication of charges
h. utilization review activities, including pre-certication and preauthorization of services and
concurrent and retrospective review of services
i. disclosure to consumer reporting agencies of any of the following PHI regarding collection of
premiums or reimbursement: name and address, date of birth, Social Security Number, payment
history, account number and name and address of the health plan
j. medical review, legal services and auditing functions, including fraud and abuse detection and
compliance programs
k. business planning and development, such as conducting cost-management and planning-
related analyses relating to managing and operating the Plan, including formulary development
and administration and/or the development or improvement of methods of payment
l. resolution of internal grievances
m. prosecution or defense of administrative claims or lawsuits involving the Plan or Plan Sponsor
n. conducting quality assurance and improvement activities, case management and care
coordination
o. evaluating healthcare provider performance or Plan performance
p. securing or placing a contract for reinsurance of risk relating to healthcare claims, other activities
relating to the renewal or replacement of stop-loss or excess of loss insurance
q. contacting healthcare providers and patients with information about treatment alternatives These
uses and disclosures are consistent with HIPAA Regulations.
The Plan Sponsor has agreed to (and the Plan has received a certication from the Plan Sponsor evidencing
such agreement) the following restrictions:
1. The Plan Sponsor will not use or further disclose the PHI except as described above or as otherwise
required by law.
2. Any agents or subcontractors of the Plan Sponsor to whom the Plan Sponsor provides PHI will
agree to the same restrictions and conditions on the use and disclosure of PHI that apply to the
Plan Sponsor. Any agents or subcontractors of the Plan Sponsor to whom the Plan Sponsor provides
electronic PHI must agree to implement reasonable and appropriate security measures to protect the
information.
3. The Plan Sponsor will not use or disclose PHI for employment-related actions and decisions or in
connection with any other benet or employee benet plan of the Plan Sponsor.
4. The Plan Sponsor will report to the Plan any use or disclosure of the PHI that is inconsistent with the
permitted uses and disclosures of which the Plan Sponsor becomes aware. The Plan Sponsor will
report to the Plan any security incident of which the Plan Sponsor becomes aware.
5. The Plan Sponsor will (or will cooperate with the plan administrator to) give you access and provide

104
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
copies to you of your PHI in accordance with the HIPAA Regulations.
6. The Plan Sponsor will (or will cooperate with the plan administrator to) allow you to amend your PHI in
accordance with the HIPAA Regulations.
7. The Plan Sponsor will (or will cooperate with the plan administrator to) make available PHI to you in
order to make an accounting of PHI in accordance with the HIPAA Regulations.
8. The Plan Sponsor will (or will cooperate with the plan administrator to) make available its internal
practices, books and records relating to the use and disclosure of PHI received from the Plan to the
Secretary of Health and Human Services (or the Secretary’s designee) for determining compliance by
the Plan with the HIPAA Regulations.
9. The Plan Sponsor will, if feasible, return or destroy all protected PHI received from the Plan and retain
no copies of the PHI when no longer needed for the purpose for which the disclosure was made,
except that, if such return or destruction is not feasible, limit further uses and disclosures to those
purposes that make the return or destruction of the PHI infeasible.
10. The Plan Sponsor will ensure that adequate separation between the Plan and Plan Sponsor is
established. Only the following employees or classes of employees or other persons under the
control of the Plan Sponsor will be given access to the PHI to be disclosed:
a. Ocers of the Plan Administrator
b. Employees of the Plan Administrator
c. Plan Sponsor’s designated Benet Coordinator and Controlling Committee
11. The Plan Sponsor will ensure that this adequate separation is supported by reasonable and
appropriate security measures to the extent that these individuals have access to electronic PHI.
12. The Plan Sponsor will (and will cooperate with the plan administrator to) implement administrative,
physical and technical safeguards that reasonably and appropriately protect the condentiality,
integrity and availability of electronic PHI that the Plan Sponsor creates, receives, maintains or
transmits on behalf of the Plan, except enrollment/disenrollment information and Summary
Information, which are not subject to these restrictions.
The access to and use by the employees described above is limited to the plan administration functions that
the Plan Sponsor (and the Plan Sponsor’s delegee, the Plan Administrator) performs for the Plan. Employees
who violate this section are subject to disciplinary action by the Plan Sponsor, including, but not limited to,
reprimands and termination.
The Plan has issued a Privacy Notice which explains the Plan’s privacy practices and your rights under HIPAA.
This Notice is available by contacting the Plan’s Privacy/Security Ocer at the following address:
Adventist Risk Management, 12501 Old Columbia Pike, Silver Spring, MD 20904 or email,
privacyocer@adventistrisk.org. The Privacy Notice is also available at www.AscendtoWholeness.org.
Release of Medical Information
Any employee covered by the Plan, on behalf of himself or herself and the employee’s covered dependents,
shall be deemed to have authorized any attending physician, nurse, hospital, or other provider of services or
supplier to furnish the plan administrator with all information and records or copies of records relating to the
diagnosis, treatment, or care of any person covered by the Plan. Members shall, by asserting a claim for Plan
benets, be deemed to have waived all provisions of law forbidding the disclosure of such information and
records. If so requested or required by law, each Member shall sign any release or authorization form in order
to facilitate the release of such medical records.

105
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Furnishing Information
A person covered by the Plan must furnish all information needed to eect coverage under the Plan and
termination or changes in such coverage. The plan administrator may require that a Member provide certain
personal data (including reasonable proof of the accuracy of the data) necessary for the determination of
the person’s benets. Failure to furnish the data (or proof of its accuracy) may delay the payment of benets.
Benet payments may be adjusted to reect correction of inaccurate or incomplete information, and an
employee, other Member and/or medical provider may be required to make up any overpayments, and the
Plan may make up any underpayments.

106
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Medicare Part D Notice
Important Notice from the Plan About Your Prescription Drug Coverage and Medicare
You are responsible for providing a copy of this notice to your Medicare-eligible dependents
Please read this notice carefully and keep it where you can nd it. This notice has information about your
current prescription drug coverage with the Plan and about your options under Medicare’s prescription
drug coverage. This information can help you decide whether or not you want to join a Medicare drug
plan. If you are considering joining, you should compare your current coverage, including which drugs
are covered at what cost, with the coverage and costs of the plans oering Medicare prescription
drug coverage in your area. Information about where you can get help to make decisions about your
prescription drug coverage is at the end of this notice.
There are two important things you need to know about your current coverage and Medicare’s
prescription drug coverage:
1. Medicare prescription drug coverage became available in 2006 to everyone with Medicare. You
can get this coverage if you join a Medicare Prescription Drug Plan or join a Medicare Advantage
Plan (like an HMO or PPO) that oers prescription drug coverage. All Medicare drug plans provide
at least a standard level of coverage set by Medicare. Some plans may also oer more coverage
for a higher monthly premium.
2. The Plan has determined that the prescription drug coverage oered by the Plan is, on average
for all plan participants, expected to pay out as much as standard Medicare prescription drug
coverage pays and is therefore considered Creditable Coverage. Because your existing coverage
is Creditable Coverage, you can keep this coverage and not pay a higher premium (a penalty) if
you later decide to join a Medicare drug plan.
When Can You Join A Medicare Drug Plan?
You can join a Medicare drug plan when you rst become eligible for Medicare and each year from October
15th to December 7th.
However, if you lose your current creditable prescription drug coverage, through no fault of your own, you will
also be eligible for a two (2) month Special Enrollment Period (SEP) to join a Medicare drug plan.
What Happens To Your Current Coverage If You Decide to Join A Medicare Drug Plan?
If you elect Medicare Part D coverage and maintain your Plan coverage, your Plan coverage will coordinate
with Part D coverage. In most instances, the Plan will pay prescription drug benets as the primary payer
and Medicare will pay secondary, and therefore the value of your Medicare Part D coverage will be greatly
reduced.
If you decide to join a Medicare drug plan and drop your current Plan coverage, be aware that if you are no
longer an active employee with a participating employer, you and your dependents may not be able to get
this coverage back. If you are an active employee with a participating employer, you can get this coverage
back, but not until the next open enrollment period (unless you have qualifying change in status and your
requested change is on account of and corresponds with the event you experience).
When Will You Pay A Higher Premium (Penalty) To Join A Medicare Drug Plan?
You should also know that if you drop or lose your current coverage with the Plan and don’t join a Medicare
drug plan within 63 continuous days after your current coverage ends, you may pay a higher premium (a
107
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
penalty) to join a Medicare drug plan later.
If you go 63 continuous days or longer without creditable prescription drug coverage, your monthly premium
may go up by at least 1% of the Medicare base beneciary premium per month for every month that you did
not have that coverage. For example, if you go nineteen months without creditable coverage, your premium
may consistently be at least 19% higher than the Medicare base beneciary premium. You may have to pay
this higher premium (a penalty) as long as you have Medicare prescription drug coverage. In addition, you
may have to wait until the following October to join.
For More Information About This Notice Or Your Current Prescription Drug Coverage…
Contact Adventist Risk Management at 1-888-276-4732. NOTE: You’ll get this notice each year. You will
also get it before the next period you can join a Medicare drug plan, and if this coverage through the Plan
changes. You also may request a copy of this notice at any time.
For More Information About Your Options Under Medicare Prescription Drug Coverage…
More detailed information about Medicare plans that oer prescription drug coverage is in the “Medicare
& You” handbook. You’ll get a copy of the handbook in the mail every year from Medicare. You may also be
contacted directly by Medicare drug plans. For more information about Medicare prescription drug coverage:
• Visit www.medicare.gov
• Call your State Health Insurance Assistance Program (see the inside back cover of your copy of the
“Medicare & You” handbook for their telephone number) for personalized help
• Call 1-800-MEDICARE (1-800-633-4227). TTY users should call 1-877-486-2048.
If you have limited income and resources, extra help paying for Medicare prescription drug coverage is
available. For information about this extra help, visit Social Security on the web at www.socialsecurity.gov, or
call them at 1-800-772-1213 (TTY 1-800-325-0778).
Remember: Keep this Creditable Coverage notice. If you decide to join one of the Medicare drug
plans, you may be required to provide a copy of this notice when you join to show whether or not you
have maintained creditable coverage and, therefore, whether or not you are required to pay a higher
premium (a penalty).
Date: December 1, 2020
Name of Entity/Sender: Healthcare Assistance Plan for Employees of the Seventh-day Adven-
tist Organizations of the North American Division (USA) of the General
Conference of Seventh-day Adventist (“Plan”), by its Plan Administrator,
Adventist Risk Management, Inc.
Contact--Position/Oce: Plan Administrator
Address: 12501 Old Columbia Pike, Silver Spring, MD 20904
Phone Number: 888-ARM-4SDA or 888-276-4732

108
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Premium Assistance Under Medicaid and the Children’s Health
Insurance Program (CHIP)
If you or your children are eligible for Medicaid or CHIP and you’re eligible for health coverage from your
employer, your state may have a premium assistance program that can help pay for coverage, using funds
from their Medicaid or CHIP programs. If you or your children aren’t eligible for Medicaid or CHIP, you won’t be
eligible for these premium assistance programs but you may be able to buy individual insurance coverage
through the Health Insurance Marketplace. For more information, visit www.healthcare.gov.
If you or your dependents are already enrolled in Medicaid or CHIP and you live in a State listed below,
contact your State Medicaid or CHIP oce to nd out if premium assistance is available.
If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and you think you or any of your
dependents might be eligible for either of these programs, contact your State Medicaid or CHIP oce or dial
1-877-KIDS NOW or www.insurekidsnow.gov to nd out how to apply. If you qualify, ask your state if it has a
program that might help you pay the premiums for an employer-sponsored plan.
If you or your dependents are eligible for premium assistance under Medicaid or CHIP, as well as eligible
under your employer plan, your employer must allow you to enroll in your employer plan if you aren’t already
enrolled. This is called a “special enrollment” opportunity, and you must request coverage within 60 days of
being determined eligible for premium assistance (as extended by the temporary deadline extension due
to the COVID-19 pandemic described in Appendix F). If you have questions about enrolling in your employer
plan, contact the Department of Labor at www.askebsa.dol.gov or call 1-866-444-EBSA (3272).
If you live in one of the following states, you may be eligible for assistance paying your employer health
plan premiums. The following list of states is current as of July 31, 2020. Contact your State for more
information on eligibility –
ALABAMA – Medicaid COLORADO – Health First Colorado (Colorado’s Medicaid Program)
& Child Health Plan Plus (CHP+)
Website: http://myalhipp.com/
Phone: 1-855-692-5447
Health First Colorado Website:
https://www.healthrstcolorado.com/
Health First Colorado Member Contact Center:
1-800-221-3943/ State Relay 711
CHP+: https://www.colorado.gov/pacic/hcpf/child-health-plan-plus
CHP+ Customer Service: 1-800-359-1991/ State Relay 711
Health Insurance Buy-In Program (HIBI):
https://www.colorado.gov/pacic/hcpf/health-insurance-buy-program
HIBI Customer Service: 1-855-692-6442
ALASKA – Medicaid FLORIDA – Medicaid
The AK Health Insurance Premium Payment Program Website:
http://myakhipp.com/
Phone: 1-866-251-4861
Email: CustomerService@MyAKHIPP.com
Medicaid Eligibility:
http://dhss.alaska.gov/dpa/Pages/medicaid/default.aspx
Website: https://www.medicaidtplrecovery.com/medicaidtplrecovery.
com/hipp/index.html
Phone: 1-877-357-3268
ARKANSAS – Medicaid GEORGIA – Medicaid
Website: http://myarhipp.com/
Phone: 1-855-MyARHIPP (855-692-7447)
Website: https://medicaid.georgia.gov/health-insurance-premium-
payment-program-hipp
Phone: 678-564-1162 ext 2131
CALIFORNIA – Medicaid INDIANA – Medicaid
Website: https://www.dhcs.ca.gov/services/Pages/TPLRD_
CAU_cont.aspx
Phone: 916-440-5676
Healthy Indiana Plan for low-income adults19-64
Website: http://www.in.gov/fssa/hip/
Phone: 1-877-438-4479
All other Medicaid
Website: https://www.in.gov/medicaid/
Phone 1-800-457-4584
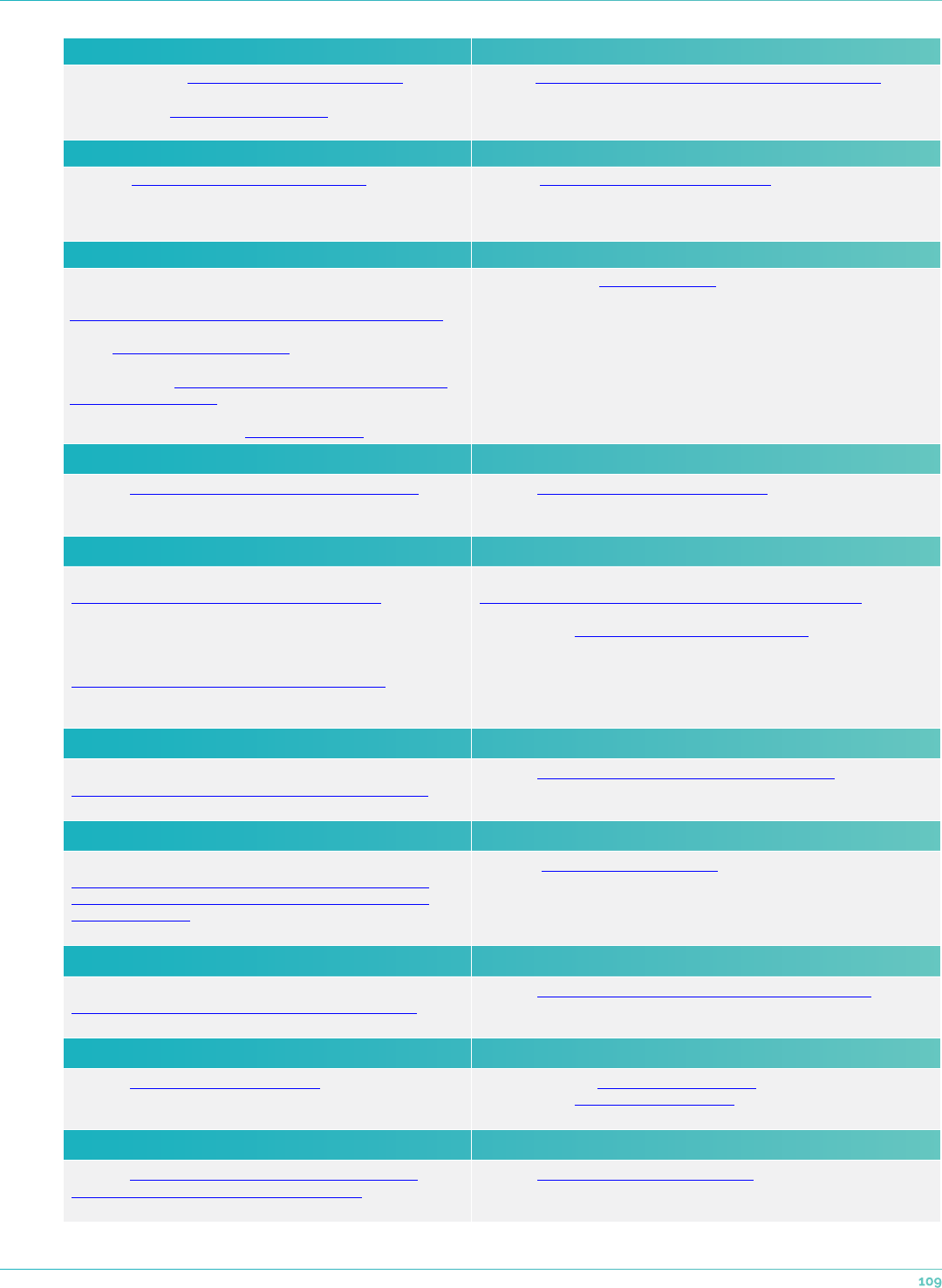
109
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
IOWA – Medicaid and CHIP (Hawki) MONTANA – Medicaid
Medicaid Website: https://dhs.iowa.gov/ime/members
Medicaid Phone: 1-800-338-8366
Hawki Website: http://dhs.iowa.gov/Hawki
Hawki Phone: 1-800-257-8563
Website: http://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP
Phone: 1-800-694-3084
KANSAS – Medicaid NEBRASKA – Medicaid
Website: http://www.kdheks.gov/hcf/default.htm
Phone: 1-800-792-4884
Website: http://www.ACCESSNebraska.ne.gov
Phone: 1-855-632-7633
Lincoln: 402-473-7000
Omaha: 402-595-1178
KENTUCKY – Medicaid NEVADA – Medicaid
Kentucky Integrated Health Insurance Premium Payment Pro-
gram (KI-HIPP) Website:
https://chfs.ky.gov/agencies/dms/member/Pages/kihipp.aspx
Phone: 1-855-459-6328
Email: KIHIPP.PROGRAM@ky.gov
KCHIP Website: https://kidshealth.ky.gov/Pages/index.aspx
Phone: 1-877-524-4718
Kentucky Medicaid Website: https://chfs.ky.gov
Medicaid Website: http://dhcfp.nv.gov
Medicaid Phone: 1-800-992-0900
LOUISIANA – Medicaid NEW HAMPSHIRE – Medicaid
Website: www.medicaid.la.gov or www.ldh.la.gov/lahipp
Phone: 1-888-342-6207 (Medicaid hotline) or 1-855-618-5488
(LaHIPP)
Website: https://www.dhhs.nh.gov/oii/hipp.htm
Phone: 603-271-5218
Toll free number for the HIPP program: 1-800-852-3345, ext 5218
MAINE – Medicaid NEW JERSEY – Medicaid and CHIP
Enrollment Website:
https://www.maine.gov/dhhs/o/applications-forms
Phone: 1-800-442-6003
TTY: Maine relay 711
Private Health Insurance Premium Webpage:
https://www.maine.gov/dhhs/o/applications-forms
Phone: -800-977-6740.
TTY: Maine relay 711
Medicaid Website:
http://www.state.nj.us/humanservices/dmahs/clients/medicaid/
Medicaid Phone: 609-631-2392
CHIP Website: http://www.njfamilycare.org/index.html
CHIP Phone: 1-800-701-0710
MASSACHUSETTS – Medicaid and CHIP NEW YORK – Medicaid
Website:
http://www.mass.gov/eohhs/gov/departments/masshealth/
Phone: 1-800-862-4840
Website: https://www.health.ny.gov/health_care/medicaid/
Phone: 1-800-541-2831
MINNESOTA – Medicaid NORTH CAROLINA – Medicaid
Website:
https://mn.gov/dhs/people-we-serve/children-and-families/
health-care/health-care-programs/programs-and-services/
other-insurance.jsp
Phone: 1-800-657-3739
Website: https://medicaid.ncdhhs.gov/
Phone: 919-855-4100
MISSOURI – Medicaid NORTH DAKOTA – Medicaid
Website:
http://www.dss.mo.gov/mhd/participants/pages/hipp.htm
Phone: 573-751-2005
Website: http://www.nd.gov/dhs/services/medicalserv/medicaid/
Phone: 1-844-854-4825
OKLAHOMA – Medicaid and CHIP UTAH – Medicaid and CHIP
Website: http://www.insureoklahoma.org
Phone: 1-888-365-3742
Medicaid Website: https://medicaid.utah.gov/
CHIP Website: http://health.utah.gov/chip
Phone: 1-877-543-7669
OREGON – Medicaid VERMONT – Medicaid
Website: http://healthcare.oregon.gov/Pages/index.aspx
http://www.oregonhealthcare.gov/index-es.html
Phone: 1-800-699-9075
Website: http://www.greenmountaincare.org/
Phone: 1-800-250-8427

110
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
PENNSYLVANIA – Medicaid VIRGINA – Medicaid and CHIP
Website: https://www.dhs.pa.gov/providers/Providers/Pages/
Medical/HIPP-Program.aspx
Phone: 1-800-692-7462
Website: https://www.coverva.org/hipp/
Medicaid Phone: 1-800-432-5924
CHIP Phone: 1-855-242-8282
RHODE ISLAND – Medicaid and CHIP WASHINGTON – Medicaid
Website: http://www.eohhs.ri.gov/
Phone: 1-855-697-4347, or 401-462-0311 (Direct RIte Share
Line)
Website: https://www.hca.wa.gov/
Phone: 1-800-562-3022
SOUTH CAROLINA – Medicaid WEST VIRGINIA – Medicaid
Website: https://www.scdhhs.gov
Phone: 1-888-549-0820
Website: http://www.mywvhipp.com/
Toll-free phone: 1-855-MyWVHIPP (1-855-699-8447)
SOUTH DAKOTA – Medicaid WISCONSIN – Medicaid and CHIP
Website: http://dss.sd.gov
Phone: 1-888-828-0059
Website:
https://www.dhs.wisconsin.gov/badgercareplus/p-10095.htm
Phone: 1-800-362-3002
TEXAS – Medicaid WYOMING – Medicaid
Website: http://gethipptexas.com/
Phone: 1-800-440-0493
Website:
https://health.wyo.gov/healthcaren/medicaid/programs-and-eligibility/
Phone: 1-800-251-1269
To see if any other states have added a premium assistance program since July 31, 2020, or for more
information on special enrollment rights, contact either:
U.S. Department of Labor
Employee Benets Security Administration
https://www.dol.gov/agencies/ebsa
1-866-444-EBSA (3272)
U.S. Department of Health and Human Services
Centers for Medicare & Medicaid Services
https://www.cms.hhs.gov/
1-877-267-2323, Menu Option 4, Ext. 61565

111
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
APPENDIX A – List of Covered Preventive Services
Preventive care benets for adults –
See below or go to https://www.healthcare.gov/preventive-care-adults/
Preventive care benets for women –
See below or go to https://www.healthcare.gov/preventive-care-women/
Preventive care benets for children –
See below or go to https://www.healthcare.gov/preventive-care-children/

112
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Preventive care benets for adults
IMPORTANT
These services are free only when delivered by a doctor or other provider in your plan’s network.
1. Abdominal aortic aneurysm one-time screening (https://healthnder.gov/HealthTopics/
Category/doctor-visits/screening-tests/talk-to-your-doctor-about-abdominal-aortic-
aneurysm) for men of specied ages who have ever smoked.
2. AlcohoI misuse screening and counseling (https://healthnder.gov/HealthTopics/Category/
health-conditions-and-diseases/heart-health/drink-alcohol-only-in-moderation).
3. Aspirin use (https://healthnder.gov/HealthTopics/Category/health-conditions-and-diseases/
heart-health/talk-with-your-doctor-about-taking-aspirin-every-day) to prevent cardiovascular
disease and colorectal cancer for adults 50 to 59 years with a high cardiovascular risk.
4. Blood pressure screening (https://health.gov/myhealthnder/topics/doctor-visits/screening-
tests/get-your-blood-pressure-checked).
5. ChoIesteroI screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/get-your-cholesterol-checked) for adults of certain ages or at higher risk.
6. ColorectaI cancer screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/get-tested-for-colorectal-cancer) for aduIts 45 to 75.
7. Depression screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/talk-with-your-doctor-about-depression).
8. Diabetes (Type 2) screening (https://healthnder.gov/HealthTopics/Category/health-
conditions-and-diseases/diabetes/take-steps-to-prevent-type-2-diabetes) for adults 40 to 70
years who are overweight or obese.
9. Diet Counseling (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/diabetes/eat-healthy) for adults at higher risk for chronic disease.
10. Falls prevention (https://healthnder.gov/HealthTopics/Population/older-adults/safety/
preventing-falls-conversation-starters) (with exercise or physical therapy and vitamin D use) for
adults 65 years and over, living in a community setting.
11. Hepatitis B screening (https://www.uspreventiveservicestaskforce.org/uspstf/
recommendation/hepatitis-b-virus-infection-screening?ds=1&s=hepatitis%20b) for people at
high risk, including people from countries with 2% or more Hepatitis B prevalence, and U.S.-born
people not vaccinated as infants and with at least one parent born in a region with 8% or more
Hepatitis B prevalence.
12. Hepatitis C screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/talking-
with-the-doctor/hepatitis-c-screening) for adults at increased risk, and one time for everyone
born 1945 - 1965.
13. HIV screening (https://health.gov/myhealthnder/topics/health-conditions/hiv-and-other-
stds/get-tested-hiv) for everyone ages 15 to 65, and other ages at increased risk.
14. Immunization vaccines (https://healthnder.gov/HealthTopics/Category/doctor-visits/

113
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
shotsvaccines/get-important-shots) for adults - doses, recommended ages, and recommended
populations vary:
• Diphtheria (https://www.vaccines.gov/diseases/diphtheria/index.html)
• Hepatitis A (https://www.vaccines.gov/diseases/hepatitis_a/index.html)
• Hepatitis B (https://www.vaccines.gov/diseases/hepatitis_b/index.html)
• Herpes Zoster (https://www.vaccines.gov/diseases/shingles/index.html)
• Human Papillomavirus (HPV) (https://www.vaccines.gov/diseases/hpv/index.html)
• Inuenza (u shot) (https://www.vaccines.gov/diseases/u/index.html)
• Measles (https://www.vaccines.gov/diseases/measles/index.html)
• MeningococcaI (https://www.vaccines.gov/diseases/meningitis/index.html)
• Mumps (https://www.vaccines.gov/diseases/mumps/index.html)
• Pertussis (https://www.vaccines.gov/diseases/pertussis/index.html)
• PneumococcaI (https://www.vaccines.gov/diseases/pneumonia/index.html)
• Rubella (https://www.vaccines.gov/diseases/rubella/index.html)
• Tetanus (https://www.vaccines.gov/diseases/tetanus/index.html)
• Varicella (Chicken pox) (https://www.vaccines.gov/diseases/chickenpox/index.html)
15. Lung cancer screening (https://www.uspreventiveservicestaskforce.org/Page/Topic/
recommendation-summary/lung-cancer-screening) for adults 50 - 80 at high risk for lung cancer
because they’re heavy smokers or have quit in the past 15 years.
16. Obesity screening and Counseling (https://healthnder.gov/HealthTopics/Category/health-
conditions-and-diseases/diabetes/watch-your-weight).
17. Sexually transmitted infection (STI) prevention counseling (https://healthnder.gov/healthtopics/
category/health-conditions-and-diseases/hiv-and-other-stds) for adults at higher risk.
18. Statin preventive medication (https://healthnder.gov/healthtopics/category/doctor-visits/
talking-with-the-doctor/medicines-to-prevent-heart-attack-and-stroke-questions-for-the-
doctor) for adults 40 to 75 at high risk
19. Syphilis screening (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/hiv-and-other-stds/syphilis-testing-questions-for-the-doctor) for adults at higher risk.
20. Tobacco Use screening (https://health.gov/myhealthnder/topics/health-conditions/
diabetes/quit-smoking) for all adults and cessation interventions for tobacco users.
21. Tuberculosis screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/talking-
with-the-doctor/testing-for-latent-tuberculosis) for certain adults without symptoms at high risk.
MORE ON PREVENTION
• Learn more about preventive care from the CDC (https://www.cdc.gov/prevention/).
• See preventive services covered for children (https://www.healthcare.gov/preventive-care-
children/) and women (https://www.healthcare.gov/preventive-care-women/).
• Learn more about what else Marketplace health insurance plans cover (https://www.healthcare.
gov/coverage/what-marketplace-plans-cover/).

114
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Preventive care benets for women
IMPORTANT
These services are free only when delivered by a doctor or other provider in your plan’s network.
Services for pregnant women or women who may become pregnant:
1. Anemia screening (https://healthnder.gov/HealthTopics/Category/pregnancy/doctor-and-
midwife-visits/have-a-healthy-pregnancy) on a routine basis.
2. Breastfeeding comprehensive support and counseling (https://healthnder.gov/HealthTopics/
Category/pregnancy/getting-ready-for-your-baby/breastfeed-your-baby) from trained
providers, and access to breastfeeding supplies, for pregnant and nursing women.
3. Contraception (https://health.gov/myhealthnder/topics/everyday-healthy-living/sexual-
health/choose-right-birth-control): Food and Drug Administration-approved contraceptive
methods, sterilization procedures, and patient education and counseling, as prescribed by a health
care provider for women with reproductive capacity (not including abortifacient drugs). This does
not apply to health plans sponsored by certain exempt “religious employers.” Learn more about
contraceptive coverage (https://www.healthcare.gov/coverage/birth-control-benets/).
4. Folic acid (https://health.gov/myhealthnder/topics/everyday-healthy-living/nutrition/get-
enough-folic-acid) supplements for women who may become pregnant.
5. Gestational diabetes screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
talking-with-the-doctor/gestational-diabetes-screening-questions-for-the-doctor) for women
24 to 28 weeks pregnant and those at high risk of developing gestational diabetes.
6. Gonorrhea screening (https://health.gov/myhealthnder/topics/health-conditions/hiv-and-
other-stds/get-tested-chlamydia-and-gonorrhea) for all women at higher risk.
7. Hepatitis B screening (https://healthnder.gov/HealthTopics/Category/pregnancy/doctor-and-
midwife-visits/have-a-healthy-pregnancy) for pregnant women at their rst prenatal visit.
8. Preeclampsia prevention and screening (https://healthnder.gov/healthtopics/category/
pregnancy/doctor-and-midwife-visits/preventing-preeclampsia-questions-for-the-doctor) for
pregnant women with high blood pressure.
9. Rh Incompatibility screening (https://healthnder.gov/HealthTopics/Category/pregnancy/
doctor-and-midwife-visits/have-a-healthy-pregnancy) for all pregnant women and follow-up
testing for women at higher risk.
10. Syphilis screening (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/hiv-and-other-stds/syphilis-testing-questions-for-the-doctor).
11. Expanded tobacco intervention and counseling (https://healthnder.gov/HealthTopics/
Category/health-conditions-and-diseases/diabetes/quit-smoking) for pregnant tobacco users.
12. Urinary tract or other infection screening (https://healthnder.gov/HealthTopics/Category/
pregnancy/doctor-and-midwife-visits/have-a-healthy-pregnancy)
Get more information about services for pregnant women from HealthFinder.gov (https://healthnder.
gov/HealthTopics/Category/pregnancy/doctor-and-midwife-visits/have-a-healthy-pregnancy)

115
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Other covered preventive services for women:
1. Breast cancer genetic test counseling (BRCA) (https://healthnder.gov/HealthTopics/Category/
health-conditions-and-diseases/cancer/talk-with-a-doctor-if-breast-or-ovarian-cancer-runs-in-
your-family) for women at higher risk.
2. Breast cancer mammography screenings (https://health.gov/myhealthnder/topics/health-
conditions/cancer/get-tested-breast-cancer) every 1 to 2 years for women over 40.
3. Breast cancer chemoprevention counseling (https://healthnder.gov/HealthTopics/Category/
health-conditions-and-diseases/cancer/talk-with-a-doctor-if-breast-or-ovarian-cancer-runs-in-
your-family) for women at higher risk.
4. Cervical cancer screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/get-screened-for-cervical-cancer) Pap test (also called a Pap smear) every 3 years
for women 21 to 65 or Human Papillomavirus (HPV) DNA test with the combination of a Pap smear
every 5 years for women 30 to 65 who don’t want a Pap smear every 3 years.
5. Chlamydia infection screening (https://healthnder.gov/HealthTopics/Category/health-
conditions-and-diseases/hiv-and-other-stds/get-tested-for-chlamydia-and-gonorrhea) for
younger women and other women at higher risk.
6. Diabetes screening (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/diabetes) for women with a history of gestational diabetes who aren’t currently pregnant
and who haven’t been diagnosed with type 2 diabetes before.
7. Domestic and interpersonal violence screening and counseling (https://healthnder.gov/
HealthTopics/Category/everyday-healthy-living/mental-health-and-relationship/watch-for-
warning-signs-of-relationship-violence) for all women.
8. Gonorrhea screening (https://health.gov/myhealthnder/topics/health-conditions/hiv-and-
other-stds/get-tested-chlamydia-and-gonorrhea) for all women at higher risk.
9. HIV screening and counseling (https://healthnder.gov/HealthTopics/Category/health-
conditions-and-diseases/hiv-and-other-stds/get-tested-for-hiv) for sexually active women.
10. Osteoporosis screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/get-a-bone-density-test) for women over age 60 depending on risk factors.
11. Rh incompatibility screening (https://healthnder.gov/HealthTopics/Category/pregnancy/
doctor-and-midwife-visits/have-a-healthy-pregnancy) follow-up testing for women at higher risk.
12. Sexually transmitted infections counseling (https://healthnder.gov/healthtopics/category/
health-conditions-and-diseases/hiv-and-other-stds) for sexually active women.
13. Syphilis screening (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/hiv-and-other-stds/syphilis-testing-questions-for-the-doctor) for women at increased
risk.
14. Tobacco use screening and interventions (https://healthnder.gov/HealthTopics/Category/
health-conditions-and-diseases/diabetes/quit-smoking).
15. Urinary incontinence screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
regular-check-ups/get-your-well-woman-visit-every-year) for women yearly.
16. WeII-woman visits (https://healthnder.gov/HealthTopics/Category/everyday-healthy-living/
sexual-health/get-your-well-woman-visit-every-year) to get recommended services for women
under 65.

116
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
MORE ON PREVENTION
• Learn more about preventive care from the CDC (https://www.cdc.gov/prevention/).
• See preventive services covered for all adults (https://www.healthcare.gov/preventive-care-
adults/) and children (https://www.healthcare.gov/preventive-care-children/).
• Learn more about what else Marketplace health insurance plans cover (https://www.healthcare.
gov/coverage/what-marketplace-plans-cover/).

117
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
Preventive care benets for children
IMPORTANT
These services are free only when delivered by a doctor or other provider in your plan’s network.
Coverage for children’s preventive health services
All Marketplace health plans and many other plans must cover the following list of preventive services
for children without charging you a co-payment (/glossary/co-payment) or co-insurance (/glossary/co-
insurance). This is true even if you haven’t met your yearly deductible (/glossary/deductible).
1. Alcohol, tobacco, and drug use assessments (https://healthnder.gov/HealthTopics/Category/
parenting/healthy-communication-and-relationships/talk-to-your-kids-about-tobacco-alcohol-
and-drugs) for adolescents.
2. Autism screening (http://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/
make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4) for children at 18 and 24 months.
3. Behavioral assessments for children ages: 0 to 11 months (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-babys-visit-to-the-doctor-ages-0-
to-11-months), 1 to 4 years (http://healthnder.gov/HealthTopics/Category/parenting/doctor-
visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4), 5 to 10 years (https://
healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-
childs-visit-to-the-doctor-ages-5-to-10), 11 to 14 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-11-
to-14), 15 to 17 years (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/
make-the-most-of-your-teens-visit-to-the-doctor-ages-15-to-17).
4. Bilirubin concentration screening (https://health.gov/myhealthnder/topics/pregnancy/doctor-
and-midwife-visits/talk-your-doctor-about-newborn-screening#panel-1) for newborns.
5. Blood pressure screening for children ages: 0 to 11 months (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-babys-visit-to-the-doctor-ages-0-
to-11-months), 1 to 4 years (http://healthnder.gov/HealthTopics/Category/parenting/doctor-
visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4), 5 to 10 years (https://
healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-
childs-visit-to-the-doctor-ages-5-to-10), 11 to 14 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-11-
to-14), 15 to 17 years (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/
make-the-most-of-your-teens-visit-to-the-doctor-ages-15-to-17).
6. Blood screening (https://health.gov/myhealthnder/topics/pregnancy/doctor-and-midwife-
visits/talk-your-doctor-about-newborn-screening#panel-1) for newborns.
7. Cervical dysplasia screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/
screening-tests/get-screened-for-cervical-cancer) for sexually active females.
8. Depression screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/screening-
tests/get-your-teen-screened-for-depression) for adolescents beginning routinely at age 12.
9. Developmental screening (https://healthnder.gov/HealthTopics/Category/parenting/doctor-
visits/watch-for-signs-of-speech-or-language-delay) for children under age 3.
10. Dyslipidemia screening for all children once between 9 and 100 years and once between 17 and
21 years, and for children at higher risk of lipid disorders ages: 1 to 4 years (http://healthnder.

118
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-
to-the-doctor-ages-1-to-4), 5 to 10 years (https://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-5-to-10), 11 to
14 years (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-
most-of-your-childs-visit-to-the-doctor-ages-11-to-14), 15 to 17 years (https://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-
doctor-ages-15-to-17)
11. Fluoride chemoprevention supplements (https://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/take-care-of-your-childs-teeth) for children without uoride in their water
source.
12. Fluoride varnish (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/take-
care-of-your-childs-teeth) for all infants and children as soon as teeth are present.
13. Gonorrhea preventive medication (https://healthnder.gov/HealthTopics/Category/pregnancy/
doctor-and-midwife-visits/talk-with-your-doctor-about-newborn-screening) for the eyes of all
newborns.
14. Hearing screening (https://healthnder.gov/HealthTopics/Category/pregnancy/doctor-and-
midwife-visits/talk-with-your-doctor-about-newborn-screening) for all newborns (https://health.
gov/myhealthnder/topics/pregnancy/doctor-and-midwife-visits/talk-your-doctor-about-
newborn-screening); and for children once between 11 and 14 years (https://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-
doctor-ages-11-to-14) , once between 15 and 17 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-doctor-ages-15-
to-17), and once between 18 and 21 years.
15. Height, weight and body mass index (BMI) measurements for children ages: 0 to 11 months
(https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-
of-your-babys-visit-to-the-doctor-ages-0-to-11-months), 1 to 4 years (http://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-
doctor-ages-1-to-4), 5 to 10 years (https://healthnder.gov/HealthTopics/Category/parenting/
doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-5-to-10), 11 to 14 years
(https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-
of-your-childs-visit-to-the-doctor-ages-11-to-14), 15 to 17 years (https://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-
doctor-ages-15-to-17).
16. Hematocrit or hemoglobin screening (http://healthnder.gov/HealthTopics/Category/parenting/
doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4) for all children.
17. Hemoglobinopathies or sickle cell screening (https://healthnder.gov/HealthTopics/Category/
pregnancy/doctor-and-midwife-visits/talk-with-your-doctor-about-newborn-screening) for
newborns.
18. Hepatitis B screening (https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/
hepatitis-b-virus-infection-screening?ds=1&s=hepatitis%20b) for adolescents at high risk, including
adolescents from countries with 2% or more Hepatitis B prevalence, and U.S.-born adolescents
not vaccinated as infants and with at least one parent born in a region with 8% or more Hepatitis B
prevalence: 11 - 17 years.
19. HIV screening (https://healthnder.gov/HealthTopics/Category/health-conditions-and-
diseases/hiv-and-other-stds/get-tested-for-hiv) for adolescents at higher risk.
20. Hypothyroidism screening (https://healthnder.gov/HealthTopics/Category/pregnancy/doctor-
and-midwife-visits/talk-with-your-doctor-about-newborn-screening) for newborns.

119
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
21. Immunization vaccines (https://healthnder.gov/HealthTopics/Category/doctor-visits/
shotsvaccines/get-your-childs-shots-on-schedule) for children from birth to age 18 - doses,
recommended ages, and recommended populations vary:
• COVID-19, as described in Appendix A.
• Diphtheria (
http://www.vaccines.gov/diseases/diphtheria/index.html), Tetanus (http://www.
vaccines.gov/diseases/tetanus/index.html), Pertussis (Whooping Cough) (https://www.
vaccines.gov/diseases/pertussis/index.html).
• Haemophilus inuenza type b (
http://www.vaccines.gov/diseases/hib/index.html)
• Hepatitis A (
http://www.vaccines.gov/diseases/hepatitis_a/index.html)
• Hepatitis B (
http://www.vaccines.gov/diseases/hepatitis_b/index.html)
• Human Papillomavirus (PVU) (
http://www.vaccines.gov/diseases/hpv/index.html)
• Inactivated Poliovirus (
http://www.vaccines.gov/diseases/polio/index.html)
• Inuenza (u shot) (
http://www.vaccines.gov/diseases/u/index.html)
• Measles (
http://www.vaccines.gov/diseases/measles/index.html)
• Meningococcal (
http://www.vaccines.gov/diseases/meningitis/index.html)
• Pneumococcal (
http://www.vaccines.gov/diseases/pneumonia/index.html)
• Rotavirus (
http://www.vaccines.gov/diseases/rotavirus/index.html)
• Varicella (Chickenpox) (
http://www.vaccines.gov/diseases/chickenpox/index.html)
22. Iron supplements (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/
make-the-most-of-your-babys-visit-to-the-doctor-ages-0-to-11-months) for children ages 6 to 12
months at risk for anemia.
23. Lead screening for children at risk of exposure.
24. Maternal depression screening for mothers of infants at 1, 2, 4, and 6-month visits (https://health.
gov/myhealthnder/topics/doctor-visits/regular-checkups/make-most-your-babys-visit-
doctor-ages-0-11-months#panel-1)
25. Medical history for all children throughout development ages: 0 to 11 months (https://healthnder.
gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-babys-visit-to-
the-doctor-ages-0-to-11-months), 1 to 4 years (http://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4), 5 to
10 years (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-
the-most-of-your-childs-visit-to-the-doctor-ages-5-to-10), 11 to 14 years (https://healthnder.
gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-
the-doctor-ages-11-to-14), 15 to 17 years (https://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-doctor-ages-15-to-17).
26. Obesity screening and counseling (https://healthnder.gov/HealthTopics/Category/parenting/
nutrition-and-physical-activity/help-your-child-stay-at-a-healthy-weight).
27. Oral health risk assessment for young children ages: 0 to 11 months (https://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-babys-visit-to-the-

120
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
doctor-ages-0-to-11-months), 1 to 4 years (http://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4), 5 to 10
years (https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-
most-of-your-childs-visit-to-the-doctor-ages-5-to-10).
28. Phenylketonuria (PKU) screening (https://healthnder.gov/HealthTopics/Category/pregnancy/
doctor-and-midwife-visits/talk-with-your-doctor-about-newborn-screening) for newborns.
29. Sexually transmitted infection (STI) prevention counseling and screening (https://health.gov/
myhealthnder/topics/health-conditions/hiv-and-other-stds) for adolescents at higher risk.
30. Tuberculin testing for children at higher risk of tuberculosis ages: : 0 to 11 months (https://
healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-of-
your-babys-visit-to-the-doctor-ages-0-to-11-months), 1 to 4 years (http://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-
doctor-ages-1-to-4), 5 to 10 years (https://healthnder.gov/HealthTopics/Category/parenting/
doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-5-to-10), 11 to 14 years
(https://healthnder.gov/HealthTopics/Category/parenting/doctor-visits/make-the-most-
of-your-childs-visit-to-the-doctor-ages-11-to-14), 15 to 17 years (https://healthnder.gov/
HealthTopics/Category/parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-
doctor-ages-15-to-17).
31. Vision screening (https://healthnder.gov/HealthTopics/Category/doctor-visits/screening-
tests/get-your-childs-vision-checked) for all children.
More information about preventive services for children
• Preventive services for children age 0 to 11 months (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-babys-visit-to-the-doctor-ages-0-to-
11-months).
• Preventive services for children age 1 to 4 years (http://healthnder.gov/HealthTopics/Category/
parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-1-to-4).
• Preventive services for children age 5 to 10 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-5-
to-10).
• Preventive services for children age 11 to 14 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-childs-visit-to-the-doctor-ages-11-
to-14).
• Preventive services for children age 15 to 17 years (https://healthnder.gov/HealthTopics/
Category/parenting/doctor-visits/make-the-most-of-your-teens-visit-to-the-doctor-ages-15-
to-17).
MORE ON PREVENTION
• Learn more about preventive care from the CDC (http://www.cdc.gov/prevention/).
• See preventive services covered for adults (https://www.healthcare.gov/preventive-care-adults/)
and women (https://www.healthcare.gov/preventive-care-women/).
• Learn more about what else Marketplace health insurance plans cover (https://www.healthcare.
gov/coverage/what-marketplace-plans-cover/).

121
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
APPENDIX E – Care During the COVID-19 Pandemic
Due to the COVID-19 pandemic, the Plan is waiving member deductibles, co-payments, and co-insurance for
testing and treatment of, and vaccination for, the COVID-19 virus, and is expanding prescription drug rell/
renewal access.
These special provisions are intended to be eective until at least the end of the national emergency for
COVID-19 (although this end date and/or the provisions in this Appendix E may be modied at any time by law
and/or at the discretion of the plan administrator).
Important - Your Partnership
The availability of testing and treatments for the COVID-19 virus are constantly changing. The plan administrator,
utilization review manager, Express Scripts, the Plan’s claims processors, the Plan’s Customer Service
department, and your Human Resources department are all committed to providing service to you and we
ask for your patience during this unprecedented scenario. We anticipate we will be required to make decisions
quickly and there may be changes to normal processes.
The Plan is committed to providing benets as noted below; however, there may be unanticipated items
that come up that may require you to pay deductibles, co-payments, or co-insurance upfront, and then seek
reimbursement. We will work through these situations with you. For assistance, please call the Plan’s Customer
Service department at 888-276-4732 for medical benets, and call Express Scripts for prescription drug benets
at 800-841-5396.
Cost Sharing Waiver
The Plan will waive all member cost sharing for any COVID-19 testing (including FDA approved/ cleared/
authorized at-home testing and antibody testing) administered or referred by a licensed or authorized health
care provider (except that the Plan does not cover testing performed for general workplace health and safety,
for public health surveillance, or for other purposes not primarily intended for individualized diagnosis or
treatment of COVID-19). This cost sharing waiver for testing includes the items/services furnished during the
provider visit that resulted in an order for, or administration of, the COVID-19 test to the extent related to the
furnishing or administration of the test or to the evaluation of the member in determining the need for the test.
When the diagnosis code U07.1 is used, the Plan will waive the member deductibles, co-payments, and co-
insurance for treatment for COVID-19 for urgent care, oce visit with diagnosis, emergency room, and in-patient
hospital stays as long as such services meet the other covered service requirements under the Plan. The Plan
will also waive member cost sharing for diagnosis codes Z03.818 and Z20.828 when there has been a possible
or conrmed COVID-19 exposure. Please note there may be additional codes later adopted as set by public
health entities.
The Plan’s usual network requirements will be waived for COVID-19 testing, but not treatment.
COVID-19 vaccines that are recommended by the Advisory Committee on Immunization Practices will be
covered at no cost (regardless of whether the immunization is recommended for routine use and even if such
vaccines have not received full approval from the FDA), and such Plan coverage for a specic COVID-19 vaccine
will begin no later than 15 business days after the Director of the CDC adopts the recommendation of the
Advisory Committee on Immunization Practices for such vaccine.
To conrm benets, please call the Plan’s customer service department at 888-276-4732 for medical benets,
and call Express Scripts (the Plan’s pharmacy benet manager) for prescription drug benets at 800-841-5396.
Prescription Drug Benets
Rells or renewals of prescriptions can be made when 25% - 35% of your current supply is remaining. Members
will also be able to have one (1) override rell per 365 days at the member’s request. The Plan will also have
protocols in place for further overrides for zip codes that are specied as needing emergency access. For more
information, please contact Express Scripts at 800-841-5396.

122
ASCEND TO WHOLENESS PLANS / SUMMARY PLAN DESCRIPTION
4844-9924-9405.10
APPENDIX F – Extension of Certain Plan Deadlines During the COVID-19 Pandemic
Eective March 1, 2020, certain Plan deadlines were temporarily waived due to the COVID-19 pandemic for
one year due to a federal rule (85 Fed. Reg. 26351). In light of the continued pandemic, that rule was updated
by Disaster Relief Notice 2021-01 issued on February 26, 2021, and this newly-updated rule will continue until
60 days after the announced end of the National Emergency.
The following deadlines have been extended:
• Enrolling in the Plan in connection with a HIPAA special enrollment event, such as due to birth, marriage,
loss of other coverage, etc. (see the HIPAA Special Enrollment Rights section for a discussion of all events)
• Filing a claim for benets
• Filing an appeal with respect to a denied benet claim
• Filing a request for, and providing the information needed to obtain, an independent external review
If you would like to le a health plan claim, appeal, or request/information for external review, and your
regular Plan deadline falls on or after March 1, 2020, then your deadline for taking that action will be extended
by one year. For example, there is usually a 180-day deadline to le an appeal. If you received a claim denial
on April 1, 2020, you will have until September 28, 2021 to le your appeal. (This date is calculated by adding
the usual 180 days plus an additional one year.) However, if your newly-calculated deadline falls before March
31, 2021, the Plan will extend a grace period to you so that your new deadline will be on March 31, 2021.
For your special enrollment deadlines, if you have (or had) a special enrollment event on or after January 31,
2020 (such as a birth, adoption, marriage, loss of other coverage), you must request enrollment within 30 days
plus one year of the event (or March 30, 2021, if later, per a Plan grace period). If you or your dependent had
a loss of eligibility under Medicaid or a change in eligibility for a State Child Health Insurance Program on or
after January 1, 2020, you must request enrollment within 60 days plus one year of the change (or April 29,
2021, if later, per a Plan grace period).
If you take advantage of the extended deadline for HIPAA special enrollment, coverage will only become
eective once you pay all of your employee-share contributions that are due from the eective date of
coverage through the date of your election. Assuming these employee-share contributions are paid, then
a newborn, newly-adopted, or newly-placed for adoption dependent child (and an uncovered employee
or spouse added in connection with the birth/adoption) may be added retroactively to the date of the birth,
adoption, or placement for adoption. For all other enrollments requested after the deadlines stated in the
HIPAA Special Enrollment Rights section, the eective date of coverage will be the rst day of the month
following the late HIPAA special enrollment request.
These special rules will end 60 days after the announced end of the COVID-19 National Emergency. This
means that any tolling of a deadline pursuant to the above will end on the earlier of (i) one year from the
original Plan deadline, and (ii) 60 days after the announced end of the COVID-19 National Emergency.
You are responsible for understanding whether a deadline extension applies to your particular situation
and determining when that extension ends. Future communications may not reference these temporary
extensions. Additionally, some future standard communications may contain “boilerplate” information that
includes the usual deadlines (which are now temporarily subject to extension).
If you have questions about whether a particular deadline extension is applicable to you or your situation,
please call the Plan’s Customer Service department at 888-276-4732.
