
1
Chapter 11
Lecture Outline
Copyright © McGraw-Hill Education. Permission required for reproduction or display.
See separate PowerPoint slides for all figures and tables pre-
inserted into PowerPoint without notes.

Introduction
• Movement is a fundamental characteristic of
all living organisms
• Three types of muscular tissue—skeletal,
cardiac, and smooth muscle
• Important to understand muscle at the
molecular, cellular, and tissue levels of
organization
11-2

Types and Characteristics of
Muscular Tissue
• Expected Learning Outcomes
– Describe the physiological properties that all muscle
types have in common.
– List the defining characteristics of skeletal muscle.
– Discuss the possible elastic functions of the
connective tissue components of a muscle.
11-3

11-4
Universal Characteristics of Muscle
• Excitability (responsiveness)
– To chemical signals, stretch, and electrical changes across the
plasma membrane
• Conductivity
– Local electrical change triggers a wave of excitation that travels
along the muscle fiber
• Contractility
– Shortens when stimulated
• Extensibility
– Capable of being stretched between contractions
• Elasticity
– Returns to its original rest length after being stretched

11-5
Skeletal Muscle
• Skeletal muscle—voluntary,
striated muscle usually
attached to bones
• Striations—alternating light
and dark transverse bands
– Results from arrangement of
internal contractile proteins
• Voluntary—usually subject
to conscious control
• Muscle cell is a muscle
fiber (myofiber)—as long as
30 cm
Figure 11.1

11-6
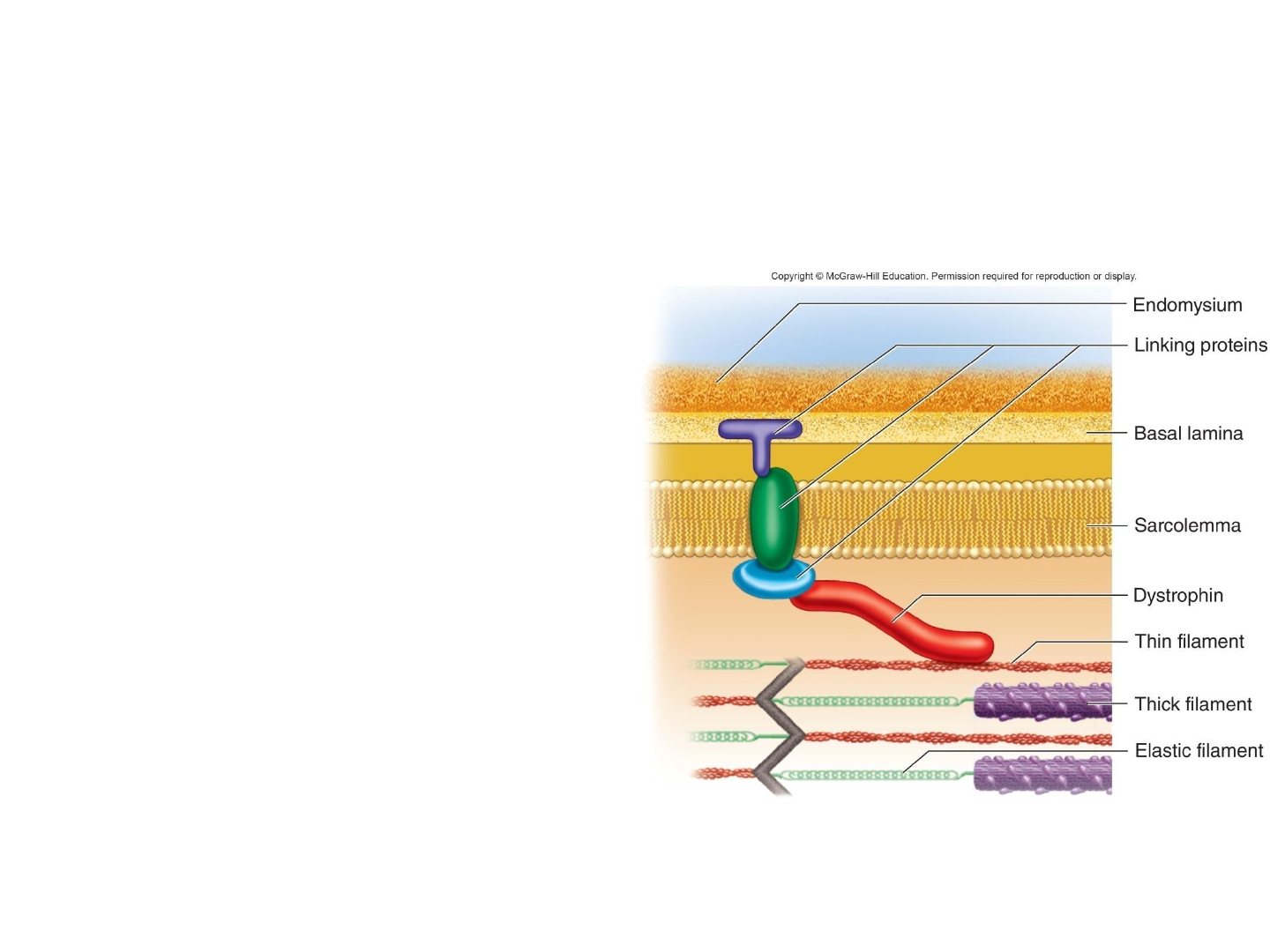
Skeletal Muscle
• Connective tissue wrappings
– Endomysium: connective tissue around muscle cell
– Perimysium: connective tissue around muscle fascicle
– Epimysium: connective tissue surrounding entire muscle
• Tendons are attachments between muscle and bone matrix
– Continuous with collagen fibers of tendons
– In turn, with connective tissue of bone matrix
• Collagen is somewhat extensible and elastic
– Stretches slightly under tension and recoils when released
• Resists excessive stretching and protects muscle from injury
• Returns muscle to its resting length
• Contributes to power output and muscle efficiency

Microscopic Anatomy of
Skeletal Muscle
• Expected Learning Outcomes
– Describe the structural components of a muscle fiber.
– Relate the striations of a muscle fiber to the
overlapping arrangement of its protein filaments.
– Name the major proteins of a muscle fiber and state
the function of each.
11-7

11-8
The Muscle Fiber
• Sarcolemma—plasma membrane of a muscle
fiber
• Sarcoplasm—cytoplasm of a muscle fiber
– Myofibrils: long protein cords occupying most of
sarcoplasm
– Glycogen: carbohydrate stored to provide energy for
exercise
– Myoglobin: red pigment; provides some oxygen
needed for muscle activity

• Multiple nuclei—flattened nuclei pressed against
the inside of the sarcolemma
– Myoblasts: stem cells that fused to form each muscle
fiber early in development
– Satellite cells: unspecialized myoblasts remaining
between the muscle fiber and endomysium
• Play a role in regeneration of damaged skeletal muscle
tissue
• Mitochondria—packed into spaces between
myofibrils
11-9
The Muscle Fiber

11-10
• Sarcoplasmic reticulum (SR)—smooth ER
that forms a network around each myofibril:
– Terminal cisternae—dilated end-sacs of SR which
cross the muscle fiber from one side to the other
– Acts as a calcium reservoir; it releases calcium
through channels to activate contraction
• T tubules—tubular infoldings of the
sarcolemma which penetrate through the cell
and emerge on the other side
• Triad—a T tubule and two terminal cisternae
associated with it
The Muscle Fiber

Sarcoplasm
Sarcolemma
Openings into
transverse tubules
Sarcoplasmic
reticulum
Mitochondria
Myofibrils
Myofilaments
A band
I band
Z disc
Nucleus
Triad:
Terminal cisternae
Transverse tubule
Muscle
fiber
11-11
Figure 11.2
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
The Muscle Fiber

11-12
Myofilaments
• Thick filaments—made of several hundred myosin molecules
– Each molecule shaped like a golf club
• Two chains intertwined to form a shaft-like tail
• Double globular head
– Heads directed outward in a helical array around the bundle
• Heads on one half of the thick filament angle to the left, while heads
on other half angle to the right
• Bare zone with no heads in the middle
Figure 11.3a, b, d
(a) Myosin molecule
Head
Tail
(b) Thick filament
Myosin head
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-13
Myofilaments
• Thin filaments
– Fibrous (F) actin: two intertwined strands
• String of globular (G) actin subunits each with an active site
that can bind to head of myosin molecule
– Tropomyosin molecules
• Each blocking six or seven active sites on G actin subunits
– Troponin molecule: small, calcium-binding protein on
each tropomyosin molecule
(c) Thin filament
Troponin complex G actinTropomyosin
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Figure 11.3c

11-14
Myofilaments
• Elastic filaments
– Titin: huge, springy protein
– Run through core of thin filament and anchor it to Z
disc and M line
– Help stabilize and position the thick filament
– Prevent overstretching and provide recoil
Figure 11.5

11-15
Myofilaments
• Contractile proteins—myosin and actin do the work of contraction
• Regulatory proteins—tropomyosin and troponin
– Act like a switch that determines when fiber can (and cannot) contract
– Contraction activated by release of calcium into sarcoplasm and its
binding to troponin
– Troponin changes shape and moves tropomyosin off the active sites on
actin
(b) Thick filament
Myosin head
(c) Thin filament
Troponin complex G actinTropomyosin
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Figure 11.3b,c

11-16
Myofilaments
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
(d) Portion of a sarcomere showing the overlap
of thick and thin filaments
Bare zone
Thin filament
Thick filament
Figure 11.3d
11-17
Myofilaments
• Several other proteins
associate with myofilaments
to anchor, align, and regulate
them
• Dystrophin—clinically
important protein
– Links actin in outermost
myofilaments to membrane
proteins that link to endomysium
– Transfers forces of muscle
contraction to connective tissue
ultimately leading to tendon
– Genetic defects in dystrophin
produce disabling disease
muscular dystrophy

11-18
Striations
• Striations result from the precise organization of myosin
and actin in cardiac and skeletal muscle cells
• Striations are alternating A-bands (dark) and I-bands (light)
Figure 11.5b

11-19
Striations
– A band: dark; “A” stands for anisotropic
• Darkest part is where thick filaments overlap a hexagonal array of
thin filaments
• H band: not as dark; middle of A band; thick filaments only
• M line: middle of H band
– I band: light; “I” stands for isotropic
• The way the bands reflect polarized light
• Z disc: provides anchorage for thin filaments and elastic filaments
• Bisects I band
Figure 11.5b

Striations
11-20
Figure 11.5a

11-21
Striations
• Sarcomere—segment from Z disc to Z disc
– Functional contractile unit of muscle fiber
• Muscle cells shorten because their individual
sarcomeres shorten
– Z disc (Z lines) are pulled closer together as thick and thin
filaments slide past each other
• Neither thick nor thin filaments change length
during shortening
– Only the amount of overlap changes
• During shortening, dystrophin and linking proteins
also pull on extracellular proteins
– Transfers pull to extracellular tissue

11-22
Structural Hierarchy of Skeletal Muscle

11-23
Structural Hierarchy of Skeletal Muscle

The Nerve—Muscle Relationship
• Expected Learning Outcomes
– Explain what a motor unit is and how it relates to
muscle contraction.
– Describe the structure of the junction where a nerve
fiber meets a muscle fiber.
– Explain why a cell has an electrical charge difference
across its plasma membrane and, in general terms,
how this relates to muscle contraction.
11-24

11-25
The Nerve—Muscle Relationship
• Skeletal muscle never contracts unless
stimulated by a nerve
• If nerve connections are severed or
poisoned, a muscle is paralyzed
– Denervation atrophy: shrinkage of
paralyzed muscle when nerve remains
disconnected

Motor Neurons and Motor Units
• Somatic motor neurons
– Nerve cells whose cell bodies are in the brainstem
and spinal cord that serve skeletal muscles
– Somatic motor fibers—their axons that lead to the
skeletal muscle
– Each nerve fiber branches out to a number of muscle
fibers
– Each muscle fiber is supplied by only one motor
neuron
11-26

11-27
Motor Neurons and Motor Units
• Motor unit—one nerve fiber
and all the muscle fibers
innervated by it
• Muscle fibers of one motor
unit
– Dispersed throughout muscle
– Contract in unison
– Produce weak contraction
over wide area
– Provide ability to sustain long-
term contraction as motor
units take turns contracting
– Effective contraction usually
requires contraction of
several motor units at once
Figure 11.6
Spinal cord
Neuromuscular
junction
Skeletal
muscle
fibers
Motor
neuron 1
Motor
neuron 2
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

Motor Neurons and Motor Units
• Average motor unit contains 200 muscle
fibers
• Small motor units—fine degree of control
– Three to six muscle fibers per neuron
– Eye and hand muscles
• Large motor units—more strength than control
– Powerful contractions supplied by large motor units
with hundreds of fibers
– Gastrocnemius of calf has 1,000 muscle fibers per
neuron
11-28

11-29
The Neuromuscular Junction
• Synapse—point where a nerve fiber meets its
target cell
• Neuromuscular junction (NMJ)—when target cell
is a muscle fiber
• Each terminal branch of the nerve fiber within
the NMJ forms separate synapse with the
muscle fiber
• One nerve fiber stimulates the muscle fiber at
several points within the NMJ

11-30
The Neuromuscular Junction
• Synaptic knob—swollen end of nerve fiber
– Contains synaptic vesicles with acetylcholine (ACh)
• Synaptic cleft—gap between synaptic knob and sarcolemma
• Schwann cell envelops and isolates NMJ
Figure 11.7b

11-31
The Neuromuscular Junction
• Nerve impulse causes synaptic vesicles to undergo
exocytosis releasing ACh into synaptic cleft
• Muscle cell has millions of ACh receptors—
proteins incorporated into its membrane
– Junctional folds of sarcolemma beneath synaptic knob
increase surface area holding ACh receptors
• Lack of receptors causes weakness in myasthenia gravis
• Basal lamina—thin layer of collagen and
glycoprotein separating Schwann cell and muscle
cell from surrounding tissues
– Contains acetylcholinesterase (AChE) that breaks
down Ach, allowing for relaxation

11-32
The Neuromuscular Junction
Figure 11.7a

11-33
Electrically Excitable Cells
• Muscle fibers and neurons are electrically
excitable
– Their membranes exhibit voltage changes in response to
stimulation
• Electrophysiology—the study of the electrical
activity of cells
• Voltage (electrical potential)—a difference in
electrical charge from one point to another
• Resting membrane potential—about −90 mV in
skeletal muscle cells
– Maintained by sodium–potassium pump

Electrically Excitable Cells
• In an unstimulated (resting) cell
– There are more anions (negatively charged particles) on the
inside of the membrane than on the outside
– These anions make the inside of the plasma membrane
negatively charged by comparison to its outer surface
– The plasma membrane is electrically polarized (charged)
with a negative resting membrane potential (RMP)
– There are excess sodium ions (Na
+
) in the extracellular
fluid (ECF)
– There are excess potassium ions (K
+
) in the intracellular
fluid (ICF)
11-34

11-35
Electrically Excitable Cells
• Stimulated (active) muscle fiber or nerve cell
– Na
+
ion gates open in the plasma membrane
– Na
+
flows into cell down its electrochemical gradient
– These cations override the negative charges in the ICF
– Depolarization: inside of plasma membrane becomes positive
– Immediately, Na
+
gates close and K
+
gates open
– K
+
rushes out of cell partly repelled by positive sodium
charge and partly because of its concentration gradient
– Loss of positive potassium ions turns the membrane negative
again (repolarization)
– This quick up-and-down voltage shift (depolarization and
repolarization) is called an action potential

11-36
Electrically Excitable Cells
• Resting membrane potential (RMP) is seen in a
waiting excitable cell, whereas action potential is a
quick event seen in a stimulated excitable cell
• An action potential perpetuates itself down the
length of a cell’s membrane
– An action potential at one point causes another one to
happen immediately in front of it, which triggers another
one a little farther along and so forth
– This wave of excitation is called an impulse

11-37
Neuromuscular Toxins and Paralysis
• Toxins interfering with synaptic function can paralyze
muscles
• Some pesticides contain cholinesterase inhibitors
– Bind to acetylcholinesterase and prevent it from degrading Ach
– Spastic paralysis: a state of continual contraction of the
muscles; possible suffocation
• Tetanus (lockjaw) is a form of spastic paralysis caused by
toxin Clostridium tetani
– Glycine in the spinal cord normally stops motor neurons from
producing unwanted muscle contractions
– Tetanus toxin blocks glycine release in the spinal cord and
causes overstimulation and spastic paralysis of the muscles

11-38
Neuromuscular Toxins and Paralysis
• Flaccid paralysis—a state in which the muscles are limp
and cannot contract
– Curare: competes with ACh for receptor sites, but does not
stimulate the muscles
– Plant poison used by South American natives to poison
blowgun darts
• Botulism—type of food poisoning caused by a
neuromuscular toxin secreted by the bacterium Clostridium
botulinum
– Blocks release of ACh causing flaccid paralysis
– Botox cosmetic injections used for wrinkle removal

Behavior of Skeletal Muscle Fibers
• Expected Learning Outcomes
– Explain how a nerve fiber stimulates a skeletal
muscle fiber.
– Explain how stimulation of a muscle fiber activates its
contractile mechanism.
– Explain the mechanism of muscle contraction.
– Explain how a muscle fiber relaxes.
– Explain why the force of a muscle contraction
depends on sarcomere length prior to stimulation.
11-39

11-40
Behavior of Skeletal Muscle Fibers
• Four major phases of contraction and relaxation
– Excitation
• Process in which nerve action potentials lead to muscle action
potentials
– Excitation–contraction coupling
• Events that link the action potentials on the sarcolemma to
activation of the myofilaments, thereby preparing them to contract
– Contraction
• Step in which the muscle fiber develops tension and may shorten
– Relaxation
• When stimulation ends, a muscle fiber relaxes and returns to its
resting length

11-41
Excitation
• Nerve signal opens voltage-gated calcium channels in synaptic knob
• Calcium enters knob and stimulates release of ACh from synaptic
vesicles into synaptic cleft
• Ach diffuses across cleft
Figure 11.8 (1, 2)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Arrival of nerve signal
1
Acetylcholine (ACh) release2
Motor
nerve
fiber
Sarcolemma
Synaptic
knob
Synaptic
vesicles
ACh
receptors
Nerve signal
ACh
Ca
2+
enters
synaptic knob
Synaptic
cleft

11-42
Excitation
• Two ACh molecules bind to each receptor and open its channel
• Na
+
enters; shifting membrane potential from −90 mV to +75 mV
• Then K
+
exits and potential returns to −90 mV
• The quick voltage shift is called an end-plate potential (EPP)
Figure 11.8 (3, 4)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Binding of ACh to receptor
3
Sarcolemma
ACh receptor
AChACh
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Opening of ligand-regulated ion gate;
creation of end-plate potential
4
K
+
Na
+

11-43
Excitation
• Voltage change in end-plate region (EPP) opens nearby voltage-
gated channels producing an action potential that spreads over
muscle surface
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Opening of voltage-regulated ion gates;
creation of action potentials
5
K
+
Na
+
Sarcolemma
Plasma
membrane
of synaptic
knob
Voltage-regulated
ion gates
Figure 11.8 (5)

11-44
Excitation–Contraction Coupling
• Action potential spreads down T tubules
• Opens voltage-gated ion channels in T tubules and Ca
+2
channels in SR
• Ca
+2
leaves SR and enters cytosol
Action potentials propagated
down T tubules
6
Calcium released from
terminal cisternae
7
Ca
2+
T tubule
T tubule
Terminal
cisterna
of SR
Sarcoplasmic
reticulum
Ca
2+
Figure 11.9 (6, 7)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-45
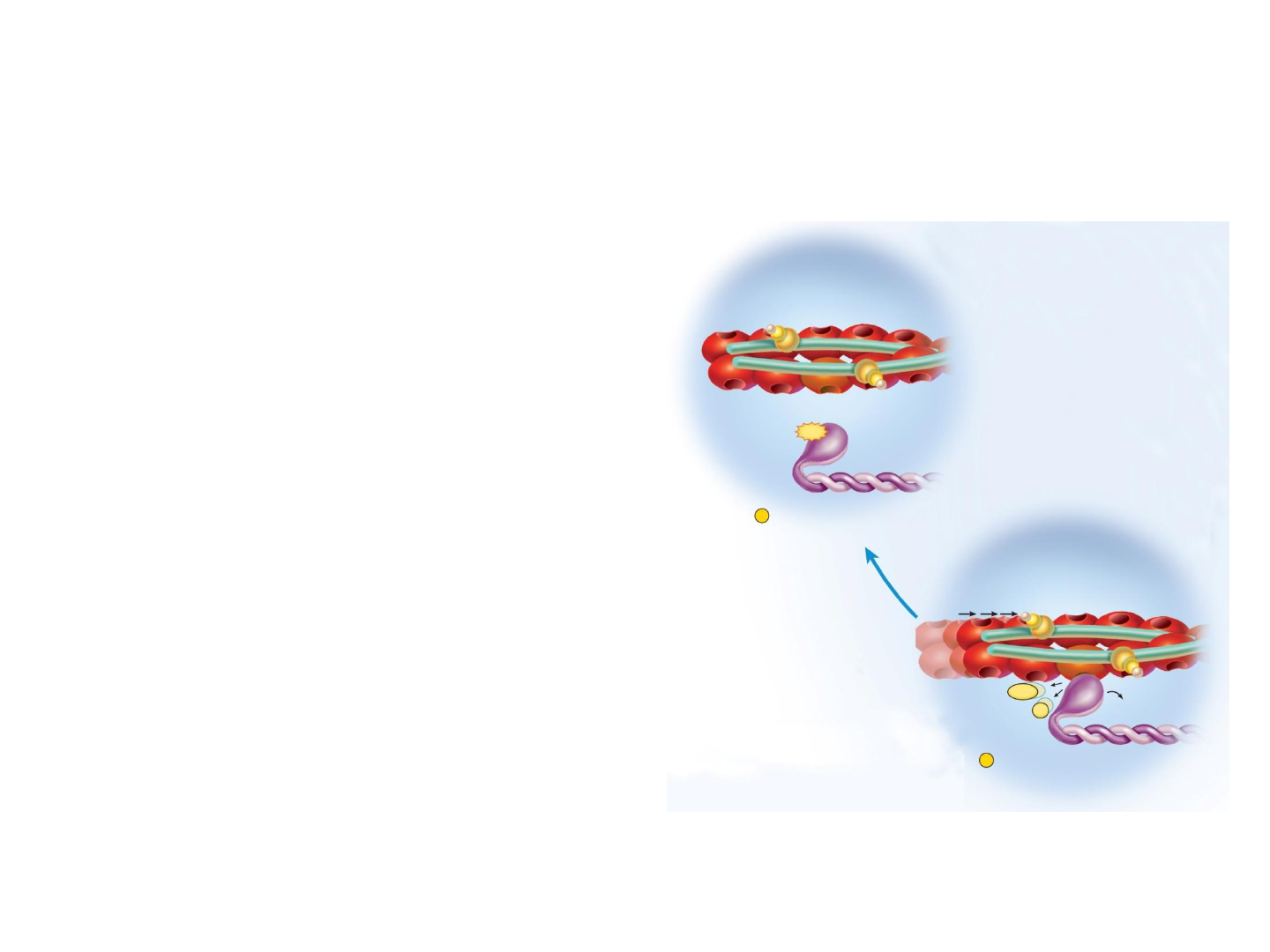
• Calcium binds to troponin in thin filaments
• Troponin–tropomyosin complex changes shape and exposes active sites
on actin
Figure 11.9 (8, 9)
8
Shifting of tropomyosin;
exposure of active sites
on actin
9
Active sites
Myosin
Ca
2+
Ca
2+
Troponin
Tropomyosin Actin Thin filament
Binding of calcium
to troponin
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Excitation–Contraction Coupling

11-46
Contraction
• ATPase in myosin
head hydrolyzes an
ATP molecule
• Activates the head
“cocking” it in an
extended position
– ADP + P
i
remain
attached
• Head binds to actin
active site forming
a myosin–actin
cross-bridge
Figure 11.10 (10, 11)
11-47
Contraction
• Myosin releases
ADP and P
i
, and flexes pulling
thin filament with it—power
stroke
• Upon binding more ATP,
myosin releases actin
and process can be repeated
– Recovery stroke recocks
head
• Each head performs five power
strokes per second
– Each stroke utilizes one
molecule of ATP
Power stroke; sliding of thin
filament over thick filament
12
Binding of new ATP;
breaking of cross-bridge
13
ATP
P
i
ADP
P
i
ADP
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Figure 11.10 (12, 13)

11-48
Relaxation
• Nerve stimulation and ACh release stop
• AChE breaks down ACh and fragments are reabsorbed into knob
• Stimulation by ACh stops
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
AChE
Cessation of nervous stimulation
and ACh release
14
ACh breakdown by
acetylcholinesterase (AChE)
15
ACh
Figure 11.11 (14, 15)

11-49
Relaxation
• Ca
+2
pumped back into SR by active transport
• Ca
+2
binds to calsequestrin while in storage in SR
Figure 11.11 (16)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Ca
2+
Ca
2+
Reabsorption of calcium ions by
sarcoplasmic reticulum
16
Terminal cisterna
of SR

11-50
Relaxation
• Ca
+2
removed from troponin
is pumped back into SR
• Tropomyosin reblocks the
active sites of actin
• Muscle fiber ceases to
produce or maintain tension
• Muscle fiber returns to its
resting length
– Due to recoil of elastic
components and contraction
of antagonistic muscles
Figure 11.11 (17, 18)
Ca
2+
Ca
2+
Loss of calcium ions from troponin
17
ADP
P
i
Return of tropomyosin to position
blocking active sites of actin
18
Tropomyosin
ATP
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-51
The Length–Tension Relationship
and Muscle Tone
• Length–tension relationship—the amount of tension
generated by a muscle depends on how stretched or
shortened it was before it was stimulated
– If overly shortened before stimulated, a weak contraction
results, as thick filaments just butt against Z discs
– If too stretched before stimulated, a weak contraction results,
as minimal overlap between thick and thin filaments results in
minimal cross-bridge formation
– Optimum resting length produces greatest force when
muscle contracts
• The nervous system maintains muscle tone (partial contraction) to
ensure that resting muscles are near this length

11-52
Length–Tension Relationship
Figure 11.12

11-53
Rigor Mortis
• Rigor mortis—hardening of muscles and stiffening of
body beginning 3 to 4 hours after death
– Deteriorating sarcoplasmic reticulum releases Ca
+2
– Deteriorating sarcolemma allows Ca
+2
to enter cytosol
– Ca
+2
activates myosin-actin cross-bridging
– Muscle contracts, but cannot relax
• Muscle relaxation requires ATP, and ATP production
is no longer produced after death
– Fibers remain contracted until myofilaments begin to decay
• Rigor mortis peaks about 12 hours after death, then
diminishes over the next 48 to 60 hours

Behavior of Whole Muscles
• Expected Learning Outcomes
– Describe the stages of a muscle twitch.
– Explain how successive muscle twitches can add up
to produce stronger muscle contractions.
– Distinguish between isometric and isotonic
contraction.
– Distinguish between concentric and eccentric
contraction.
11-54

11-55
Threshold, Latent Period, and Twitch
• Myogram—a chart of the
timing and strength of a
muscle’s contraction
• Threshold—minimum voltage
necessary to generate an
action potential in the muscle
fiber and produce a contraction
• Twitch—a quick cycle of
contraction and relaxation
when stimulus is at threshold
or higher
Figure 11.13
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or
display.
Contraction
phase
Relaxation
phase
Time
Latent
period
Time of
stimulation
Muscle tension

11-56
Threshold, Latent Period, and Twitch
Figure 11.13
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or
display.
Contraction
phase
Relaxation
phase
Time
Latent
period
Time of
stimulation
Muscle tension
• Latent period—very brief delay
between stimulus and contraction
– Time required for excitation,
excitation–contraction coupling, and
tensing of elastic components of
muscle (generating internal tension)
• Contraction phase—time when
muscle generates external tension
– Force generated can overcome the
load and cause movement
• Relaxation phase—time when
tension declines to baseline
– SR reabsorbs Ca
2+
, myosin releases
actin and tension decreases
– Takes longer than contraction
• Entire twitch duration varies
between 7 and 100 ms

11-57
Contraction Strength of Twitches
• With subthreshold stimuli—no contraction at all
• At threshold intensity and above—twitch produced
• Even if the same voltage is delivered, different
stimuli cause twitches varying in strength,
because:
– The muscle’s starting length influences tension generation
– Muscles fatigue after continual use
– Warmer muscles’ enzymes work more quickly
– Muscle cell’s hydration level influences cross-bridge
formation
– Increasing the frequency of stimulus delivery increases
tension output

11-58
Contraction Strength of Twitches
• Muscles must contract with variable
strength for different tasks
• Stimulating the nerve with higher
voltages produces stronger
contractions
– Higher voltages excite more nerve fibers
which stimulate more motor units to
contract
– Recruitment or multiple motor unit
(MMU) summation—the process of
bringing more motor units into play with
stronger stimuli
– Occurs according to the size principle:
weak stimuli (low voltage) recruit small
units, while strong stimuli recruit small
and large units for powerful movements
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
1 2 3 4 5 6 7 8 9
1 2 3 4 5 6 7 8 9
Threshold
Stimulus voltage
Stimuli to nerve
Tension
Proportion of nerve fibers excited
Responses of muscle
Maximum contraction
Figure 11.14

11-59
Contraction Strength of Twitches
• Low frequency stimuli produce identical twitches
• Higher frequency stimuli (eg., 20 stimuli/s) produce temporal (wave)
summation
– Each new twitch rides on the previous one generating higher tension
– Only partial relaxation between stimuli resulting in fluttering,
incomplete tetanus
• Unnaturally high stimulus frequencies (in lab experiments) cause a
steady, contraction called complete (fused) tetanus

11-60
• Isometric muscle contraction
– Muscle produces internal tension but external resistance
causes it to stay the same length
– Can be a prelude to movement when tension is absorbed by
elastic component of muscle
– Important in postural muscle function and antagonistic muscle
joint stabilization
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Muscle develops
tension but does
not shorten
No movement
(a) Isometric contraction
Isometric and Isotonic Contraction
Figure 11.16a

Isometric and Isotonic Contraction
• Isotonic muscle contraction
– Muscle changes in length with no change in tension
– Concentric contraction: muscle shortens as it maintains
tension (example: lifting weight)
– Eccentric contraction: muscle lengthens as it maintains
tension (example: slowly lowering weight)
11-61
Figure 11.16b, c

11-62
Isometric and Isotonic Contraction
• At the beginning of contraction—isometric phase
– Muscle tension rises but muscle does not shorten
• When tension overcomes resistance of the load
– Tension levels off
• Muscle begins to shorten and move the load—isotonic phase
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Muscle
tension
Muscle
length
Isometric
phase
Isotonic
phase
Time
Length or Tension
Figure 11.17

Muscle Metabolism
• Expected Learning Outcomes
– Explain how skeletal muscle meets its energy
demands during rest and exercise.
– Explain the basis of muscle fatigue and soreness.
– Define oxygen debt and explain why extra oxygen is
needed even after an exercise has ended.
– Distinguish between two physiological types of
muscle fibers, and explain their functional roles.
– Discuss the factors that affect muscular strength.
– Discuss the effects of resistance and endurance
exercises on muscles.
11-63

11-64
ATP Sources
• All muscle contraction depends on ATP
• ATP supply depends on availability of:
– Oxygen and organic energy sources (e.g., glucose and
fatty acids)
• Two main pathways of ATP synthesis
– Anaerobic fermentation
• Enables cells to produce ATP in the absence of oxygen
• Yields little ATP and lactic acid, possibly contributing to muscle
fatigue
– Aerobic respiration
• Produces far more ATP
• Does not generate lactic acid
• Requires a continual supply of oxygen

11-65
ATP Sources
Figure 11.18
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Aerobic respiration
using oxygen from
myoglobin
Glycogen–
lactic acid
system
(anaerobic
fermentation)
Phosphagen
system
Duration of exercise
0 10 seconds 40 seconds
Aerobic
respiration
supported by
cardiopulmonary
function
Repayment of
oxygen debt
Mode of ATP synthesis

11-66
Immediate Energy
• Short, intense exercise (100 m dash)
– Oxygen is briefly supplied by myoglobin but is rapidly depleted
– Muscles meet most ATP demand by borrowing phosphate
groups (P
i
) from other molecules and transferring them to ADP
– Two enzyme systems control these phosphate transfers
• Myokinase: transfers P
i
from one ADP to another, converting the
latter to ATP
• Creatine kinase: obtains P
i
from a phosphate-storage molecule
creatine phosphate (CP) and gives it to ADP
– Phosphagen system—the combination of ATP and CP which
provides nearly all energy for short bursts of activity
• Enough energy for 6 seconds of sprinting

11-67
Creatine
phosphate
Creatine
Creatine
kinase
Myokinase
P
i
ATP
ATP
ADP ADP
ADP
AMP
P
i
Figure 11.19
Immediate Energy
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-68
Short-Term Energy
• As the phosphagen system is exhausted, muscles
shift to anaerobic fermentation
– Muscles obtain glucose from blood and their own stored
glycogen
– In the absence of oxygen, glycolysis can generate a net
gain of 2 ATP for every glucose molecule consumed
– Converts glucose to lactic acid
• Glycogen–lactic acid system—the pathway from
glycogen to lactic acid
• Produces enough ATP for 30 to 40 seconds of
maximum activity

11-69
Long-Term Energy
• After about 40 seconds, the respiratory and
cardiovascular systems start to deliver oxygen fast
enough for aerobic respiration to meet most of muscle’s
ATP demand
• Aerobic respiration produces more ATP per glucose
than glycolysis does (another 30 ATP per glucose)
– Efficient means of meeting the ATP demands of prolonged exercise
– After 3-4 minutes, the rate of oxygen consumption levels off to a
steady state where aerobic ATP production keeps pace with demand
– For 30 minutes energy comes equally from glucose and fatty acids
– Beyond 30 minutes, depletion of glucose causes fatty acids to
become the more significant fuel

11-70
Fatigue and Endurance
• Muscle fatigue—progressive weakness from prolonged use
of muscles
• Fatigue in high-intensity exercise is thought to result from:
– Potassium accumulation in the T tubules reduces excitability
– Excess ADP and P
i
slow cross-bridge movements, inhibit calcium
release and decrease force production in myofibrils
– (Possibly a drop in pH, but lactic acid does not seem to accumulate
in the muscle cell)
• Fatigue in low-intensity (long duration) exercise is thought
to result from:
– Fuel depletion as glycogen and glucose levels decline
– Electrolyte loss through sweat can decrease muscle excitability
– Central fatigue when less motor signals are issued from brain
• Brain cells inhibited by exercising muscles’ release of ammonia
• Psychological will to persevere—not well understood

11-71
Fatigue and Endurance
• Maximum oxygen uptake (VO
2
max) is major
determinant of one’s ability to maintain high-intensity
exercise for more than 4 to 5 minutes
– VO
2
max: the point at which the rate of oxygen
consumption plateaus and does not increase further with
added workload
• Proportional to body size
• Peaks at around age 20
• Usually greater in males than females
• Can be twice as great in trained endurance athlete as in
untrained person

11-72
Excess Postexercise Oxygen
Consumption (EPOC)
• EPOC meets a metabolic demand also known as
oxygen debt
• It is the difference between the elevated rate of
oxygen consumption following exercise and the
usual resting rate
• Needed for the following purposes:
– To aerobically replenish ATP (some of which helps
regenerate CP stores)
– To replace oxygen reserves on myoglobin
– To provide oxygen to liver that is busy disposing of lactic acid
– To provide oxygen to many cells that have elevated
metabolic rates after exercise
• EPOC can be six times basal consumption and last an
hour

11-73
Physiological Classes of
Muscle Fibers

11-74
Physiological Classes of
Muscle Fibers
• Fast versus slow-twitch fibers can predominate in
certain muscle groups
– Muscles of the back contract relatively quickly (100 ms to peak
tension) whereas muscles that move the eyes contract quickly (8
ms to peak tension)
• Slow-twitch, slow oxidative (SO), red or type I fibers
– Well adapted for endurance; resist fatigue by oxidative (aerobic)
ATP production
– Important for muscles that maintain posture (e.g., erector spinae
of the back, soleus of calf)
– Abundant mitochondria, capillaries, myoglobin: deep red color
– Contain a form of myosin with slow ATPase, and a SR that
releases calcium slowly
– Relatively thin fibers
– Grouped in small motor units controlled by small, easily excited
motor neurons allowing for precise movements

11-75
Physiological Classes of
Muscle Fibers
• Fast-twitch, fast glycolytic (FG), white, or type IIb fibers
– Fibers are well adapted for quick responses
– Important for quick and powerful muscles: eye and hand
muscles, gastrocnemius of calf and biceps brachii
– Contain a form of myosin with fast ATPase and a large SR that
releases calcium quickly
– Utilize glycolysis and anaerobic fermentation for energy
• Abundant glycogen and creatine phosphate
• Lack of myoglobin gives them pale (white) appearance
– Fibers are thick and strong
– Grouped in large motor units controlled by larger, less excitable
neurons allowing for powerful movements

11-76
Physiological Classes of
Muscle Fibers
• Every muscle contains a mix of fiber types, but one
type predominates depending on muscle function
• Fiber type within a muscle differs across individuals
– Some individuals seem genetically predisposed to be
sprinters, while others more suited for endurance

Physiological Classes of
Muscle Fibers
• Staining for enzymes
(oxidative versus
glycolytic) reveals the
distribution of fiber
types within one
muscle
11-77
Figure 11.20

11-78
Muscular Strength and Conditioning
• Muscles can generate more tension than the bones
and tendons can withstand
• Muscular strength depends on:
– Primarily muscle size
• Thicker muscle forms more cross-bridges
• A muscle can exert a tension of 3 or 4 kg/cm
2
of cross-
sectional area
– Fascicle arrangement
• Pennate are stronger than parallel, and parallel stronger
than circular
– Size of active motor units
• The larger the motor unit, the stronger the contraction
– Multiple motor unit summation
• Simultaneous activation of more units increases tension

11-79
Muscular Strength and Conditioning
(continued)
• Muscular strength depends on:
– Temporal summation
• The greater the frequency of stimulation, the more strongly
a muscle contracts
– Length–tension relationship
• A muscle resting at optimal length is prepared to contract
more forcefully than a muscle that is excessively contracted
or stretched
– Fatigue
• Fatigued muscles contract more weakly than rested
muscles

11-80
Muscular Strength and Conditioning
• Resistance training (example: weightlifting)
– Contraction of a muscle against a load that resists
movement
– A few minutes of resistance exercise a few times a
week is enough to stimulate muscle growth
– Growth is from cellular enlargement
– Muscle fibers synthesize more myofilaments and
myofibrils and grow thicker

11-81
Muscular Strength and Conditioning
• Endurance training (aerobic exercise)
– Improves fatigue-resistant muscles
– Slow twitch fibers produce more mitochondria,
glycogen, and acquire a greater density of blood
capillaries
– Improves skeletal strength
– Increases the red blood cell count and oxygen
transport capacity of the blood
– Enhances the function of the cardiovascular,
respiratory, and nervous systems

Cardiac and Smooth Muscle
• Expected Learning Outcomes
– Describe the structural and physiological differences
between cardiac muscle and skeletal muscle.
– Explain why these differences are important to
cardiac function.
– Describe the structural and physiological differences
between smooth muscle and skeletal muscle.
– Relate the unique properties of smooth muscle to its
locations and functions.
11-82

Cardiac and Smooth Muscle
• Cardiac and smooth muscle share certain
properties
– Their cells are myocytes—not as long and
fibrous as skeletal muscles; they have one
nucleus
– They are involuntary
– They receive innervation from the autonomic
nervous system (not from somatic motor neurons)
11-83

11-84
Cardiac Muscle
• Properties of cardiac muscle
– Contracts with regular rhythm
– Works in sleep or wakefulness, without fail, and
without conscious attention
– Highly resistant to fatigue
– Muscle cells of a given chamber must contract in
unison
– Contractions must last long enough to expel blood

11-85
Cardiac Muscle
• Characteristics of cardiac muscle cells
– Striated like skeletal muscle, but myocytes (cardiocytes)
are shorter and thicker
• Sarcoplasmic reticulum less developed, but T tubules are larger
and admit Ca
2+
from the extracellular fluid
– Myocyte is joined at its ends to other myocytes by
intercalated discs
• Appear as thick, dark lines in stained tissue sections
• Electrical gap junctions allow each myocyte to directly stimulate
its neighbors
• Mechanical junctions that keep the myocytes from pulling apart
– Damaged cardiac muscle cells repair by fibrosis
• Unfortunately, after a heart attack, functional muscle is not
regenerated

11-86
Cardiac Muscle
• Can contract without need for nervous
stimulation
– Contains a built-in pacemaker that rhythmically sets
off a wave of electrical excitation
– Wave travels through the muscle and triggers
contraction of heart chambers
– Autorhythmic: able to contract rhythmically and
independently

11-87
Cardiac Muscle
• Autonomic nervous system can increase or decrease
heart rate and contraction strength
• Very slow twitches; does not exhibit quick twitches
like skeletal muscle
- Maintains tension for about 200 to 250 ms
- Gives the heart time to expel blood
• Uses aerobic respiration almost exclusively
- Rich in myoglobin and glycogen
- Has especially large mitochondria
• 25% of volume of cardiac muscle cell
• 2% of skeletal muscle cell with smaller mitochondria
- Highly resistant to fatigue

11-88
Smooth Muscle
• Smooth muscle is named for its lack of
striations
• Some smooth muscles lack nerve supply; others
receive input from autonomic fibers with many
varicosities containing synaptic vesicles
• Capable of mitosis and hyperplasia
• Injured smooth muscle regenerates well
• Smooth muscle is slower than skeletal and
cardiac muscle
– Takes longer to contract but can remain contracted for
a long time without fatigue

11-89
Smooth Muscle
• Smooth muscle forms layers within walls of
hollow organs
– It can propel contents of an organ (e.g., food in GI tract)
– It can modify pressure and flow of blood in the
circulatory system and air in the respiratory system
• Can provide fine control in some locations
– Smooth muscle of iris controls pupil size
– Piloerector muscles raise hairs in skin

11-90
Smooth Muscle Myocyte Structure
• Myocytes have a fusiform shape
– There is one nucleus, located near the middle of the cell
– Thick and thin filaments are present, but not aligned with
each other (“smooth” not striated)
• Sarcoplasmic reticulum is scanty and there are no T
tubules
• Ca
2+
needed for muscle contraction comes from
ECF by way of Ca
2+
channels in sarcolemma
• Z discs are absent and replaced by dense bodies
– Well-ordered array of protein masses that form protein
plaques on the inner face of the plasma membrane and
scattered throughout sarcoplasm
– Dense bodies of neighboring cells are linked together

11-91
Types of Smooth Muscle
• Multiunit smooth muscle
– Occurs in some of the largest
arteries and air passages, in
piloerector muscles, and in
iris of the eye
– Autonomic innervation forms
motor units
• Terminal branches of a nerve
fiber synapse with individual
myocytes
• Each motor unit contracts
independently of the others
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Synapses
Autonomic
nerve fibers
(a) Multiunit
smooth muscle
Figure 11.23a

11-92
Types of Smooth Muscle
• Single-unit smooth muscle
– More common
– Occurs in most blood
vessels, in digestive,
respiratory, urinary, and
reproductive tracts
– Also called visceral muscle
• Often in two layers: inner
circular and outer
longitudinal
– Myocytes of this cell type are
electrically coupled to each
other by gap junctions
– They directly stimulate each
other and a large number of
cells contract as one
Figure 11.23b
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Varicosities
Gap junctions
Autonomic
nerve fibers
(b) Single-unit
smooth muscle

11-93
Types of Smooth Muscle
Figure 11.21
Synaptic
vesicle
Mitochondrion
Autonomic
nerve fiber
Varicosities
Single-unit
smooth muscle
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-94
Types of Smooth Muscle
Epithelium
Mucosa:
Muscularis externa:
Lamina propria
Muscularis
mucosae
Circular layer
Longitudinal
layer
Figure 11.22
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.

11-95
Excitation of Smooth Muscle
• Smooth muscle is involuntary and can contract (or
relax) in response to a variety of stimuli
– Autonomic activity
• Parasympathetic nerves secrete acetylcholine stimulating GI tract
smooth muscle
• Sympathetic nerves secrete norepinephrine relaxing smooth
muscle in bronchioles (dilating them)
– Hormones, carbon dioxide, oxygen, and pH
• Hormone oxytocin stimulates uterine contractions
– Temperature
• Cold excites piloerector muscles
• Warmth relaxes muscle in skin blood vessels
– Stretch
• Stomach contracts when stretched by food
– Autorhythmicity
• Some single-unit smooth muscle cells in GI tract are
pacemakers

11-96
Contraction and Relaxation
• Contraction is always triggered by Ca
2+
,
energized by ATP, and achieved by sliding
filaments
• Smooth muscle gets most Ca
2+
from ECF
– Gated Ca
2+
channels open to allow Ca
2+
to enter cell
– Calcium channels are concentrated in caveolae—
pockets on sarcolemma
– Different channels gated by different stimuli
• Can respond to mechanical stretch, voltage, or chemical ligands

11-97
Contraction and Relaxation
• Calcium binds to calmodulin on thick filaments
– Activates myosin light-chain kinase; adds phosphate to
regulatory protein on myosin head
• Myosin ATPase, hydrolyzes ATP
– Enables myosin similar power and recovery strokes like
skeletal muscle
• Thick filaments pull on thin ones, thin ones pull on
dense bodies and membrane plaques
• Force is transferred to plasma membrane and entire
cell shortens
– Puckers and twists like someone wringing out a wet towel

11-98
Smooth Muscle Contraction
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Dense body
Intermediate filaments
of cytoskeleton
Actin filaments
(b) Contracted smooth
muscle cells
(a) Relaxed smooth muscle cells
Plaque
Myosin
Figure 11.24a,b

11-99
• Contraction and relaxation very slow in
comparison to skeletal muscle
– Latent period in smooth muscle 50 to 100 ms (versus
2 ms in skeletal muscle)
– Tension peaks at about 500 ms (0.5 sec)
– Declines over a period of 1 to 2 seconds
– Slow myosin ATPase enzyme and pumps that
remove Ca
2+
– Ca
2+
binds to calmodulin instead of troponin
• Activates kinases and ATPases that hydrolyze ATP
Contraction and Relaxation

11-100
• Latch-bridge mechanism is resistant to fatigue
– Heads of myosin molecules do not detach from actin
immediately
– Do not consume any more ATP
– Maintains tetanus tonic contraction (smooth muscle
tone)
• Arteries—vasomotor tone; intestinal tone
– Makes most of its ATP aerobically
Contraction and Relaxation

11-101
Response to Stretch
• Stretch can open mechanically gated calcium
channels in the sarcolemma causing contraction
– Peristalsis: waves of contraction brought about by food
distending the esophagus or feces distending the colon
• Propels contents along the organ
• Stress–relaxation response (receptive relaxation)—
helps hollow organs gradually fill (urinary bladder)
– When stretched, tissue briefly contracts then relaxes;
helps prevent emptying while filling

11-102
• Skeletal muscle cannot contract forcefully if
overstretched
• Smooth muscle contracts forcefully even
when greatly stretched
– Allows hollow organs such as the stomach and
bladder to fill and then expel their contents efficiently
• Plasticity—the ability to adjust its tension to the
degree of stretch
– A hollow organ such as the bladder can be greatly
stretched yet not become flabby when empty
Response to Stretch

11-103
• Smooth muscle can be anywhere from half to
twice its resting length and still contract
powerfully
• Three reasons
– There are no Z discs, so thick filaments cannot butt
against them and stop contraction
– Since the thick and thin filaments are not arranged in
orderly sarcomeres, stretching does not cause a
situation where there is too little overlap for cross-
bridges to form
– The thick filaments of smooth muscle have myosin
heads along their entire length, so cross-bridges can
form anywhere
Response to Stretch

11-104
Muscular Dystrophy
• Muscular dystrophy―group of hereditary diseases in
which skeletal muscles degenerate and weaken, and
are replaced with fat and fibrous scar tissue
• Duchenne muscular dystrophy is caused by a sex-
linked recessive trait (1 of 3,500 live-born boys)
– Most common form
– Disease of males; diagnosed between 2 and 10 years of age
– Mutation in gene for muscle protein dystrophin
• Actin not linked to sarcolemma and cell membranes damaged
during contraction; necrosis and scar tissue result
– Rarely live past 20 years of age due to effects on respiratory
and cardiac muscle; incurable

11-105
Muscular Dystrophy
• Facioscapulohumeral MD―autosomal dominant
trait affecting both sexes equally
– Facial and shoulder muscles more than pelvic muscles
• Limb-girdle dystrophy
– Combination of several diseases of intermediate severity
– Affects shoulder, arm, and pelvic muscles

11-106
Myasthenia Gravis
• Autoimmune disease in which antibodies
attack neuromuscular junctions and bind ACh
receptors together in clusters
– Usually occurs in women between 20 and 40
– Muscle fibers then remove the clusters of receptors from
the sarcolemma by endocytosis
– Fiber becomes less and less sensitive to Ach
– Effects usually first appear in facial muscles
• Drooping eyelids and double vision, difficulty swallowing, and
weakness of the limbs
– Strabismus: inability to fixate on the same point with
both eyes

11-107
Myasthenia Gravis
• Treatments for Myasthenia Gravis
– Cholinesterase inhibitors retard breakdown of ACh
allowing it to stimulate the muscle longer
– Immunosuppressive agents suppress the production
of antibodies that destroy ACh receptors
– Thymus removal (thymectomy) helps to dampen the
overactive immune response that causes myasthenia
gravis
– Plasmapheresis: technique to remove harmful
antibodies from blood plasma

11-108
Myasthenia Gravis
• Drooping eyelids and weakness of muscles of eye
Figure 11.25
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
