IRS EXEMPT ORGANIZATIONS (TE/GE)
HOSPITAL COMPLIANCE PROJECT
FINAL REPORT
TABLE OF CONTENTS (DETAILED) (pages ii-iv)
I. INTRODUCTION AND SYNOPSIS (pages 1-10)
II. INTERIM REPORT AND ADDITIONAL WORK UNDERTAKEN FOR FINAL
REPORT (pages 11-15)
III. BACKGROUND ON U.S. HOSPITALS AND PRIOR STUDIES (pages 16-21)
IV. DEMOGRAPHICS – PATIENT MIX, REVENUES, EXCESS REVENUES
(pages 22-38)
V. DIFFERENCES IN COMMUNITY BENEFIT REPORTING ACROSS CERTAIN
DEMOGRAPHICS
• By Community Type (pages 39-65)
• By Revenue Size (pages 66-92)
VI. OTHER COMMUNITY BENEFIT REPORTING – BAD DEBT AND
SHORTFALLS, RESEARCH, INCOME AND HEALTH INSURANCE
COVERAGE LEVELS (pages 93-121)
VII. EXECUTIVE COMPENSATION (pages 122-146)
VIII. FORM 990, SCHEDULE H, HOSPITALS (pages 147-151)
IX. SUMMARY OF FINDINGS BY DEMOGRAPHIC
• Narrative Description (pages 152-166)
• Quick Reference Tables (pages 167-168)
X. KEY OBSERVATIONS AND LESSONS LEARNED (pages 169-171)
APPENDICES
A. List of Charts and Tables
B. Form 13790, Compliance Check Questionnaire Tax-Exempt Hospitals
C. Form 990, Schedule H, Hospitals
i
TABLE OF CONTENTS (DETAILED)
I. INTRODUCTION AND SYNPOSIS
A. Introduction and Limitations on Analysis
B. Demographics and Key Findings
C. Summary of Demographics and Community Benefit
1. Patient Mix
2. Community Benefit Expenditures (percentages of total
revenues)
3. Community Benefit Expenditures Mix (uncompensated care,
medical education and training, medical research, community
programs)
4. Uncompensated Care (percentages of total revenues)
5. Comparison of Reported Uncompensated Care and Community
Benefit Expenditures against Specified Percentage of Revenue
Levels
6. Revenues vs. Expenses
D. Executive Compensation
II. INTERIM REPORT AND ADDITIONAL WORK UNDERTAKEN FOR FINAL
REPORT
A. Questionnaire Content Included in Final Report
B. Significant Adjustments to the Interim Report
C. Breakdown of Hospitals by Community Types (High Population, Critical
Access Hospital (CAH), Rural (non-CAH), and Other Urban and
Suburban Hospitals)
D. Breakdown of Hospitals by Revenue Size
E. Hospitals Reporting Largest Amounts of Medical Research
Expenditures
F. Analysis of Bad Debt and Shortfalls as Uncompensated Care
G. Comparison of Reported Community Benefit Expenditures Across
Communities Based on Income and Insurance Coverage Levels
H. Executive Compensation
I. Form 990, Schedule H, Hospitals
III. BACKGROUND ON U.S. HOSPITALS AND PRIOR STUDIES
A. Background on U.S. Hospitals
B. Other Studies on Community Benefit Provided by Nonprofit Hospitals
C. Study on Executive Compensation of Nonprofit Hospitals
IV. DEMOGRAPHICS - PATIENT MIX, REVENUES, EXCESS REVENUES
A. Patient Insurance Coverage
B. Revenues and Excess Revenues By Revenue Size
C. Revenues and Excess Revenues by Community Type
D. Relationship Between Community Type and Revenue Size
E. Groupings by Excess Revenues
ii
V. DIFFERENCES IN COMMUNITY BENEFIT REPORTING ACROSS
CERTAIN DEMOGRAPHICS - COMMUNITY TYPES, REVENUE SIZE
A. Introduction
B. Comparison of Certain Information By Community Type
1. Summary of Key Findings – Community Type
2. Patient Mix (Based on Type of Insurance Coverage) by
Community Type
3. Number and Percentage of Hospitals Reporting Community
Benefit Expenditures, by Expenditure Type within Community
Type
4. Aggregate Uncompensated Care by Community Type
5. Aggregate Medical Research Expenditures by Community Type
6. Aggregate Medical Education and Training Expenditures by
Community Type
7. Aggregate Community Program Expenditures by Community
Type
8. Aggregate Community Benefit Expenditures by Community
Type
9. Aggregate Community Benefit Expenditures as a Percentage of
Revenues
C. Comparisons of Certain Information By Annual Revenue Size
1. Summary of Key Findings – Revenue Size
2. Patient Mix (Based on Type of Insurance Coverage) by
Revenue Size
3. Number and Percentage of Hospitals Reporting Community
Benefit Expenditures, by Expenditure Type within Revenue Size
4. Aggregate Uncompensated Care by Revenue Size
5. Aggregate Medical Research Expenditures by Revenue Size
6. Aggregate Medical Education and Training Expenditures by
Revenue Size
7. Aggregate Community Program Expenditures by Revenue Size
8. Aggregate Community Benefit Expenditures by Revenue Size
9. Aggregate Community Benefit Expenditures as a Percentage of
Revenues
VI. OTHER COMMUNITY BENEFIT REPORTING - BAD DEBT AND
SHORTFALLS, RESEARCH, INCOME AND HEALTH INSURANCE
COVERAGE LEVELS
A. Overview and Summary of Key Findings
B. Hospitals Reporting Largest Amounts of Medical Research
Expenditures
C. Analysis of Bad Debt and Shortfalls as Uncompensated Care
1. Reporting of Shortfalls and Bad Debt by Community Type
2. Reporting of Shortfalls and Bad Debt by Revenue Size
3. Reporting Differences when Shortfalls and Bad Debts are
Included in Uncompensated Care
iii
iv
D. Comparison of Community Benefit Expenditures Across Various
Income and Health Insurance Coverage Levels
1. Overview
2. Community Benefit Expenditures Across Community Per Capita
Income Levels
3. Community Benefit Expenditures Across Community Health
Insurance Coverage Levels
4. Interaction Between Per Capita Income and Health Insurance
Coverage
VII. EXECUTIVE COMPENSATION
A. Overview
B. Summary of Compensation Practices as Reported by Responding
Hospitals
C. Summary of Examinations
1. Overview of Examination Component of the Project
2. Examination Results
VIII. FORM 990, SCHEDULE H, HOSPITALS
A. Overview of Schedule H, Hospitals
B. Description of Schedule H, Parts I through VI
C. Transition Relief
D. Promoting Uniform Reporting through Schedule H
IX. SUMMARY OF FINDINGS BY DEMOGRAPHIC
X. KEY OBSERVATIONS AND LESSONS LEARNED
APPENDICES
A. List of Charts and Tables
B. Form 13790, Compliance Check Questionnaire Tax-Exempt Hospitals
C. Form 990, Schedule H, Hospitals

I. INTRODUCTION AND SYNOPSIS
A. Introduction and Limitations on Analysis
The IRS commenced its Hospital Compliance Project (Project) in May 2006 to
study nonprofit hospitals and community benefit, and to determine how nonprofit
hospitals establish and report executive compensation. The Project involved
mailing out a comprehensive compliance check questionnaire to 544 nonprofit
hospitals and analyzing their responses.
1
The questionnaire (see Appendix B)
requested information regarding the hospital’s activities, governance,
expenditures, and executive compensation practices. The Project also involved
examinations of 20 hospitals regarding executive compensation issues.
The hospitals included in the study represent a modest portion of the nonprofit
hospital sector. See Section III, below, for a discussion of background on U.S.
hospitals and of other recent government reports on community benefit and
executive compensation provided by nonprofit hospitals.
The IRS issued its Interim Report on Hospital Compliance Project on July 19,
2007 (Interim Report). The Interim Report addressed only the community benefit
aspects of the questionnaire and presented data gathered from the questionnaire
responses of 487 hospitals and certain information reported on Forms 990 filed
by responding hospitals. The executive compensation component of the Project
was not addressed in the Interim Report because the examinations were ongoing
at the time of the report’s release.
The Final Report addresses the “next steps” identified in the Interim Report.
These are:
• Analyze the reported data to determine whether differences in reporting,
such as the treatment of bad debt and shortfalls as uncompensated care,
may be isolated and adjusted to allow more meaningful comparisons
across the respondents.
• Obtain additional research and analyze the differences in community
benefit expenditure amounts and types to take into account varying
demographics, such as rural and urban communities and hospitals.
• Test the reported community benefit amounts and types by conducting
data analysis, compliance checks, or examinations of individual hospitals,
and by other means, including with respect to outliers in the reported
data.
1
A copy of the questionnaire is attached as Appendix B. In selecting the hospitals to be
contacted, the IRS queried its files to identify nonprofit hospitals exempt under section 501(c)(3).
From an initial identified universe of approximately 6,000 entities, the IRS selected 544
organizations that it confirmed as hospitals. The IRS sent compliance questionnaire letters to
each of these hospitals, which were of varying sizes and types and were located in different
regions and communities across the United States. Some judgment was used to identify
hospitals which were not uniquely identifiable in the IRS database. The resulting sample may or
may not reflect the nonprofit hospital sector in general.
1

The IRS also indicated it would (1) follow up on the 11 hospitals that did not
respond to the questionnaire; (2) continue its work on the Form 990, Schedule H,
Hospitals;
2
and (3) complete the executive compensation component of the
project.
The IRS continued to study the information provided by the responding hospitals,
and obtained additional information regarding 11 hospitals that initially did not
respond to the questionnaire. The numbers reported in the Interim Report have
been adjusted in the Final Report to reflect this further study and additional
information. Significant adjustments to the data reported in the Interim Report
are listed in Section II, below. The Final Report includes 489 respondent
hospitals that reported community benefit expenditures, but generally
summarizes data for the 485 hospitals that actually provided sufficiently complete
community benefit data. There are other situations in which certain respondents
did not provide sufficient information to permit categorization of all of the
indices/variables considered in this report. Sample sizes will vary as a result.
Throughout the report, certain information was not included or was combined
with other information to prevent potential identification of respondent hospitals.
In addition, because of rounding conventions, some figures may not reconcile
(including that, in some cases, the combined data for individual categories of a
group may be slightly more or less than 100%).
The findings of the Final Report are subject to a number of limitations. Except for
certain compensation data that was reviewed through examinations, the data
reported by the respondents was not independently verified. In addition, the data
reported responds to a single tax year and may not be representative of results
for a different tax year or on an ongoing basis. Results for a different year could
vary significantly depending on a variety of factors, including, for example, the
economic climate. It is also important to note that the percentage of hospitals
included in the various categories used in the report (e.g., community type) may
not be representative of the sector at large. This may have an effect on certain
findings in the report.
The study found significant variations from community benefit reporting that will
be required by the new Form 990 Schedule H beginning with 2009 tax years.
The community benefit expenditures reported by some hospitals appear to
overstate Form 990 reportable community benefit, due to reporting
uncompensated care based on charges rather than on costs, or including bad
debt, Medicare shortfalls, and private insurance shortfalls as community benefit.
On the other hand, exclusion by some hospitals of shortfalls from Medicaid, other
means-tested public programs, or uninsured patients as uncompensated care,
may understate the Form 990 reportable community benefit attributable to those
programs.
2
See Appendix C for a copy of Form 990, Schedule H, released in official form on December 24,
2008.
2

For these and other reasons, the summarized community benefit data is subject
to material limitations, and may not accurately depict the community benefit
actually provided by the respondents or by nonprofit hospitals as a whole.
Notwithstanding these limitations, some interesting findings are suggested in
both the community benefit and compensation areas of the study.
B. Demographics and Key Findings
The hospitals were classified into four community types based on location of the
hospital and in part on Census Bureau data: high population, other urban and
suburban, critical access hospitals, and rural non-critical access hospitals. The
94 hospitals (19%) located in the 26 largest urban areas in the United States
were categorized in the high population category. The other 249 hospitals (51%)
located in Census Bureau urban areas were included in the other urban and
suburban category. The 68 hospitals (14%) designated as critical access
hospitals under federal law were categorized in the critical access hospital (CAH)
category. The 78 hospitals (16%) that are not CAHs and not located in any
Census Bureau urban area were categorized in the rural (non-CAH) category.
The hospitals also were classified by revenue size based on annual revenues as
reported on Forms 990 as follows: (1) under $25 million, 85 hospitals (17%); (2)
$25 million to $100 million, 173 hospitals (36%); (3) $100 million to $250 million,
133 hospitals (27%); (4) $250 million to $500 million, 61 hospitals (13%); and (5)
over $500 million, 36 hospitals (7%). For purposes of this section, reporting of
revenue size categories generally is limited to the smallest and largest
categories, where the differences are most pronounced.
The hospitals also were categorized and examined based on health insurance
coverage and per capita income of the area surrounding the hospital. In addition,
a group of 15 hospitals reporting nearly all (93%) of the reported medical
research expenditures was studied.
1. Diversity of nonprofit hospitals. There was considerable diversity in the
demographics, activities, and financial resources among the respondent
hospitals. The types and amounts of uncompensated care and other community
benefit expenditures varied by the hospitals across revenue size, income and
insurance coverage levels of the surrounding area, and the hospital’s setting
within a rural, suburban, or urban community. In particular, significant
differences were observed between the groups of critical access hospitals and
hospitals in the high population areas, and between the smallest and largest
groups of hospitals based on revenue size (e.g., in general, larger hospitals
reported higher community benefit expenditures and higher excess revenues).
2. Aggregate community benefit
. The average and median percentages of total
revenues reported as spent on aggregate community benefit expenditures were
9% and 6%, respectively, for the overall group. Among the community types,
3

these percentages were lowest for rural hospitals (CAH and non-CAH) and
highest for hospitals in the high population areas. These percentages generally
increased with revenue size. For the group of 15 hospitals reporting
disproportionately large medical research expenditures, the average and median
percentages of total revenues reported as spent on aggregate community benefit
expenditures were both 19%.
3. Types of community benefit. Uncompensated care was the largest reported
community benefit expenditure overall and across all demographics, other than
for the group of 15 hospitals that reported nearly all of the aggregate medical
research expenditures. Overall, the average and median percentages of
uncompensated care as a percentage of total revenues were 7% and 4%,
respectively. Reported uncompensated care expenditures were 56% of
aggregate community benefit expenditures. Medical education and training
expenditures constituted 23% of aggregate reported expenditures, followed by
medical research (15%), and community programs (6%). This mix varied by
community type and revenue size, and as described below, materially changed
when the group of 15 hospitals reporting disproportionately large medical
research expenditures was excluded.
4. Concentration of expenditures in small group of hospitals. Uncompensated
care and aggregate community benefit expenditures were unevenly distributed
among hospitals and concentrated in a relatively small group. The study looked
at reported community benefit compared to certain specified revenue levels.
Overall, 58% of hospitals reported uncompensated care amounts less than or
equal to 5% of total revenues. Overall, 21% of the hospitals reported aggregate
community benefit expenditures less than 2% of total revenues; 47% reported
aggregate community benefit expenditures less than 5% of revenues. Critical
access hospitals and the smallest hospitals generally reported higher
percentages of hospitals below these levels. High population hospitals and the
largest hospitals generally reported lower percentages of hospitals below these
levels.
5. Revenues vs. expenses
. Reported excess revenues (total revenues less
expenses) varied across the demographics. Overall, when data was aggregated
for all hospitals, revenues exceeded expenses by 5%. This percentage was 3%
for the smallest hospitals and increased with revenue size. Among the
community types, critical access hospitals reported the smallest percentage, and
other rural hospitals reported the largest percentage. Overall, 21% of the
hospitals reported a deficit (total expenses greater than total revenues). The
percentage of hospitals reporting deficits varied by community type and revenue
size.
6. Community income and insurance coverage levels. The study did not find a
correlation between community benefit expenditure levels and per capita income
levels of the area surrounding the hospital. The study did, however, observe that
4

community benefit expenditure levels generally increased as uninsured rates of
the area surrounding the hospital increased.
7. Compensation practices. Nearly all hospitals in the study reported complying
with key elements of the rebuttable presumption procedure available to establish
compensation of certain executives and disqualified persons. Based on
traditional risk analysis and the compensation examinations of 20 hospitals, the
study found widespread compliance with the Section 4958 excess benefit
transaction rules. Although many reported compensation amounts appeared to
be high, nearly all amounts reviewed in these examinations were upheld as
established pursuant to the rebuttable presumption process and within the range
of reasonable compensation.
C. Summary of Demographics and Community Benefit
The following summarizes key demographic or community benefit measures.
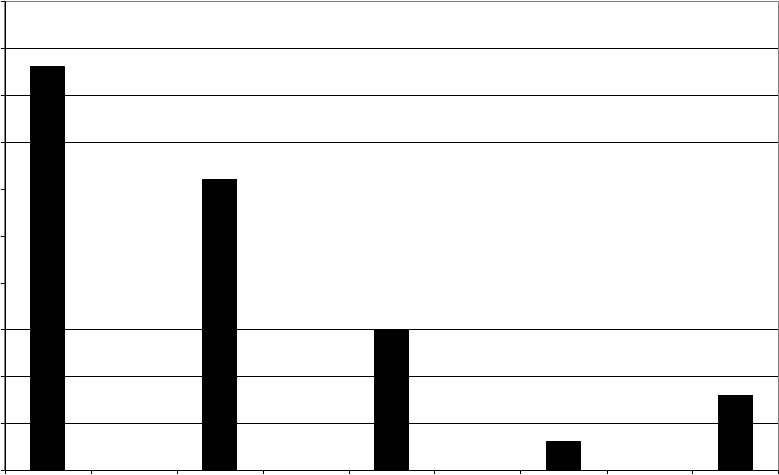
1. Patient Mix
The reported patient mix of the overall group of hospitals showed that the highest
percentage of patients was private insurance patients (43%), followed by
Medicare (31%), Medicaid (15%), uninsured (8%), and other public programs
(3%).
Patient Mix
0%
10%
20%
30%
40%
50%
High-Population Critical Access Rural non-CAH Other Urban &
Suburban
< $25M $500M+
Community Type Revenues
Percentage of Patients
Private Insurance Medicare Medicaid Other Public Uninsured
Critical access hospitals and the smallest hospitals reported the lowest
percentage of private insurance patients and the highest percentage of Medicare
patients. High population hospitals and the largest hospitals had the highest
percentage of Medicaid patients.
5

2. Community Benefit Expenditures (percentages of total revenues)
The overall average and median percentages of total revenues reported as spent
on aggregate community benefit expenditures were 9% and 6%, respectively.
These percentages varied across community type and revenue size. Aggregate
community benefit expenditures were not evenly distributed by the hospitals in
the study, but were concentrated in a relatively small number of hospitals. 9% of
the hospitals reported 60% of the aggregate community benefit expenditures;
19% of the hospitals reported 78% of the aggregate community benefit
expenditures.
Community Benefit Expenditures as Percentage of Total Revenues
12.7%
6.3%
8.4%
8.9%
9.9%
9.8%
2.8%
3.2%
5.8%
3.3%
10.5%
19.0%
12.4%
0%
2%
4%
6%
8%
10%
12%
14%
16%
18%
20%
High
Population
Critical
Access
Rural non-
CAH
Other Urban &
Suburban
< $25M $500M+ Research
Community Type Revenues
Average
Median
Among community types, the percentages were lowest for critical access
hospitals and highest for high population hospitals. The percentages of total
revenues generally increased with revenue size. The highest reported average
and median percentages were by the group of 15 hospitals that reported nearly
all of the medical research expenditures (referred to as “research hospitals” for
this section).
3. Community Benefit Expenditures Mix (uncompensated care,
medical education and training, medical research, community
programs)
Uncompensated care was the largest component of reported community benefit
for each community type and revenue size category, but the composition varied
across the demographics.
6

Composition of Community Benefit Expenditures
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
High-Population Critical Access Rural non-CAH Other Urban &
Suburban
< $25M $500M+
Community Type Revenues
Percentage of Community Benefit Expenditures
Uncompensated Care Medical Training Medical Research Community Programs
Uncompensated care as a percentage of overall community benefit expenditures
was greatest for CAHs, other rural hospitals, and the smallest hospitals.
Significant variations were observed in reported expenditures for medical
education and training expenditures and medical research across the community
types. Both medical education and training and medical research expenditures
as a percentage of overall community benefit expenditures increased with
revenue size. The inclusion
of bad debt and various
shortfalls impacted the
uncompensated care levels
reported. Overall, and for
each community type and
revenue size, greater
percentages of hospitals
reported including bad debt
and self pay shortfalls in
uncompensated care than
any other types of shortfalls.
The community benefit mix
changed materially when
Communit
y
Benefit Expenditure Mix with Research
Breakout
45%
15%
22%
71%
56%
28%
21%
23%
5%
7%
6%
0% 20% 40% 60% 80% 100%
Research
Hospitals
Hospitals other
than Research
All
Hospitals
% of Total CBE
Medi c al Researc h Uncompensated Care Medical Training Community Programs
7

the group of 15 hospitals that reported nearly all of the medical research
expenditures was removed. The figure above shows the mix for the overall
group, the group of 15 hospitals reporting nearly all of the medical research
expenditures, and the overall group without the 15 hospitals.
4. Uncompensated Care (percentages of total revenues)
The average and median percentages of total revenues reported as spent on
uncompensated care were 7% and 4%, respectively. Uncompensated care
expenditures were not evenly distributed among the hospitals in the study, but
were concentrated in a relatively small number of hospitals. 14% of the hospitals
reported 63% of the aggregate uncompensated care expenditures; 26% of the
hospitals reported 82% of the aggregate uncompensated care expenditures.
Uncompensated Care as Percentage of Total Revenues
7.9%
5.6%
7.6%
7.3%
9.3%
5.6%
6.2%
4.8%
2.1%
2.7%
4.3%
3.1%
4.7%
3.3%
0%
2%
4%
6%
8%
10%
High
Population
Critical
Access
Rural non-
CAH
Other Urban &
Suburban
< $25M $500M+ Research
Community Type Revenues
Average
Median
Critical access hospitals reported the lowest percentages and high population
hospitals reported the highest percentages among the community types. The
group of smallest hospitals reported the highest average percentage, but the
lowest median percentage, among the revenue size groups.
5. Comparison of Reported Uncompensated Care and Community
Benefit Expenditures against Specified Percentage of Revenue
Levels
The figure below displays the percentage of hospitals with reported community
benefit and uncompensated care expenditures at or less than specified
percentage of revenue levels.
8

Demographic:
% of hospitals with
community benefit
expenditures <2% of
revenues
% of hospitals with
community benefit
expenditures <5% of
revenues
% of hospitals with
uncompensated
care expenditures
≤3% of revenues
% of hospitals with
uncompensated
care expenditures
≤5% of revenues
High population 11% 32% 33% 52%
CAH 39% 61% 59% 67%
Rural – non CAH 31% 57% 52% 65%
Other urban and suburban 17% 46% 39% 55%
Under $25 million 34% 60% 49% 60%
$25 million to under $100 million 30% 56% 49% 61%
$100 million to under $250 million 12% 42% 37% 55%
$250 million to under $500 million * * 34% 49%
Over $500 million * * 33% 60%
Overall 21% 47% 43% 58%
* The two largest revenue sizes were combined to prevent potential identification of respondent hospitals.
In the combined group ($250 million and over), the percentage of hospitals with community benefit
expenditures less than 2% of revenues is 5%, and less than 5% of revenues is 27%.
6. Revenues vs. Expenses
79% of the hospitals reported excess revenues (revenues exceeding expenses
as reported on the Form 990), and 21% reported that total expenses exceeded
total revenues (i.e., reported a deficit). The percentage of hospitals that reported
revenue deficits decreased as revenue size increased, and varied across the
community types. CAHs and the smallest hospitals had the highest percentage
of hospitals reporting a deficit.
Distribution of Hospitals by Excess Revenue
26%
10%
15%
19%
15%
20%
22%
22%
14%
21%
13%
19%
31%
34%
58%
39%
36%
51%10%
35%
20%
13%
34%
22%
-40% -20% 0% 20% 40% 60% 80% 100%
High Population
Critical Access
Rural non-CAH
Other Urban & Suburban
< $25M
$250M +
Community TypeRevenues
Percentage of Hospitals
Deficit or 0% Excess Revenues >0% to <2.5% Excess Revenues 2.5% to <5% Excess Revenues ≥5%
← Deficit | Excess →
Overall, excess revenues expressed as a percentage of total revenues was 4.6%
and increased with revenue size. Among community types, critical access
hospitals reported the lowest percentage (4%), and other rural hospitals reported
the highest percentage (6%).
D. Executive Compensation
9
The study’s questionnaire asked various questions regarding each hospital’s
compensation practices. These involved reporting compensation amounts for
the hospital’s officers, directors, trustees, and key employees, as well as
information regarding certain policies and practices used to establish
compensation for such persons. In addition, the study involved the examination
of 20 organizations regarding their executive compensation practices.
In general, the hospitals reported widespread compliance with key indicators of
sound compensation practices, including use of formal written compensation
policies, use of comparability data, approval in advance by persons without a
conflict of interest, and setting compensation within the range of comparability
data. This pattern was reported consistently across the community types and
revenue size categories, and was confirmed in the examinations of the 20
hospitals.
The average and median compensation amounts paid to the top management
official as reported on the questionnaire were $490,000 and $377,000,
respectively. Compensation amounts varied across demographics, but generally
increased as the hospital’s revenue size increased. Generally, rural hospitals
(CAH and non-CAH) paid lower compensation than did urban and suburban
hospitals (high population and other urban and suburban).
For the 20 hospital compensation examinations, the average and median
compensation amounts paid to the top management official were $1.4 million and
$1.3 million, respectively. Because the examined hospitals were selected on the
basis of higher reported compensation amounts, a disparity between the overall
group and the examined hospitals was expected.
10
II. INTERIM REPORT AND ADDITIONAL WORK UNDERTAKEN FOR FINAL
REPORT
A. Questionnaire Content Included in Final Report
The primary focus of the Final Report’s work was to analyze differences in
community benefit expenditures among the respondent hospitals. This Final
Report provides breakdowns by demographics for several of the questionnaire’s
key areas, including aggregate community benefit expenditures, uncompensated
care, medical education and training, medical research, and community
programs. These include the following questions:
• Patients covered by private insurance, Medicare, Medicaid, other public
insurance, no insurance – questions 2 through 7
• Medical research expenditures – questions 21 and 22
• Professional medical education and training – questions 30 and 31
• Uncompensated care – questions 35 through 38, 40
• Community programs – questions 57, 58, 61, 62, 65, 66, 69 through 71
B. Significant Adjustments to the Interim Report
The Interim Report included data comparing various hospital expenses, including
certain community benefit expenditures, as a percentage of total revenue. These
revenue numbers were derived from the organizations’ most recently filed Forms
990 that had been received by the IRS at the time the questionnaire information
for that hospital was being reviewed and analyzed. After the issuance of the
Interim Report, additional Forms 990 for certain of the respondent hospitals were
received by the IRS, allowing the use of revenue information from the tax year to
which the questionnaire’s expense and community benefit expenditure
information pertains. Accordingly, in this Final Report, the total revenue
information is taken from the Form 990 that corresponded to the tax year which
each hospital used to complete the questionnaire.
This adjustment significantly changed some of the calculations of expenses
reported as a percentage of revenue for those hospitals that had a large change
in revenue from the Form 990 for the tax year initially used in the Interim Report.
Changes also resulted from continued analysis of narrative and other information
provided by the responding hospitals and from correcting data entry and
transcription errors.
The most significant changes are described as follows.
1. Average and median annual total revenues of the responding hospitals.
The Interim Report reported average and median annual total revenues of
all of the hospitals in the study as $169 million and $83 million,
respectively. The average and median annual total revenues of all of the
11

hospitals in the study were adjusted upward to $179 million and $89
million, respectively. These upward adjustments in total revenues affected
many of the percentages reported in the Interim Report that used total
revenues in the denominator (e.g., percentage of total revenues spent on
community program expenditures).
2. Patient Mix. The Final Report shows a change in the reported patient
insurance coverage mix from 46% to 43% for private insurance, 46% to
49% for public programs (Medicare, Medicaid, and other public programs),
and 7% to 8% with no insurance coverage.
3. Medical Research. The average of the percentages of total revenues
spent on medical research by these hospitals was adjusted downward
from 8% to 2% while the median decreased from 0.24% to 0.22%.
3
4. Community Programs. The averages and medians of the percentages of
total revenue spent on aggregate community programs, and on the
various components of community programs (e.g., immunization
programs), have been revised. The most significant change was the
downward adjustment of the average percentage of total revenue reported
to have been spent on aggregate community programs from 3.4% to
0.9%.
C. Breakdown of Hospitals by Community Types (High Population, Critical
Access Hospital (CAH), Rural (non-CAH), and Other Urban and Suburban
Hospitals)
To assess differences in community benefit expenditure amounts and types to
take into account varying demographics such as rural, suburban, and urban
communities and hospitals, the Final Report establishes four “community types”
and reports much of the aggregate community benefit expenditure data across
these four community types. These community types attempt to reflect
demographic areas commonly regarded as urban, suburban, and rural.
The hospitals located in rural areas were divided between those that are critical
access hospitals and those that are not critical access hospitals (as described in
more detail below). These groups are referred to as “critical access hospitals” (or
“CAH”) and “rural (non-CAH).” The remaining hospitals were divided into two
groups. Those hospitals located in the 26 largest urban areas in the United
States were categorized in the “high population” category. The other hospitals
located in urban or suburban areas were included in the “other urban and
suburban” category (referred to in the figures as “other”).
Based on the reported data, the 489 hospitals were classified into community
types as follows:
• “High population” – 94 hospitals (19%)
3
A significant component of the downward adjustment in the average is due to the correction of
a data entry and transcription error made during the study.
12

• “Critical access hospitals (CAH)” – 68 hospitals (14%)
• “Rural (non-CAH)” – 78 hospitals (16%)
• “Other urban and suburban” – 249 hospitals (51%).
The community types are defined as follows:
High population. “High population” refers to the hospitals in the study that are
located in the 26 urban areas in the United States that had populations of 1.5
million or more people, based on the 2000 Census. The U.S. Census Bureau
defines an urban area as core census block groups or blocks that have a
population density of at least 1,000 people per square mile, and surrounding
census blocks that have an overall density of at least 500 people per square
mile.
4
Based on this definition, some of the hospitals in this group are located in
what people commonly consider the suburbs of large cities, but other hospitals
located in many large cities are not included in this group.
The urban areas included in the high population community type are displayed in
the map below.
Other urban and suburban. “Other urban and suburban” refers to hospitals that
are located in any Census Bureau urban area that had a population of less than
1.5 million according to the 2000 Census. Accordingly, these hospitals are
located in all the Census Bureau urban areas other than the 26 largest urban
areas included in the high population category.
4
See www.census.gov (http://www.census.gov/geo/www/ua/ua_2k.html).
13

Critical access hospitals (CAHs). “Critical access hospital” refers to all the
hospitals in the study that are designated critical access hospitals by the
Department of Health and Human Services or otherwise under federal law.
CAHs must be certified by the Centers for Medicare & Medicaid Services (CMS),
an agency within the Department of Health and Human Services. A facility that
meets the following criteria may be designated by CMS as a CAH:
5
• Is located in a State that has established with CMS a Medicare rural
hospital flexibility program; and
• Has been designated by the State as a CAH; and
• Is currently participating in Medicare as a rural public, non-profit or for-
profit hospital; or was a participating hospital that ceased operation during
the 10-year period from November 29, 1989 to November 29, 1999; or is a
health clinic or health center that was downsized from a hospital; and
• Is located in a rural area or is treated as rural; and
• Is located more than a 35-mile drive from any other hospital or CAH (in
mountainous terrain or in areas with only secondary roads available, the
mileage criterion is 15 miles); and
• Maintains no more than 25 inpatient beds; and
• Maintains an annual average length of stay of 96 hours per patient for
acute inpatient care; and
• Complies with all CAH Conditions of Participation, including the
requirement to make available 24-hour emergency care services 7 days
per week.
Rural (non-CAH). “Rural (non-CAH)” refers to the hospitals in the study that are
not located in any Census Bureau urban area and are not CAHs. CMS provided
the IRS with a list of rural hospitals that are not CAHs which CMS used in its
Fiscal Year 2009 inpatient prospective payment system (IPPS) proposed rule
impact file. IPPS is used to set payment rates for acute care hospitals that are
not compensated under the CAH system. This CMS list was then compared to
the list of hospitals in the study as a way of confirming these were located
outside of Census Bureau urban areas.
D. Breakdown of Hospitals by Revenue Size
The Final Report provides breakdowns of aggregate information by revenue size,
based on annual revenue as reported in Forms 990. Based on reported data, the
IRS was able to classify 488 hospitals as follows:
• Under $25 million – 85 hospitals (17%)
• $25 million to $100 million – 173 hospitals (36%)
5
See www.cms.hhs.gov (http://www.cms.hhs.gov/CertificationandComplianc/04_CAHs.asp); 42
U.S.C. 1395X(mm); 42 U.S.C. 1395i-4(e); 42 C.R.F. 485.606.
14
• $100 million to $250 million – 133 hospitals (27%)
• $250 million to $500 million – 61 hospitals (13%)
• Over $500 million – 36 hospitals (7%).
E. Hospitals Reporting Largest Amounts of Medical Research Expenditures
The Final Report categorizes a group of 15 hospitals that reported 93% of the
medical research expenditures reported by the respondent hospitals. The report
also summarizes key community benefit expenditure data regarding this group,
and isolates the impact of this group’s medical research expenditures on the
overall group’s reported community benefit expenditures. See Section VI.B,
below.
F. Analysis of Bad Debt and Shortfalls as Uncompensated Care
The Final Report analyzes reporting of bad debt and shortfalls from insurance,
government programs, and uninsured patients, across community types and
revenues sizes. These results are described in Section VI.C, below.
G. Comparison of Reported Community Benefit Expenditures Across
Communities Based on Income and Insurance Coverage Levels
The Final Report analyzes reporting of community benefit expenditures along
certain per capita income and insurance coverage levels to determine whether
reported uncompensated care varied by income and insurance coverage levels
of the communities served by the responding hospitals. See Section VI.D,
below.
H. Executive Compensation
The Final Report summarizes the data provided by the respondent hospitals in
response to the questions contained in Part III – Compensation Practices, of the
questionnaire. In addition, the Final Report summarizes the results of the 20
examinations that addressed certain executive compensation issues. See
Section VII, below.
I. Form 990, Schedule H, Hospitals
The Final Report describes the final Form 990, Schedule H, Hospitals, effective
for 2008 and later tax years, and explains how that schedule addresses many of
the reporting concerns in this study. See Section VIII, below.
15

III. BACKGROUND ON U.S. HOSPITALS AND PRIOR STUDIES
A. Background on U.S. Hospitals
According to the American Hospital Association (AHA), there are 5,708
registered hospitals in the United States.
6
These include 4,897 community
hospitals, which are defined as all nonfederal, short-term general, and other
special hospitals (obstetrics and gynecology; eye, ear, nose, and throat;
rehabilitation; orthopedic; and other individually described specialty services).
7
The community hospitals include the following:
• 2,913 nongovernment nonprofit community hospitals (59% of community
hospitals)
• 873 investor-owned for-profit community hospitals (18% of community
hospitals)
• 1,111 state and local government community hospitals (23% of community
hospitals).
8
AHA reports 1,997 rural community hospitals (41%) and 2,900 urban community
hospitals (59%).
9
In its 2006 report on community benefit, the Congressional
Budget Office reported that 51% of nonprofit hospitals were in large urban areas,
34% were in small urban or suburban areas, and 14% were in rural areas.
10
According to the Congressional Budget Office, the distribution of hospitals across
nonprofits, for-profits and government hospitals “varies markedly by region. In
the Northeast, 89 percent of the hospitals are nonprofits, whereas in the South
only 43 percent of the hospitals are nonprofits. For-profit hospitals are common
in the South and West, but not in the Northeast and Midwest.”
11
This is
consistent with the 2005 GAO report, which reported that “states in the Northeast
6
http://www.aha.org/aha/resource-center/Statistics-and-Studies/fast-facts.html (Fast Facts on US
Hospitals). The information from AHA’s web site was as last updated on November 7, 2008. For
this purpose, a registered hospital is a hospital that satisfies AHA’s criteria for registration as a
hospital facility, including both AHA member hospitals and nonmember hospitals.
7
The remaining 811 non-community hospitals include federal government hospitals, nonfederal
psychiatric hospitals, nonfederal long term care hospitals, prison hospitals, college infirmaries,
and other facilities.
8
This breakdown is similar to that reported by the Congressional Budget Office (CBO) in 2006:
nonprofit hospitals (58%), for-profit hospitals (18%), and government hospitals (24%).
Congressional Budget Office, “Nonprofit Hospitals and the Provision of Community Benefits,”
December 2006, pages 12-13 (Tables 2 and 3). It is also similar to the breakdown reported in
the 2005 United States Government Accountability Office (GAO) report, “Nonprofit, For-Profit,
and Government Hospitals, Uncompensated Care and Other Community Benefits,” May 2005,
page 4 (nonprofit hospitals – 62%, government hospitals – 20%, and for-profit hospitals – 18%).
9
The AHA fact sheet did not describe how the hospitals were classified as rural or urban.
10
Congressional Budget Office, “Nonprofit Hospitals and the Provision of Community Benefits,”
December 2006, page 13.
11
Id. at 12.
16

and Midwest had relatively high concentrations of nonprofit hospitals, whereas in
the South the concentration was relatively low.”
12
The 2006 CBO study also reported the following, based on data from 2003:
13
• Nonprofit hospitals tend to be larger than for-profit hospitals and are more
likely to be teaching hospitals
• Nonprofit hospitals have higher average total assets, fixed assets, net
patient revenues, and operating expenses than both for-profit and
government hospitals
• Nonprofit hospitals have a total margin (3.9%), measured as total
payments from all sources over all costs as a share of payments, that is
somewhat higher than government hospitals (2.9%) but lower than for-
profits (9.1%)
Critical Access Hospitals. The Medicare Rural Hospital Flexibility Program,
created by Congress in 1997, allows certain hospitals to be licensed as critical
access hospitals. Critical access hospitals generally must be located in a rural
area or in an area treated as rural, and satisfy certain specified requirements
allowing them to be designated as such.
14
Under federal law, critical access
hospitals differ from urban and other rural hospitals, both in terms of how they
are reimbursed under Medicare programs and in their organization and
operations.
As of September 2008, there were 1,294 critical access hospitals in 45 states
across the United States.
15
The five states with the greatest number of critical
access hospitals were Kansas (83), Iowa (82), Minnesota (79), Texas (74), and
Nebraska (65). Three heavily populated states – California (27), Florida (11),
and New York (13) – have fewer critical access hospitals. Five states –
Connecticut, Delaware, Maryland, New Jersey, and Rhode Island – did not
participate in federal programs required for critical access designation and did
not have any critical access hospitals in their states.
12
United States Government Accountability Office (GAO) report, “Nonprofit, For-Profit, and
Government Hospitals, Uncompensated Care and Other Community Benefits,” May 2005, page
4.
13
Congressional Budget Office, “Nonprofit Hospitals and the Provision of Community Benefits,”
December 2006, pages 12-14.
14
See Section II.C for a description of the requirements for critical access hospital designation.
15
www.flexmonitoring.org/cahlistRA.cgi (CAH Information). The information described here is as
reported by the Flex Monitoring Team, which consists of the Rural Health Research Centers at
the Universities of Minnesota, North Carolina at Chapel Hill, and Southern Maine. The team
members are recipients of a cooperative agreement award from the Federal Office of Rural
Health Policy to monitor and evaluate the Medicare Rural Hospital Flexibility Program. The
monitoring project assesses the impact of the flexibility program on rural hospitals and
communities and the role of states in achieving overall program objectives, including improving
access to and the quality of health care services; improving the financial performance of critical
access hospitals; and engaging rural communities in health care system development.
17

Unlike other hospitals which are reimbursed under the Medicare prospective
payment system, critical access hospitals receive cost-based reimbursement for
inpatient and outpatient care. These differences may affect financial
performance, and the incentives, financial management, and utilization practices
under the two Medicare payment methods may differ substantially.
16
The Flex Monitoring Team (see footnote 15 for an explanation of the Flex
Monitoring Team) reviews 20 financial indicators in six domains – profitability,
liquidity, capital structure, revenue, cost, and utilization – and prepares annual
reports regarding these indicators for critical access hospitals across the United
States. For example, in its August 2008 report (for 2006), the team reported a
“total margin” (net income divided by total revenue) of 3.6% for critical access
hospitals across the United States;
17
the total margin reported in the team’s
August 2007 report (for 2005) was 2.6%.
18
Profitability varied materially across
the states – for 2005, critical access hospitals in 7 states had aggregate negative
“total margins” and 4 states reported total margins exceeding 5% of total
revenue.
19
For 2006, 4 states reported aggregate negative total margins, and 14
states reported total margins exceeding 5% of total revenue.
20
The Flex
Monitoring Team reports demonstrate that financial performance for critical
access hospitals varies considerably across the various states.
B. Other Studies on Community Benefit Provided by Nonprofit Hospitals
Other recent studies have explored community benefit reporting by nonprofit and
other hospitals. These studies include a 2006 study by the Congressional
Budget Office,
21
and two separate studies by the Government Accountability
Office – one in 2005
22
and the other in 2008.
23
As described below, these
studies generally found that community benefit reporting varied by type of
hospital, and that uncompensated care and community benefit expenditures
often were concentrated in a relatively small number of hospitals, whether
nonprofit, for-profit, or government hospitals.
2005 GAO Report
. In May 2005, the GAO issued a report to the Committee on
Ways and Means, House of Representatives of the United States Congress,
16
Flex Monitoring Team Data Summary Report No. 5, “CAH Financial Indicators Report:
Summary of Indicator Medians by State,” August 2008, page 2.
17
Id. at 4.
18
Flex Monitoring Team Data Summary Report No. 4, “CAH Financial Indicators Report:
Summary of Indicator Medians by State,” August 2007, page 4.
19
Id.
20
Flex Monitoring Team Data Summary Report No. 5, “CAH Financial Indicators Report:
Summary of Indicator Medians by State,” August 2008, page 4.
21
Congressional Budget Office, “Nonprofit Hospitals and the Provision of Community Benefits,”
December 2006.
22
United States Government Accountability Office (GAO) report, “Nonprofit, For-Profit, and
Government Hospitals, Uncompensated Care and Other Community Benefits,” May 2005.
23
United States Government Accountability Office (GAO) report, “Nonprofit Hospitals, Variation in
Standards and Guidance Limits Comparison of How Hospitals Meet Community Benefit
Requirements,” September 2008.
18

regarding uncompensated care and other community benefits provided by
nonprofit, for-profit and government hospitals. The study looked at data from 5
states – California, Florida, Georgia, Indiana, and Texas. The study defined
community benefits to include uncompensated care as well as services such as
the provision of health education and medical research. GAO found that
government hospitals generally devoted substantially larger shares of their
patient operating expenses to uncompensated care (defined to include charity
care and bad debt) than did nonprofit and for-profit hospitals.
24
Further, within
each group, the burden of uncompensated care costs was not evenly distributed
among hospitals but instead was concentrated in a small number of hospitals,
meaning that a small number of nonprofit hospitals accounted for substantially
more of the uncompensated care than did other nonprofit hospitals.
25
For all
three groups, the top quarter of hospitals devoted substantially greater
percentages of their patient operating expenses to uncompensated care, on
average, compared with the bottom quarter of hospitals.
26
2006 Congressional Budget Office Report. This study measured the provision of
certain community benefits and compared nonprofit hospitals with for-profit
hospitals. It also examined the provision of community benefits by nonfederal
government hospitals.
The 2006 CBO Report found that although nonprofit hospitals must provide
community benefits in order to receive tax exemptions, there is little consensus
on what constitutes a community benefit or how to measure such benefits.
27
CBO found that, on average, nonprofit hospitals provided higher levels of
uncompensated care (for purposes of this study, the sum of charity care and bad
debt) than did otherwise similar for-profit hospitals, but that among individual
hospitals, the provision of uncompensated care varied widely.
28
Uncompensated
care as a share of hospitals’ operating expenses was much higher at government
hospitals (13.0%) than at either nonprofit hospitals (4.7%) or for-profit hospitals
(4.2%).
29
CBO also found that nonprofit hospitals were more likely than for-profit hospitals
to provide certain specialized services that have been identified by certain
24
United States Government Accountability Office (GAO) report, “Nonprofit, For-Profit, and
Government Hospitals, Uncompensated Care and Other Community Benefits,” May 2005 (What
GAO Found).
25
Id.
26
Id. at 13-14.
27
Congressional Budget Office, “Nonprofit Hospitals and the Provision of Community Benefits,”
December 2006, page 1.
28
Id. at 1-2. CBO observed that uncompensated care, when measured by including bad debt,
has “substantial limitations” as a measure of community benefits, as it does not distinguish
between the provision of charity care for the indigent and bad debt. Id. at 9.
29
Id. at 2.
19

researchers as being generally unprofitable, including emergency room care,
labor and delivery services, burn intensive care, and high-level trauma care.
30
2008 GAO Report. In September 2008, the GAO issued its Report to the
Ranking Member, Committee on Finance, U.S. Senate, regarding community
benefit reporting by nonprofit hospitals.
31
In this study, GAO analyzed federal
and state laws; the standards and guidance from federal agencies and industry
groups; and 2006 data from California, Indiana, Massachusetts, and Texas.
GAO found that the IRS’s community benefit standard allows nonprofit hospitals
broad latitude to determine the services and activities that constitute community
benefit, and that state community benefit requirements that hospitals must meet
to qualify for state tax-exempt or nonprofit status vary substantially in scope and
detail.
32
GAO found that variations in the activities nonprofit hospitals define as
community benefit lead to substantial differences in the amount of community
benefits they report, and that nonprofit hospitals measure costs of these activities
differently, which can lead to inconsistencies in reported community benefits.
33
C. Study on Executive Compensation of Nonprofit Hospitals
2006 GAO Nonprofit Hospital System Survey on Executive Compensation
Policies and Practices. In response to a request by the House Ways and Means
Committee, the GAO surveyed executive compensation issues at selected
private, nonprofit hospital systems to gain an understanding of the policies and
practices related to the salaries, benefits, travel, gifts and entertainment
expenses paid by these hospital systems.
34
The study’s key questions were as
follows:
• What corporate governance structure do selected hospital systems report
as having in place over executive compensation?
• What is the basis for the compensation and benefits earned by, awarded
to, or paid to the executives as reported by selected hospital systems?
• What internal controls do selected hospital systems report as having in
place over the approval, payment, and monitoring of executive travel and
entertainment expenses, gifts, and other perquisites?
35
The GAO found that the hospital systems reported similarities in certain
governance and compensation policies and practices, such as:
30
Id. at 3, 20.
31
United States Government Accountability Office (GAO) report, “Nonprofit Hospitals, Variation in
Standards and Guidance Limits Comparison of How Hospitals Meet Community Benefit
Requirements,” September 2008.
32
Id. (see What GAO Found).
33
Id.
34
United States Government Accountability Office, Nonprofit Hospital Systems, Survey on
Executive Compensation Policies and Practices, June 2006.
35
Id. at 1.
20

• having an executive compensation committee or entire board with primary
responsibility for approving executives’ base salary, bonuses, and
perquisites;
• having a conflict of interest policy that covers members of the executive
compensation committee and compensation consultants; and
• relying upon comparable market data of total compensation and benefits
prior to making compensation determinations.
36
The GAO found, however, that the hospital systems reported a range of practices
with respect to entertainment, travel expenses, payment for perquisites such as
memberships in recreational and social clubs, and audits of perquisites and
entertainment expenses.
37
36
Id. at 2.
37
Id.
21
IV. DEMOGRAPHICS - PATIENT MIX, REVENUES, EXCESS REVENUES
This section provides demographic information for the hospitals included in the
study. Section IV.A reports insurance coverage based on questionnaire
responses. Section IV.B summarizes basic financial information (by revenue
size) of the hospitals that reported revenues and expenses for their Form 990.
Section IV.C provides financial information by community type. Section IV.D
describes the demographic overlap of the community type and revenue size
categories. Section IV.E provides a further breakdown by excess revenue
categories.
A. Patient Insurance Coverage
Based on 480 responses, the average percentage of patients with no insurance
was 8%, with private insurance was 43%, with Medicare was 31%, with Medicaid
was 15%, and with some other form of public insurance was 3%. Figure 1,
below, displays the breakdown.
Figure 1. Average Percentage of Insurance Coverage
43%
31%
15%
8%
3%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
Private
Insurance
(n=475)
Medicare
(n=474)
Medicaid
(n=474)
Other Public
Insurance
(n=331)
Self Pay
(n=475)
Insurance Type
Average Percentage of Patients
B. Revenues and Excess Revenues By Revenue Size
This section classifies the hospitals into five revenue categories, and reports
revenue, expense, and excess revenue information for these categories. Key
findings of this section include the following:
22

1. The average and median total revenue amounts were $179 million and
$89 million, respectively. The average and median excess revenue
amounts were $8.3 million and $2.5 million, respectively.
2. The largest hospitals reported a disproportionately large percentage of
aggregate total revenues. 7% of all hospitals (those with revenues over
$500 million) reported 40% of aggregate total revenues.
3. Overall, excess revenues as a percentage of total revenues was 4.6%.
Excess revenues as a percentage of total revenues was lowest for the
group of hospitals with revenues under $25 million (3.3%), and increased
with revenue size. Each revenue size category reported an aggregate
excess revenue amount, as well as average and median excess revenue
amounts, greater than zero.
4. 79% of all hospitals reported excess revenues. 39% reported excess
revenues as a percentage of total revenues in the 0% to 5% range. 40%
reported excess revenues as a percentage of total revenues in the over
5% range.
5. 21% of the overall group reported a deficit (total expenses greater than
total revenues) or zero excess revenues. The percentage of hospitals
reporting a deficit or zero excess revenues was greatest for the group of
smallest hospitals (35%) and decreased with revenue size.
The aggregate annual revenues reported on Form 990 by the 488 hospitals was
$87.5 billion. A relatively small number of larger hospitals reported a
disproportionately large portion of the overall reported revenues.
Figure 2, below, shows the distribution of hospitals by annual revenues and
compares the percentages of hospitals in each revenue size group to the
percentages of aggregate revenues reported by each group.
Figure 2. Distribution of Hospitals by Aggregate Annual Revenues
Respondent Profile
Aggregate Reported
Revenue
Annual Revenues
#
% of all
hospitals
$Billion
% of
aggregate
revenue
Under $25M 85 17% $1.2 1%
$25M to under $100M 173 36% $9.8 11%
$100M to under $250M 133 27% $21.0 24%
$250M to under $500M 61 13% $20.8 24%
$500M and over 36 7% $34.7 40%
Total 488 100% $87.5 100%
23

The smallest revenue size comprised 17% of the hospitals, but only 1% of the
aggregate reported revenues. The largest group comprised 40% of aggregate
revenues even though it comprised only 7% of the total number of hospitals.
Figure 3, below, displays total annual revenues, total expenses, and the
excess/deficit revenues (difference between total revenues and total expenses)
as reported on Form 990 for each category. Separate charts are provided below
for total revenues and excess revenues.
Figure 3. Annual Total Revenues, Total Expenses, and Excess/Deficit Revenue by
Revenue Size
Annual Total Revenues Annual Total Expenses Annual Excess/Deficit Revenue
Revenue Size
Aggregate Average Median Aggregate Average Median Aggregate Average Median
(Billion $) (Million $) (Million $) (Billion $) (Million $) (Million $) (Million $) (Million $) (Million $)
Under $25M
(N = 85)
1.224 14.4 15.2 1.184 13.9 15.0 40.6 0.5 0.3
$25M - Under
$100M (N = 173)
9.795 56.6 56.2 9.425 54.5 52.8 370.2 2.1 1.7
$100M - Under
$250M (N = 133)
20.985 157.8 152.2 20.184 151.8 146.9 801.0 6.0 4.9
$250M – Under
$500M (N = 61)
20.829 341.5 330.2 19.903 326.3 310.9 925.9 15.2 16.2
$500M and
Over (N = 36)
34.690 963.6 734.7 32.769 910.3 698.6 1,920.9 53.4 38.3
Overall (N = 488) 87.523 179.4 89.4 83.464 171.0 87.1 4,058.5 8.3 2.5
The average total annual revenue, as reported on the respondents’ Forms 990,
Line 12, was $179 million, and the median was $89 million. Each revenue size
category reported positive numbers for average and median excess revenues.
The charts below display the average and median total revenues and excess
revenue by revenue size category.
24

Figure 4. Average and Median of Annual Total Revenues by Revenue Size
14.4
5
6
.
6
157
.
8
341
.
5
963.
6
1
7
9
.
4
1
5
.2
5
6
.
2
15
2
.
2
3
3
0
.
2
734.7
89.4
0
100
200
300
400
500
600
700
800
900
1,000
1,100
Under $25M (N =
85)
$25M - Under
$100M (N = 173)
$100M - Under
$250M (N = 133)
$250M - Under
$500M (N = 61)
$500M and Over
(N = 36)
All (N = 488)
Revenue Size
Average & Median of Annual Total Revenues (in $ Million)
Average Median
In general, the average and median amounts are relatively close within each of
the different groups. The difference between the average and median for
hospitals with revenues of $500 million and over, however, varies more than for
the others. This indicates that some relatively large hospitals have total
revenues that are much higher than the median total revenues for the $500
million and over group.
25

Figure 5. Average and Median of Annual Excess Revenue
by Revenue Size
0
.
5
2.1
6.
0
1
5.
2
53.4
8.3
0.
3
1.7
4
.
9
1
6.
2
3
8.
3
2
.5
0
10
20
30
40
50
60
Under $25M (N
= 85)
$25M - Under
$100M (N = 173)
$100M - Under
$250M (N = 133)
$250M - Under
$500M (N = 61)
$500M and
Over (N = 36)
All (N = 488)
Revenue Size
Average & Median of Annual Excess Revenue (in $ Million)
Average Median
Figure 6, below, shows the reported aggregate excess revenues as a percentage
of aggregate total revenues for each revenue size category and overall. These
calculations are based on aggregate amounts reported in Figure 3 above. For
example, the overall 4.6% figure represents $4.1 billion of aggregate excess
revenues divided by $87.5 billion of aggregate total revenues.
26

Figure 6. Excess Revenue as a Percentage of Total Revenue
Revenue Size Excess revenue as a percentage of
total revenue
Under $25 million (N = 85) 3.3%
$25 million to $100 million (N = 173) 3.8%
$100 million to $250 million (N = 133) 3.8%
$250 million to $500 million (N = 61) 4.4%
Over $500 million (N = 36) 5.5%
Total (N = 488) 4.6%
The aggregate excess revenue as a percentage of aggregate total revenue
generally increased across the categories, from a low of 3.3% for the under $25
million category to a high of 5.5% for the over $500 million category. The overall
average was 4.6%.
Figure 7, below, shows the distribution of negative/positive excess revenues as a
percentage of revenues.
Figure 7. Distribution of Excess Revenue as a Percentage of Annual Total Revenue by
Revenue Size
Excess Revenues as Percentage of Total Revenues Range
All
0% or Negative
Positive to <
2.5%
2.5% - < 5% 5% - < 10% 10% & Over
% of all % of % of % of % of % of
hospitals revenue revenue revenue revenue revenue
Revenue Size
N
N
size
N
size
N
size
N
size
N
size
Under $25M 85 17 30 35 13 15 11 13 19 22 12 14
$25M - Under
$100M
173 36 39 23 29 17 41 24 43 25 21 12
$100M - Under
$250M
133 27 25 19 30 23 29 22 39 29 10 8
$250M and
Over
97 20 10 10 19 20 18 19 40 41 10 10
All 488 100 104 21 91 19 99 20 141 29 53 11
Figure 7, above, shows that overall 21% of the hospitals reported total expenses
greater or equal to total revenues, and 39% of the hospitals reported excess
revenues as a percentage of total revenues in the range of greater than 0% to
5%. 40% of all hospitals reported excess revenues as a percentage of total
revenues of at least 5%; 11% reported excess revenues of at least 10% of total
revenues.
The percentage of hospitals reporting a deficit or zero excess revenue decreased
as revenue size increased. The $500 million and over revenue size had the
smallest percentage of hospitals reporting zero or a deficit.
38
38
The two largest revenue sizes were combined to prevent potential identification of respondent
hospitals.
27

C. Revenues and Excess Revenues by Community Type
This section classifies the hospitals into four community types, and reports
revenue, expense, and excess revenue information for these categories. Key
findings of this section include the following:
1. Rural hospitals generally reported smaller total revenues and excess
revenues than did other community types. The rural community types had
a disproportionately small percentage of aggregate total revenues (30% of
the hospitals, 10% of aggregate revenues), while the high population
community type had a disproportionately large percentage of aggregate
revenues (19% of hospitals, 41% of aggregate revenues).
2. Each community type reported aggregate excess revenues and average
and median excess revenues as a percentage of total revenues greater
than zero. CAHs reported the smallest average and median total
revenues ($29 million and $20 million, respectively) and the smallest
average and median excess revenue amounts ($1.0 million and $0.5
million, respectively). High population hospitals reported the largest
average and median amounts, both for total revenues ($389 million and
$196 million, respectively) and for excess revenues ($17.5 million and
$4.2 million, respectively).
3. CAHs reported the smallest percentage of excess revenues as a
percentage of total revenues (3.5%); rural (non-CAH) hospitals reported
the largest percentage (6.0%). 34% of CAHs reported a deficit (total
expenses greater than total revenues) or zero excess revenue compared
to 13% for rural (non-CAH) hospitals and 21% overall.
The table below shows the distribution of hospitals and aggregate total revenues
by community types.
Figure 8. Distribution of Hospitals and Total Revenues by Community Type
Respondent Profile
Aggregate Reported
Revenue
Community Type
# % $Billion %
High Population 93 19% $36.2 41%
Rural – CAH 68 14% $2.0 2%
Rural – Non CAH 78 16% $7.3 8%
Other 249 51% $42.1 48%
Total 488 100% $87.5 100%
The rural community types had a disproportionately small percentage of
aggregate total revenues while the high population community type had a
disproportionately large percentage of aggregate revenues. The other urban and
suburban category comprised approximately half of the number of hospitals and
overall reported total revenues.
28

Figure 9, below, includes the aggregate, average and median total revenues,
total expenses, and excess of revenues over expenses by community type.
Figure 10 and Figure 11 display total revenues and excess revenues by
community type.
Figure 9. Annual Total Revenues, Total Expenses, and Excess/Deficit Revenue
by Community Type
Annual Total Revenues Annual Total Expenses Annual Excess/Deficit Revenue
Aggregate
Average Median
Aggregate
Average Median
Aggregate
Average Median
Community
Types
(Billion $) (Million $) (Million $) (Billion $) (Million $) (Million $) (Million $) (Million $) (Million $)
High
Population
(N = 93)
36.184 389.1 195.8 34.557 371.6 196.7 1,627.5 17.5 4.2
Rural - CAH
(N = 68)
1.965 28.9 19.6 1.896 27.9 19.3 69.3 1.0 0.5
Rural - Non
CAH
(N = 78)
7.256 93.0 67.7 6.823 87.5 64.8 433.3 5.6 3.4
Others
(N = 249)
42.117 169.1 113.9 40.189 161.4 109.7 1,928.4 7.7 3.1
Overall 87.523 179.4 89.4 83.464 171.0 87.1 4,058.5 8.3 2.5
29

Figure 10. Average and Median Annual Total Revenue by Community Type
389.1
28.9
93.0
169.1
179.4
195.8
19.6
67.7
113.9
89.4
0
50
100
150
200
250
300
350
400
450
High Population
(N = 93)
CAH (N = 68) Rural - Non CAH
(N = 78)
Others (N = 249) All (N = 488)
Community Type
Average & Median of Annual Total Revenues (in $ Million)
Average Median
The CAHs reported the smallest average and median revenue amounts of any
community type. The average annual total revenue for hospitals in the high
population group is more than double the average annual total revenue for
hospitals in the other urban and suburban category, the next largest group, and
more than double the average annual total revenue for the entire group of
hospitals.
The high population group shows the largest difference between average
revenue and median revenue. This deviation indicates that there are a number
of extremely large hospitals (relative to the others in the group) located in high
population areas.
30

Figure 11. Average and Median Annual Excess Revenue by Community Type
17. 5
1.0
5.6
7.7
8.3
4.2
0.5
3.4
3.1
2.5
0
2
4
6
8
10
12
14
16
18
20
High Population
(N = 93)
CAH (N = 68) Rural - Non CAH
(N = 78)
Others (N = 249) All (N = 488)
Community Type
Average & Median of Annual Excess Revenue (in $ Million)
Average Median
31

As was the case with total revenues, the greatest variation between average and
median excess revenue amounts was with the high population group.
The table below shows the reported excess revenues as a percentage of total
revenues for each community type. These calculations are based on aggregate
amounts reported in Figure 9, above. For example, the overall 4.6% figure
represents $4.1 billion of aggregate excess revenues divided by $87.5 billion of
aggregate total revenues.
Figure 12. Excess Revenue as a Percentage
of Total Revenue by Community Type
Community Type Excess revenues as a percentage
of total revenue
High population (N = 93) 4.5%
Rural - CAH (N = 68) 3.5%
Rural - Non CAH (N = 78) 6.0%
Others (N = 249) 4.6%
All 488 hospitals 4.6%
The overall measure of excess revenues as a percentage of total revenues was
4.6%. All four community types reported revenues greater than expenses for the
year. The CAH community type reported the smallest percentage of excess
revenues as a percentage of total revenues (3.5%) and rural (non-CAH) hospitals
reported the largest percentage (6%). High population and other urban and
suburban hospitals were approximately at the overall percentage.
Figure 13, below, shows the distribution of negative/positive excess revenues as
a percentage of revenues by community type.
Figure 13. Distribution of Excess Revenues as a Percentage of Annual Total Revenue
by Community Type
Excess Revenue as Percentage of Revenue Range
All
0% or Negative Positive to < 2.5% 2.5% - < 5% 5% - < 10% 10% & Over
Community
Type
N
% of all
hospitals
N
% of
community
type
N
% of
community
type
N
% of
community
type
N
% of
community
type
N
% of
community
type
High
Population
93 19 20 22 24 26 20 22 21 23 8 9
CAH 68 14 23 34 7 10 15 22 17 25 6 9
Rural -
Non CAH
78 16 10 13 12 15 11 14 32 41 13 17
Others 249 51 51 20 48 19 53 21 71 29 26 10
All 488 100 104 21 91 19 99 20 141 29 53 11
CAHs reported the largest percentage of hospitals with a deficit or zero excess
revenues, and other rural hospitals reported the smallest.
32
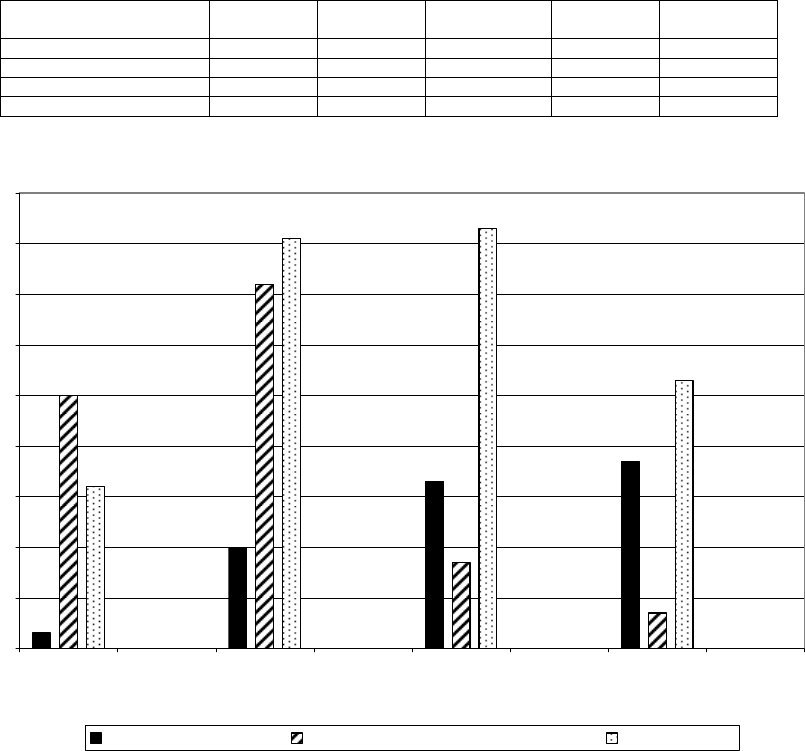
D. Relationship between Community Type and Revenue Size
The figures below show the overlap of community type and revenue size within
the respondent hospitals. For example, in Figure 15, the middle vertical bar in
the under $25 million revenue size shows there are 50 rural hospitals (CAH and
non-CAH) under $25 million in revenue size. Figure 15 shows the distribution of
community types across the revenue size categories, and Figure 16 shows the
distribution of revenue size across community types.
Figure 14. Number of Hospitals by Revenue Size and Community Type
Under $25
million
$25 -$100
million
$100 - $250
million
Over $250
million
Total
High Population 3 20 33 37 93
CAH/Rural Non-CAH 50 72 17 7 146
Other 32 81 83 53 249
Total 85 173 133 97 488
Figure 15. Number of Hospitals by Community Type and Revenue Size
3
20
33
37
50
72
17
7
32
81
83
53
0
10
20
30
40
50
60
70
80
90
Under $25M
(n=85)
$25M under
$100M (n=173)
$100M under
$250M (n=133)
Over $250M
(n=97)
Revenue Size
Number of Hospitals
High Population(n=93) Critical Access/Rural Non-CAH (146) Other (n=249)
33

Figure 16. Number of Hospitals by Revenue Size and Community Type
3
50
32
20
72
81
33
17
83
37
7
53
0
10
20
30
40
50
60
70
80
90
High Population(n=93) Critical Access/Rural Non-
CAH (n=146)
Other (n=249)
Community Type
Number of Hospitals
Under $25M (n=85) $25M under $100M (n=173)
$100M under $250M (n=133) Over $250M (n=97)
As might be expected, there generally was a strong correlation between
community type and revenue size. Most rural hospitals (84%) reported total
revenues under $100 million. 75% of high population hospitals reported total
revenues over $100 million, and high population hospitals constituted 58% of
these reporting total revenues over $500 million.
39
More than 20% of high
population hospitals and more than 5% of other urban and suburban hospitals
were in the over $500 million revenue size. More than 55% of CAHs were in the
lowest revenue size.
E. Groupings by Excess Revenues
The previous sections reported revenues and excess revenues based on
revenue size and community type categories. This section classifies the 488
hospitals into five categories based on the amounts of the excess revenues over
expenses reported on the Forms 990. Overall, the hospitals reported $4.1 billion
of excess revenues. Figure 17, below, shows the distribution of hospitals and
aggregate excess revenues by these five excess revenue categories.
39
The two groups of rural hospitals and the two largest revenue sizes were combined in the
figures to prevent potential identification of respondent hospitals.
34

Figure 17. Distribution of Hospitals and Aggregate Excess Revenue
by Excess Revenue Size
Respondent Profile
Aggregate Reported Excess
Revenue
Annual Excess Revenues
# % $M %
$0 or under 104 21% $-373 -9%
$1 to under $2.5M 138 28% $158 4%
$2.5M to under $7.5M 109 22% $484 12%
$7.5M to under $15M 60 12% $647 16%
$15 M and over 77 16% $3,143 77%
Total 488 100% $4,059 100%
The table shows the bulk of reported excess revenues was reported by a
relatively small group of hospitals. The group of hospitals reporting $15 million or
more of excess revenues comprised 16% of the hospitals, but reported 77% of
the aggregate excess revenues.
The table below displays total revenues, total expenses, and the excess/deficit
revenues for each excess revenue category listed above. Figure 19 and Figure
20 display total revenues and excess revenues by excess revenue category.
Figure 18. Annual Total Revenues, Total Expenses, and Excess/Deficit Revenues by
Excess Revenue Size
Annual Total Revenues Annual Total Expenses Annual Excess/Deficit Revenue
Excess Revenue
Size
Aggregate Average Median Aggregate Average Median Aggregate Average Median
(Billion $) (Million $) (Million $) (Billion $) (Million $) (Million $) (Million $) (Million $) (Million $)
$0 or Under
(N = 104)
10.525 101.2 57.1 10.898 104.8 59.5 -373.3 -3.6 -1.6
$1 - Under $2.5M
(N = 138)
7.543 54.7 32.5 7.385 53.5 32.0 158.3 1.1 1.2
$2.5M - Under
$7.5M (N = 109)
13.389 122.8 83.3 12.905 118.4 76.9 484.1 4.4 4.0
$7.5M - Under
$15M (N = 60)
12.798 213.3 178.8 12.151 202.5 168.7 646.6 10.8 10.8
$15M or Over
(N = 77)
43.268 561.9 386.7 40.126 521.1 357.2 3,142.9 40.8 29.5
Overall (N=488) 87.523 179.4 89.4 83.464 171.0 87.1 4,058.5 8.3 2.5
35
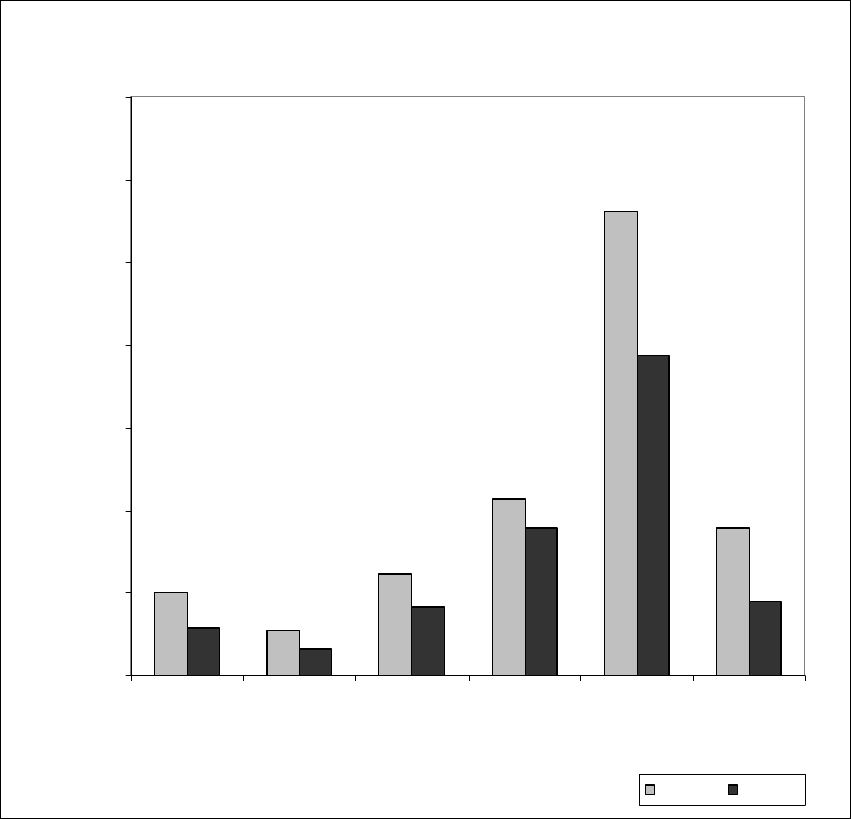
Figure 19. Average and Median Annual Total Revenue by Excess Revenue Size
1
01.2
54.7
12
2.
8
213.3
561.9
179
.
4
57
.
1
3
2.
5
83
.
3
178
.
8
386.7
89
.
4
0
100
200
300
400
500
600
700
$0 or Under
(N = 104)
$1 - Under
$2.5M (N =
138)
$2.5M -
Under $7.5M
(N = 109)
$7.5M -
Under $15M
(N = 60)
$15M or Over
(N = 77)
All (N = 488)
Excess Revenue Size
Average & Median of Annual Total Revenues (in $ Million)
Average Median
36

Figure 20. Average and Median Annual Excess Revenue by Excess Revenue Size
-3.6
1.1
4.4
10.8
40.8
8.3
-1.6
1.2
4.0
10.8
29.5
2.5
-4
6
16
26
36
46
$0 or Under
(N = 104)
$1 - Under
$2.5M (N =
138)
$2.5M - Under
$7.5M (N =
109)
$7.5M - Under
$15M (N = 60)
$15M or Over
(N = 77)
All (N = 488)
Excess Revenue Size
Avearge & Median of Annual Excess Revenue (in $ Million)
Average Median
Figure 19 shows that hospitals with deficits or the smallest excess revenues
tended to be those with lower total revenues (under $123 million average, under
$83 million median).
Figure 21, below, shows the distribution of negative/positive excess revenues as
a percentage of annual revenues by excess revenue sizes.
37

Figure 21. Distribution of Excess Revenue as a Percentage of Annual Total Revenue
by Excess Revenue Size
Excess Revenue as a Percentage of Annual Revenue Range
All
0% or
Negative
Positive to < 5% 5% - < 10% 10% or Over
% of all % of % of % of % of
hospitals revenue revenue revenue revenue
Excess Revenue Size
N
N
size
N
size
N
size
N
size
Negative & 0 104 21 104 100 0 - 0 - 0 -
$1 - Under $2.5M 138 28 0 - 104 75 26 19 8 6
$2.5M - Under $7.5M 109 22 0 - 55 51 40 37 14 13
$7.5M - Under $15M 60 12 0 - 20 33 29 48 11 18
$15M or Over 77 16 0 - 11 14 46 60 20 26
All 488 100 104 21 190 39 141 29 53 11
Most of the hospitals in the $1 to under $7.5 million ranges (64%) reported
excess revenues under 5% of total revenues. Most of the hospitals in the $7.5
million or over ranges (55%) reported excess revenues in the 5% to under 10%
level.
38

V. DIFFERENCES IN COMMUNITY BENEFIT REPORTING ACROSS
CERTAIN DEMOGRAPHICS - COMMUNITY TYPES, REVENUE SIZE
A. Introduction
The respondent hospitals were classified into two different demographic groups –
community types and revenue size. The distribution of the respondent hospitals
across these two groups is as follows.
Community types:
• “High population” – 94 hospitals (19%)
• “Other urban and suburban” – 249 hospitals (51%)
• “Critical access hospitals (CAH)” – 68 hospitals (14%)
• “Rural (non-CAH)” – 78 hospitals (16%)
Revenue size:
• Under $25 million – 85 hospitals (17%)
• $25 million to $100 million – 173 hospitals (36%)
• $100 million to $250 million – 133 hospitals (27%)
• $250 million to $500 million – 61 hospitals (13%)
• Over $500 million – 36 hospitals (7%)
Section V.B provides breakdowns by community type, and Section V.C provides
breakdowns by revenue size, for aggregate community benefit expenditures,
uncompensated care, medical education and training, medical research, and
community programs.
B. Comparison of Certain Information by Community Type
40
1. Summary of Key Findings – Community Type
a. The patient mix for each community type generally followed that for the
overall group – in descending order, private insurance, Medicare,
Medicaid, uninsured, and other public programs. All community types
reported uninsured patients as 7% to 8% of total patients. CAHs
reported the highest percentage of Medicare patients (36% compared
to 31% overall), and high population hospitals reported the highest
percentage of Medicaid patients (19% compared to 15% overall).
b. Between 94% and 96% of each community type reported
uncompensated care expenditures. Although the percentage of
hospitals reporting they provided community benefit did not vary
materially across community types, there were some exceptions. Only
60% of CAHs reported providing medical education and training,
40
For a description of the community types, see Section II.C, above.
39
compared to 77% overall. 40% of the high population hospitals
reported medical research expenditures, compared to less than 5% of
rural hospitals (CAH and non-CAH).
c. The median percentage of patients reported as receiving
uncompensated care was 3% overall, ranging from 2% for rural
hospitals to 6% for high population hospitals. The median percentages
of patients reported as receiving uncompensated care were less than
the overall percentage of patients without insurance for each
community type. However, the average percentage of patients
receiving uncompensated care was greater than the percentage of
patients without insurance for the high population group (11%
compared to 8%), the other urban and suburban group (10%
compared to 8%), and the rural (non-CAH) group (8% compared to
7%).
d. The average and median percentages of total revenues reported as
spent on uncompensated care were 7% and 4%, respectively. CAHs
reported the lowest average (6%) and median (2%) percentages; high
population hospitals reported the highest average (8%) and median
(5%) percentages. The percentage of hospitals reporting
uncompensated care expenditures at 3% or less of total revenues
ranged from 33% for high population hospitals to 59% for CAHs. Over
half of the hospitals in each community type (58% overall) reported
uncompensated care expenditures at 5% or less of total revenues.
e. Uncompensated care represented the largest community benefit
expenditure overall (56%) and for each community type. However, the
percentage of overall community benefit expenditures reported as
spent on uncompensated care ranged from 42% for high population
hospitals to 77% for CAHs. The mix of community benefit
expenditures among uncompensated care, medical research, medical
education and training, and community programs varied considerably
across community types.
f. The average and median percentages of total revenue reported as
spent on medical research and on medical education and training
varied considerably across community types. CAHs as a group
consistently reported spending lower percentages of total revenues on
these expenditures than did all other community types. High
population hospitals as a group consistently reported spending higher
percentages of total revenues on these expenditures than did all other
community types.
g. There was considerable variation across the community types
regarding community program expenditures. CAHs reported spending
40

19% of overall community benefit expenditures on community
programs compared to a range of 5% to 7% for the other community
types. Each community type reported spending most of its community
program expenditures on improving access to health care and other
health care promotion.
h. The median percentages of total revenue reported as spent on
aggregate community benefit expenditures were 2.8% for CAHs, 3.2%
for rural (non-CAH) hospitals, 5.8% for other urban and suburban
hospitals, and 9.8% for high population hospitals. The same pattern
followed for average percentages of total revenue reported as spent on
aggregate community benefit expenditures: 6.3% for CAHs, 8.4% for
rural (non-CAH) hospitals, 8.9% for other urban and suburban
hospitals, and 12.7% for high population hospitals. The overall median
and average percentages were 5.5% and 9.2%, respectively.
i. 47% of all hospitals reported spending less than 5% of total revenues
on aggregate community benefit expenditures. These ranged from
32% for high population hospitals to 61% for CAHs. 46% of other
urban and suburban hospitals, and 57% of rural (non-CAH) hospitals,
reported spending less than 5% of total revenues on aggregate
community benefit expenditures.
2. Patient Mix (Based on Type of Insurance Coverage) by Community
Type
The table and charts below break down insurance coverage by community type
for the 480 hospitals that reported this information. Overall, the average
percentages reported by the hospitals were that 43% of their patients had private
insurance, 31% were covered by Medicare, 15% were covered by Medicaid, 3%
were covered by other public insurance programs, and 8% were uninsured.
41
41
According to the U.S. Census Bureau, the percentage of individuals without health insurance in
2005 was 15.3%. U.S. Census Bureau, Current Population Survey, 2006 Annual Social and
Economic Supplement (as revised March 2007).
41

Figure 22. Distribution of Health Insurance Coverage by Community Type*
Category of Health Insurance Coverage
Community Type
Private
Insurance
(%)
Medicare
(%)
Medicaid
(%)
Other
Public
Insurance
(%)
No
Health
Insurance
(%)
High Population 43.5% 27.7% 19.3% 3.9% 7.8%
Critical Access 38.2% 36.4% 12.7% 2.6% 8.1%
Rural - Non Critical Access 44.2% 32.8% 13.2% 3.0% 7.1%
Other Urban & Suburban 44.4% 30.2% 14.7% 2.5% 7.6%
All patients 43.3% 31.0% 15.1% 2.9% 7.7%
*Some hospitals reported total patient amounts that did not equal the total number of patients
reported in the various health insurance coverage categories.
Figure 23 and Figure 24, below, present the same health insurance coverage
information in two different ways. Figure 23 groups the community type
percentages for each type of coverage. Figure 24 shows the insurance coverage
mix within each community type.
Figure 23. Percentage of Patients with Insurance Coverage by Community Type,
by Type of Coverage
(n=480)
28%
19%
4%
36%
3%
8%
44%
33%
13%
3%
30%
15%
3%
8%
31%
3%
8%
44%
38%
13%
7%
44%
43%
15%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
Private
Insurance
Medicare Medicaid Other Public
Insurance
Uninsured
Types of Insurance
Percentage of Patients
High Population Critical Access Rural Non-CAH Other Total
42

Figure 24. Percentage of Patients with Insurance Coverage by Type,
by Community Type
(n=480)
44%
38%
44% 44%
43%
28%
36%
33%
30%
31%
19%
13% 13%
15% 15%
4%
3% 3% 3% 3%
8% 8%
7%
8% 8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
High
Population
Critical
Access
Rural Non-
CAH
Other Total
Community Type
Percentage of Patients
Private Insurance Medicare Medicaid Other Public Insurance Uninsured
The distribution of types of coverage across the community types is relatively
similar to the distribution of the entire respondent group. However, the hospitals
located in high population areas reported a smaller percentage of patients with
coverage through Medicare (28% vs. 31% overall) and a larger percentage of
patients with coverage through Medicaid (19% vs. 15% overall) compared with
the total group and each of the other community types. CAHs reported a smaller
percentage of patients with private insurance (38% vs. 43% overall) and a larger
percentage of patients with coverage through Medicare (36% vs. 31% overall)
compared with the overall group and each of the other community types. All
community types reported 7% to 8% of patients with no insurance coverage.
3. Number and Percentage of Hospitals Reporting Community
Benefit Expenditures, by Expenditure Type within Community Type
485 of the 489 (99%) hospitals reported community benefit expenditures in one
or more categories. Four hospitals did not report any expenditure amounts. This
section reports percentages based on the 485 hospitals that reported
expenditure amounts. Uncompensated care was the most commonly reported
community benefit expenditure category overall and for each community type.
Medical education and training was the next most common. Certain community
programs were also widely provided such as lectures and community based
43
education, newsletters and publications, medical screening, and improving
access to health care.
The table below shows the percentage of hospitals that reported the various
types of community benefit expenditures.
44
Figure 25. Number and Percentage of Hospitals Reporting Community Benefit
Expenditures by Expenditure Category and Community Type
Community Type
Category of High Population Critical Rural - Non Critical Other Aggregate
Community Hospitals Access Hospitals Access Hospitals Hospitals (N = 485)
Benefit
Expenditure
N % of all N % of all N % of all N % of all % of
hospitals in hospitals in hospitals in hospitals in N all
each category each category each category each category hospitals
▪ Uncompensated 90 96% 64 94% 75 96% 237 95% 466 95%
Care
▪ Medical, 81 86% 41 60% 56 72% 200 80% 378 77%
Education &
Training
▪ Medical
38 40% ** ** ** ** 60 24% 104 21%
Research
▪ Lectures, 67 71% 52 76% 66 85% 202 81% 387 79%
seminars &
education
▪ Medical 67 71% 52 76% 63 81% 195 78% 377 77%
screening
▪ Newsletter/ 71 76% 47 69% 64 82% 192 77% 374 76%
publications
▪ Improving 64 68% 30 44% 43 55% 136 55% 273 56%
access to
healthcare
▪ Immunization 41 44% 33 49% 35 45% 93 37% 202 41%
programs
▪ Other 33 35% 21 31% 30 38% 70 28% 154 31%
healthcare
promotion
▪ Studies on 30 32% 20 29% 14 18% 75 30% 139 28%
community's
unmet health-
care needs
Total CBE 100% 100% 100% 100% 100%
**To prevent potential identification of respondent hospitals, the CAH and non-CAH rural hospitals were combined in calculating the
number and percentage of hospitals reporting medical research expenditures. Within the combined rural hospitals category, 6
hospitals, 4%, reported research expenditures.
The percentage of hospitals reporting they provided specific types of community
benefit generally did not vary materially across the community types. There were
some exceptions. While 60% of CAHs reported providing medical education and
training, at least 72% of hospitals in all the other categories reported doing so. In
addition, 40% of hospitals in the high population group and 24% of hospitals in
45

the other urban and suburban category reported medical research expenditures,
while 4% of rural hospitals reported such expenditures.
4. Aggregate Uncompensated Care by Community Type
The aggregate uncompensated care expenditures reported by 466 hospitals as a
percentage of total revenues was 6.41%.
42
Uncompensated care expenditures
were not evenly distributed by the hospitals in the study, but were concentrated
in a relatively small number of hospitals. 14% of the hospitals reported 63% of
the aggregate uncompensated care expenditures; 26% of the hospitals reported
82% of the aggregate uncompensated care expenditures.
Percentage of patients. Figure 26 shows the reported average and median
percentages of patients receiving uncompensated care by the hospital’s
community type. The average and median percentages for the entire group were
9.8% and 3.4%, respectively.
Figure 26. Percentage of Patients Receiving Uncompensated Care
by Community Type
Community Type Number Average Median
of hospitals (%) (%)
High population 86 11.2 6.0
Rural – CAH 59 6.7 1.9
Rural - Non CAH 73 8.4 1.7
Others 225 10.4 4.7
Total 443 9.8 3.4
Note: This table includes only those hospitals that reported the
number of patients receiving uncompensated care.
Rural hospitals (CAH and non-CAH) reported lower average and median
percentages than the other community types and the overall group. High
population hospitals reported the highest average and median percentages of
patients receiving uncompensated care.
Percentage of revenues. Figure 27 and Figure 28 below show the average and
median percentages of total revenue reported as spent by 466 hospitals on
uncompensated care for each community type.
42
This reflects total reported uncompensated care expenditures divided by total reported
revenues for the entire group of 466 hospitals. This differs from the average and median
percentages of individual hospitals’ percentages reported below (e.g., Figure 27).
46

Figure 27. Percentage of Total Revenue Spent on Uncompensated Care
by Community Type
(Average and Medians)
(n=466)
Average Median
High Population
(n=90)
7.9% 4.8%
Critical Access
(n=64)
5.6% 2.1%
Rural Non-CAH
(n=75)
7.6% 2.7%
Other (n=237) 7.3% 4.3%
Total (n=466) 7.2% 3.9%
Figure 28. Percentage of Revenue Spent on Uncompensated Care
by Community Type
(Averages and Medians)
(n=466)
7.9%
7.6%
7.3%
7.2%
2.1%
4.3%
3.9%
5.6%
4.8%
2.7%
0.0%
1.0%
2.0%
3.0%
4.0%
5.0%
6.0%
7.0%
8.0%
9.0%
High
Population
(n=90) 96%*
Critical
Access
Hospital
(n=64) 94%*
Rural Non-
CAH(n=75)
96%*
Other (n=237)
95%*
Total (n=466)
95%*
Community Type
*Percentage of respondents reporting uncompensated care amounts
Percentage of Total Revenue Spent
Average Median
The median percentage of total revenue that was spent on uncompensated care
is 3.9% and the average is 7.2%. All of the averages are between 7% and 8%
with the exception of CAHs which reported an average of 5.6% of total revenue
spent on uncompensated care. The medians are lower than the averages in all
categories. This spread is widest in non-CAH rural hospitals where the average
is 7.6% and the median is 2.7%. The medians range from 2.1% for CAHs to
4.8% for high population hospitals.
47

Figure 29 through Figure 32 show the percentage of hospitals within each
community type that reported uncompensated care as a percentage of total
revenues within certain ranges.
Figure 29. Number and Percentage of Hospitals with Reported Uncompensated Care as a
Percentage of Total Revenue, by Community Type
Community Type
Uncompensated Care
High Critical Rural-Non Critical Other
Expenditure as
Percentage
Population Access Access Hospitals
Overall
of Total Revenues
N % N % N % N % N %
≤ 1%
7 8 20 31 19 25 41 17 87 19
Over 1% - ≤ 3% 23 26 18 28 20 27 51 22 112 24
Over 3% - ≤ 5% 17 19 5 8 10 13 39 16 71 15
Over 5% - ≤ 10% 19 21 9 14 12 16 59 25 99 21
> 10% 24 27 12 19 14 19 47 20 97 21
Total 90 100 64 100 75 100 237 100 466 100
Figure 30. Distribution of Hospitals by Community Type Based on Percentage of Total
Revenue Spent on Uncompensated Care
(Averages)
(n=466)
26%
19%
21%
27%
31%
28%
8%
14%
19%
13%
16%
19%
22%
16%
25%
20%
24%
8%
27%
25%
17%
21%
21%
15%
19%
0%
5%
10%
15%
20%
25%
30%
35%
0.0% - 1.0% 1.01% - 3.0% 3.01% - 5.0% 5.01% -
10.0%
Over 10.0%
Percentage of Total Revenue Spent
*Percentages in legend represent number of respondents in each Community Type reporting Uncompensated Care amounts
Percentage of Hospitals
High Population (n=90) 96%* Critical Access (n=64) 94%* Rural - Non-CAH(n=75) 96%*
Other (n=237) 95%* Total (n=466) 95%*
48

CAHs reported the highest percentage of hospitals in the low ranges (at or below
3%); high population hospitals reported the highest percentages of hospitals in
the high range (over 10%).
8% of hospitals in high population areas reported spending 1% or less of their
total revenue on uncompensated care while 31% of CAHs and 25% of non-CAH
rural hospitals reported doing so. In the 1% to 3% of total revenue range, all
categories of hospitals reported between 22% and 28%. High population and
other urban and suburban hospitals reported the highest percentage of
organizations in the 3% to 5% range, the 5% to 10% range, and the over 10%
range.
Figure 31. Distribution of Hospitals by Community Type Based on Percentage of Total
Revenue Spent on Uncompensated Care
(Averages)
(n=466)
31%
25%
17%
19%
26%
28%
27%
22%
24%
19%
8%
13%
16%
15%
21%
14%
16%
25%
27%
19% 19%
20%
21%
8%
21%
0%
5%
10%
15%
20%
25%
30%
35%
High
Population
(n=90) 96%*
Critical
Access (n=64)
94%*
Rural - Non-
CAH (n=75)
96%*
Other (n=237)
95%*
Total (n=466)
95%*
Community Type
* Percentage of respondents reporting Uncompensated Care amounts
Percentage of Hospitals
0.0% - 1.0% 1.01% - 3.0% 3.01% - 5.0% 5.01% - 10.0% Over 10.0%
While not shown in the chart above to prevent potential identification of
respondent hospitals, a small number of hospitals in each community type
reported spending over 50% of total revenues on community benefit
expenditures.
Figure 32, below, shows the percentage of hospitals (on a cumulative basis)
reporting uncompensated care expenditures at or less than specified percentage
of revenue levels.
49

Figure 32. Percentage of Hospitals Reporting Uncompensated Care Expenditures at or
Less Than Specified Percentage of Revenue Levels
Community Type ≤1% ≤3% ≤5% ≤10%
High population 8% 33% 52% 73%
CAHs 31% 59% 67% 81%
Rural (non-
CAHs)
25% 52% 65% 81%
Other 17% 39% 55% 80%
Total 19% 43% 58% 79%
As Figure 32 shows, between one half and two thirds of the hospitals in each
community type reported 5% or less of total revenues as spent on
uncompensated care. Over one half of the rural hospitals reported
uncompensated care expenditures of less than 3% of total revenues.
See Section VI.C.1, below, for an analysis of the reporting of various shortfalls
and bad debt as uncompensated care by community type.
5. Aggregate Medical Research Expenditures by Community Type
117 hospitals (24%) reported conducting medical research, but only 104 actually
reported medical research expenditure amounts. The aggregate medical
research expenditures reported by hospitals that reported such amounts was
3.48% of total revenues.
43
The average and median percentages of medical
research expenditures as a percentage of total revenues were 1.6% and 0.2%,
respectively.
A group of 15 hospitals reported 93% of the overall reported medical research
expenditures. See Section VI.B, below, for an analysis of community benefit
expenditures of this group.
Figure 33, below, shows the average and median percentages of total revenue
that hospitals reported as spent on medical research across the community
types. This chart includes only those 104 hospitals that reported an expenditure
amount for medical research.
43
This represents the total medical research expenditures divided by the total revenues for the
entire group of 104 hospitals. This differs from the median and average percentages of the
individual hospitals’ percentages.
50

Figure 33. Percentage of Total Revenue Spent on Medical Research by Community Type
(Averages and Medians)
(n=104)
3.2%
0.0%
0.5%
0.7%
1.6%
0.3%
0.1%
0.2%
0.4%
0.0%
0.0%
0.5%
1.0%
1.5%
2.0%
2.5%
3.0%
3.5%
High
Population
Critical
Access
Rural Non-
CAH
Other Total
Community Type
Percentage of Total Revenue Spent on Medical Research
Average Median
All of the medians are less than 0.5% and all the averages except for hospitals in
the high population community type (and overall) are less than 1%. Hospitals in
high population areas reported an average percentage of total revenue spent on
medical research of 3.2%. A few hospitals in the high population category with
comparatively large reported research expenditures as a percentage of their total
revenues explains the significant variation between average and median
amounts for this group and overall.
Figure 34 provides a breakdown of total revenue spent on medical research by
the respondent group in four percentage bands by community type.
51

Figure 34. Distribution of Hospitals by Community Type Based on Percentage of Total
Revenues Spent on Medical Research
(n=104)
26%
100%
40%
48%
41%
0%
20%
25%
24%
34%
0%
40%
29%
13%
0% 0%
2%
6%
26%
25%
0%
20%
40%
60%
80%
100%
120%
High
Population
Critical
Access
Rural Non-
CAH
Other To
Community Type
Percentage of Hospitals
tal
0% - .10% 0.11% - .50% .51% - 10.0% Over 10.0%
41% of the hospitals in the sample reported spending 0.1% or less of their total
revenue on medical research. 24% reported spending between 0.11% and
0.5%, and 29% reported spending between 0.51% and 10%. 6% of hospitals
reported spending more than 10% of their total revenue on medical research. No
general pattern describes the reported data across community types.
6. Aggregate Medical Education and Training Expenditures by
Community Type
77% of the hospitals reported medical education and training expenditures. The
aggregate medical education and training expenditures reported as spent by
these hospitals was 3.37% of total revenues.
44
The average and median
percentages of medical education and training expenditures reported by 378
hospitals as a percentage of revenues were 1.3% and 0.3%, respectively.
45
Figure 35 shows the average and median percentages of total revenue spent on
medical education and training across community types.
44
This represents the total medical education and training expenditures divided by total revenues
for the entire group of 378 hospitals.
45
The group of 15 hospitals that reported 93% of the aggregate reported medical research
expenditures also reported 58% of the aggregate reported medical education and training
expenditures (see Section VI.B, below).
52

Figure 35. Percentage of Total Revenue Spent on Medical Education and Training
by Community Type
(Averages and Medians)
(n=378)
2.7
0.2
0.6
1.3 1.3
1.6
0.1
0.2
0.4
0.3
0
0.5
1
1.5
2
2.5
3
High
Population
(n=81) 86%*
Critical Access
(n=41) 60%*
Rural Non-
CAH (n=56)
72%*
Other (n=200)
80%*
Total (n=378)
77%*
Community Type
* Percentage of respondents reporting Medical and Education Training amounts
Percentage of Total Revenue Spent on Medical Education and Training
Average Median
Hospitals in high population areas and hospitals in other urban and suburban
areas reported higher average and median percentages of total revenue spent
on medical education and training than the rural hospitals in the study.
As Figure 36, below, shows, most hospitals (57%) reporting revenue spent on
medical education and training reported spending no more than 0.5% of their
total revenue on such activities. 12% reported spending over 4% on medical
education and training.
53

Figure 36. Distribution of Hospitals by Community Type Based on Percentage of
Revenues Spent on Medical Education and Training
(Averages)
(n=378)
43%
30% 30%
42%
24%
12%
8%
14%
12%
31%
3%
22%
19%
26%
3%
11%
12%
15%
27%
16%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
High Population
(n=81)
Critical
Access/Rural-Non-
CAH (n=97)
Other (n=200) Total (n=378)
Community Type
Percentage of Hospitals
0.0% - .10% (n=113) 0.11% - .50% (n=102) .51% - 1.0% (n=46)
1.01% - 4.0% (n=71) Over 4.0% (n=46)
In the figure above, the two categories of rural hospitals were combined to
prevent potential identification of respondent hospitals. 93% of CAHs and 81%
of non-CAH rural hospitals reported spending in the two lowest categories (i.e.,
0.5% or less spent on medical education and training). 57% of hospitals in high
population areas reported spending in the two highest ranges (i.e., over 1%
spent on medical education and training).
7. Aggregate Community Program Expenditures by Community Type
The category of community program expenditures consists of seven separate
sub-types: lectures, seminars and education; medical screening; newsletters and
publications; improving access to health care; immunization programs; studies on
community’s unmet health care needs; and other health care promotion.
The following table summarizes community program expenditures by individual
community type.
54

Figure 37. Amounts and Percentages of Community Program Expenditures,
by Expenditure Category and Community Type
Community Type
High Population Critical Access
Rural - Non
Critical
Other Aggregate
Community Access
Urban &
Suburban
Program (N = 89) (N = 62) (N = 75) (N = 222)
(N = 448)
Expenditure
Amount % of Amount % of Amount % of Amount % of Amount % of
(in $ total (in $ total (in $ total (in $ total (in $ total
million) CPE million) CPE million) CPE million) CPE million) CPE
▪ Other healthcare 174.0 53% 3.3 12% 6.9 22% 61.3 31% 245.5 42%
promotion
▪ Improving access to 111.4 34% 11.6 41% 14.3 45% 70.3 35% 207.6 35%
healthcare
▪ Lectures, seminars, 15.5 5% 2.7 10% 5.1 16% 30.9 15% 54.2 9%
and education
▪ Medical 11.1 3% 6.4 23% 1.7 5% 13.2 7% 32.4 6%
screening
▪ Newsletter/ 8.5 3% 1.1 4% 2.7 8% 19.6 10% 31.9 5%
publications
▪ Immunization 7.6 2% 1.8 6% 0.6 2% 2.0 1% 12.0 2%
programs
▪ Studies on community's 1.8 1% 1.4 5% 0.5 2% 2.7 1% 6.4 1%
unmet healthcare needs
Total Community Program
Expenditures
329.9 100% 28.3 100% 31.8 100% 200.0 100% 590.0 100%
Figure 38, below, shows the distribution of community program expenditures
broken out by expenditure category and community type.
55

Figure 38. Percentages of Community Program Expenditures by Expenditure Category
and Community Type
(n=448)
3%
2%
5%
1%
34%
3%
53%
23%
6%
10%
5%
41%
4%
12%
5%
2%
16%
2%
45%
8%
22%
7%
1%
15%
1%
35%
10%
31%
0%
10%
20%
30%
40%
50%
60%
Medical Screening Immunization
Programs
Lectures and
Seminars
Unmet Healthcare
Needs
Improving Access
to Healthcare
Newsletters and
Publications
Other Healthcare
Promotion
Community Programs
Percentage of Subtotal of Community Program Expenditures
High Population (n=89) Critical Access (n=62) Rural - Non - CAH (n=75) Other (N=222)
The table and chart illustrate there is considerable variation across the
community types regarding expenditures for the various components of
community programs. For example, high population area hospitals reported 53%
of their community program expenditures on other health care promotion and 3%
on medical screening, whereas CAHs reported spending 12% and 23%
respectively, of community program expenditures on those items.
Figure 39, below, shows the average and median percentages of total revenues
spent on community programs by community type.
56

Figure 39. Percentage of Total Revenues Spent on Community Programs
by Community Type
(Averages and Medians)
(n=448)
1.67
0.95
0.55
0.77
0.94
0.19
0.27
0.23
0.21
0.22
0.00
0.20
0.40
0.60
0.80
1.00
1.20
1.40
1.60
1.80
High
Population
(n=89)
Critical
Access (n=62)
Rural - Non-
CAH (n=75)
Other (n=222) Totals (n=448)
Community Type
Percentage of Total Revenue Spent
Averages Medians
8. Aggregate Community Benefit Expenditures by Community Type
The entire respondent group of 485 hospitals reported aggregate community
benefit expenditures of $9.4 billion. Uncompensated care was reported at $5.2
billion, medical education and training at $2.2 billion, medical research at $1.4
billion, and community programs at $0.6 billion. Aggregate community benefit
expenditures were not evenly distributed by the hospitals in the study, but were
concentrated in a relatively small number of hospitals. 9% of the hospitals
reported 60% of the aggregate community benefit expenditures; 19% of the
hospitals reported 78% of the aggregate community benefit expenditures.
Figure 40 and Figure 41, below, break down aggregate community benefit
expenditure by community type, and provide a community benefit expenditure
profile or mix showing the percentage of community benefit expenditures for
each community type that is comprised of reported uncompensated care,
medical education and training, medical research, and community programs.
46
46
The mix of community benefit expenditures changes when the group of 15 hospitals reporting
93% of aggregate reported medical research expenditures is isolated. See Section VI.B, below.
57

Figure 40. Amounts and Percentages of Total Community Benefit Expenditures
by Expenditure Category and Community Type
Community Type
High Population Critical Access
Rural - Non
Critical
Other Aggregate
Community Access
Urban &
Suburban
Benefit
(N = 485)
Expenditure
Amount % of Amount % of Amount % of Amount % of Amount % of
(in $ total (in $ total (in $ total (in $ total (in $ total
million) CBE million) CBE million) CBE million) CBE million) CBE
▪ Uncompensated 2,043.0 42% 115.9 77% 415.2 76% 2,653.3 69% 5,227.5 56%
Care
▪ Medical, Education & 1,248.4 26% 5.7 4% 92.5 17% 817.9 21% 2,164.5 23%
Training
▪ Medical
1,232.6 25% 0.0 0% 6.2 1% 173.3 5% 1,412.1 15%
Research
▪ Community 329.9 7% 28.3 19% 31.8 6% 200.0 5% 590.0 6%
Programs
Total Community Benefit
Expenditures
4,853.9 100% 149.9 100% 545.7 100% 3,844.5 100% 9,394.1 100%
Figure 40 shows the distribution of aggregate reported community benefit
expenditures across the community types in absolute dollars. Rural hospitals
(CAH and other) comprised 30% of the hospitals, but reported 7% of aggregate
community benefit expenditures. The amounts reported as spent on medical
education and training, and on medical research, by rural hospitals were low
compared to the other community types. High population hospitals comprised
19% of the hospitals, but reported 52% of aggregate community benefit
expenditures, 87% of all amounts reported as spent on medical research, and
58% of amounts reported as spent on medical education and training.
58

Figure 41. Percentage of Community Benefit Expenditures by Expenditure Category and
Community Type
(n=485)
42%
77%
76%
69%
56%
4%
17%
21%
23%
0%
1%
5%
15%
7%
19%
6%
5%
6%
26%
25%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
High
Population
Critical
Access
Rural Non
CAH
Other Totals
Community Type
Percentage of Overall Community Benefit Expenditure
Uncompensated Care Medical Education and Training Medical Research Community Programs
There are material differences in community benefit expenditure profiles across
the community types. One contrast among the different types is that hospitals in
the high population areas reported spending more than half (51%) of their
community benefit expenditures on medical education and training and medical
research. The hospitals in the other categories spent considerably less in these
areas. 42% of the reported spending on community benefit expenditures for
hospitals in the high population areas was spent on uncompensated care,
compared to 69% to 77% for uncompensated care by the other community types.
CAHs reported spending 19% of their community benefit expenditures on
community programs compared to 5% to 7% for the other community types.
Figure 42, below, reports the average and median percentage of total revenue
reported as spent on community benefit expenditures, by category and
community type.
47
47
The results change when the group of 15 hospitals that reported 93% of aggregate reported
medical research expenditures is isolated. See Section VI.B, below.
59

Figure 42. Average and Median Percentage of Total Revenue Spent on Community Benefit
Expenditures by Expenditure Category and Community Type
Community Type
Category of High Population Rural - Critical
Rural - Non
Critical
Other Aggregate
Community Hospitals Access Hospitals Access Hospitals Hospitals
Benefit Expenditure (N = 485)
Average Median Average Median Average Median Average Median Average Median
(%) (%) (%) (%) (%) (%) (%) (%) (%) (%)
▪ Uncompensated 7.88 4.82 5.59 2.14 7.57 2.74 7.28 4.33 7.21 3.88
Care (N= 466)
▪ Medical, Education 2.66 1.63 0.19 0.09 0.59 0.19 1.25 0.39 1.34 0.34
& Training (N = 378)
▪ Medical
3.18 0.39 0.00 0.00 0.45 0.29 0.73 0.12 1.61 0.22
Research (N=104)
▪ Total Community Program 1.67 0.19 0.95 0.27 0.55 0.23 0.77 0.21 0.94 0.22
Expenditures (N = 448)
Total Community Benefit
Expenditures
12.70 9.84 6.33 2.84 8.36 3.17 8.87 5.75 9.18 5.50
Figure 43 below shows the (rounded) average and median total revenues spent
on community benefit expenditures by community type.
Figure 43. Average and Median of Total Revenue Spent on Community Benefit
Expenditures by Community Type
(Averages and Medians)
(n=485)
13%
6%
8%
9% 9%
10%
3% 3%
6% 6%
0%
2%
4%
6%
8%
10%
12%
14%
High
Population
Critical
Access
Rural - Non
CAH
Other Total
Community Type
Percentage of Total Revenue Spent
Average Median
60
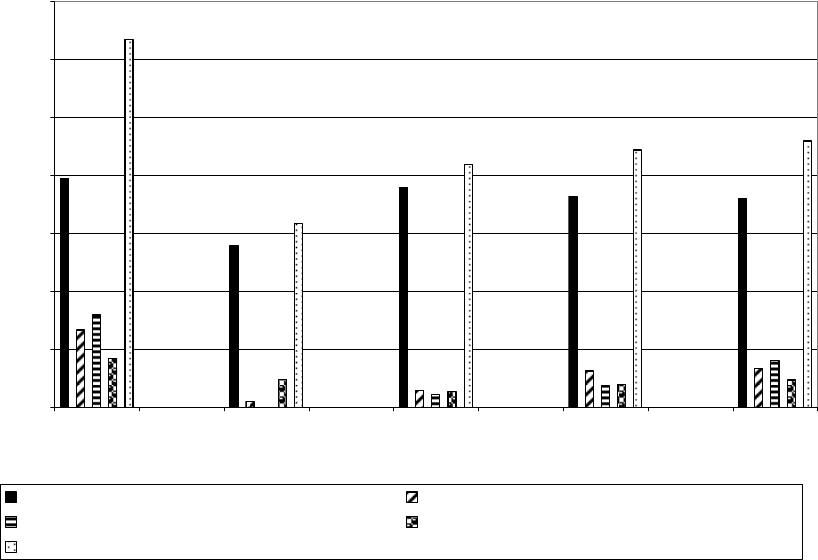
The average and median reported aggregate community benefit expenditures as
a percentage of total revenues were 9% and 6%, respectively, for the entire
group. The highest reported average and median amounts were for the high
population group (13% and 10%, respectively), and the lowest were for the CAH
group (6% and 3%, respectively).
Figure 44 and Figure 45, below, show the percentages of revenue (average and
median) spent on various community benefit expenditures by expenditure and
community type.
Figure 44. Percentage of Total Revenue Spent on Various Community Benefit
Expenditures by Expenditure and Community Type
(Averages)
(n=485)
5.6%
7.6%
7.3%
7.2%
0.0%
1.0%
12.7%
6.3%
8.4%
8.9%
7.9%
2.7%
0.2%
0.6%
1.3%
1.3%
3.2%
0.5%
0.7%
1.6%
1.7%
0.6%
0.8%
0.9%
9.2%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
High
Population
Critical
Access
Rural - Non
CAH
Other Aggregate
Community Type
Average Percentage of Total Revenue Spent
Uncompensated Care (n=466) Medical Education and Training (n=378)
Medical Research (n=104) Total Community Program Expenditures(n=448)
Total CBE (n=485)
61

Figure 45. Percentage of Total Revenues Spent on Various Community Benefit
Expenditures by Expenditure and Community Type
(Medians)
(n=485)
4.8%
2.1%
2.7%
4.3%
3.9%
1.6%
0.1%
0.2%
0.4%
0.4%
0.2%
9.8%
2.8%
3.1%
5.8%
5.5%
0.3%
0.1%
0.2%
0.3%
0.0%
0.2%
0.2%
0.2%
0.3%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
High
Population
Critical
Access
Rural - Non
CAH
Other Aggregate
Community Type
Median Percentage of Total Revenue Spent
Uncompensated Care (n=466) Medical Education and Training (n=378)
Medical Research (n=104) Total Community Program Expenditures (n=448)
Total CBE (n=485)
9. Aggregate Community Benefit Expenditures as a Percentage of
Revenues
This section summarizes the distribution of aggregate community benefit
reporting across the community types. Figure 46, Figure 47, and Figure 48 show
the distribution of hospitals, by community type, with reported community benefit
expenditures within specified percentages of total revenue ranges. Figure 49
displays the cumulative percentage of hospitals within each community type that
reported aggregate community benefit expenditures as a percentage of total
revenues at or less than specified levels (e.g., less than 5% of total revenues).
62

Figure 46. Number and Percentage of Hospitals with Reported Community Benefit
Expenditures as Percentage of Total Revenue, by Community Type
Community Type
High
Rural -
Critical
Rural-Non
Critical
Other
Total Community Benefit
Expenditure as Percentage
Population Access Access Hospitals All Hospitals
of Total
Hospitals Hospitals Hospitals
Revenues
N % N % N % N % N %
< 2% 10 11 * 39 * 31 41 17 101 21
2% - < 5% 20 21 * 22 * 26 73 29 128 26
5% - < 10% 18 19 * 19 * 22 65 26 113 23
10% - < 20% 29 31 * 14 * 13 51 21 99 21
≥ 20% 17 18 * 6 * 8 17 7 44 9
Total 94 100 * 100 * 100 247 100 485 100
* Not shown to prevent potential identification of respondent hospitals.
21% of all hospitals reported aggregate community benefit expenditures of less
than 2% of total revenues; 47% reported aggregate community benefit
expenditures of less than 5% of total revenues. Figure 47 and Figure 48, below,
illustrate the variations across community types reported in the above table.
Figure 47. Percentage of Hospitals with Reported Community Benefit Expenditures as
Percentage of Total Revenue by Community Type
(n=485)
11%
31%
18%
39%
22%
19%
14%
6%
26%
22%
8%
17%
29%
26%
21%
7%
21%
9%
19%
21%
13%
31%
21%
23%
26%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
Under 2% 2.0% Under
5.0%
5.0% Under
10.0%
10.0 % Under
20.0%
Over 20.0%
Percentage of Total Revenue Ranges
Percentage of Hospitals
High Population Critical Access Rural Non-CAH Other Total
63

Figure 48. Percentage of Hospitals with Reported Community Benefit Expenditures as
Percentage of Total Revenue by Community Type
(n=485)
39%
31%
17%
21%21%
22%
26%
29%
26%
19% 19%
22%
26%
31%
14%
13%
21%
18%
6%
8%
7%
9%
11%
23%
21%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Community Types
Percentage of Hospitals
Under 2% 2.0% Under 5.0% 5.0% Under 10.0% 10.0% Under 20.0% Over 20.0%
The figures above show the distribution of hospitals that reported spending a
certain percentage of their total revenue on community benefit expenditures
within specified ranges by community types. The percentage of hospitals in the
high population areas that reported spending at least 10% of revenues was 49%,
compared to 21% or less for rural hospitals. The percentages of CAHs and rural
(non-CAH) hospitals that reported spending less than 5% of total revenues on
community benefit expenditures were 61% and 57%, respectively, compared to
32% for high population hospitals.
Figure 49, below, shows, on a cumulative basis, the percentage of hospitals
reporting community benefit expenditures at or less than specified percentages
of revenue levels.
Figure 49. Percentage of Hospitals Reporting Community Benefit Expenditures Less Than
Specified Percentage of Revenue Levels
Community Type <2% <5% <10%
High population 11% 32% 51%
CAHs 39% 61% 81%
Rural (non-CAHs) 31% 57% 79%
Other 17% 46% 72%
Total 21% 47% 71%
64
Figure 49 shows that 21% of all hospitals reported spending less than 2% of total
revenues on aggregate community benefit expenditures. 47% reported spending
less than 5% of total revenues on community benefit expenditures. CAHs and
rural (non-CAH) hospitals included the highest percentage of hospitals that
reported community benefit expenditures below the 2% and 5% of total revenue
levels. 49% of high population hospitals reported spending at least 10% of total
revenues on community benefit expenditures, compared to 30% of hospitals
overall.
65

C. Comparisons of Certain Information By Annual Revenue Size
48
1. Summary of Key Findings – Revenue Size
a. The patient mix for each revenue size category generally followed that
for the overall group – in descending order, private insurance,
Medicare, Medicaid, uninsured, and other public programs. Each
revenue size reported 7% to 9% of patients with no health insurance
coverage. Hospitals with revenues under $25 million reported the
highest percentage of Medicare patients (37% compared to 31%
overall), and hospitals with revenues over $500 million reported the
highest percentage of Medicaid patients (21% compared to 15%
overall).
b. Between 92% and 98% of each revenue size category reported
uncompensated care expenditures. Participation in most expenditure
types was lowest for hospitals with under $25 million in revenues, and
in many instances (medical education and training, medical research,
and certain community programs) generally increased with revenue
size. Participation in medical research ranged from under 10% of
hospitals (those under $100 million in revenues) to 67% of hospitals
(those over $500 million in revenues).
c. The median percentage of patients reported as receiving
uncompensated care was 3% overall, but was highest for the larger
revenue size categories (10% for revenues between $250 million and
$500 million and 5% for revenues over $500 million). Four of the
revenue size groups (hospitals with revenues between $250 million
and $500 million were the exception) reported higher percentages of
patients without insurance than their median percentages of patients
receiving uncompensated care. Each revenue size reported higher
average percentages of patients receiving uncompensated care than
percentages of patients without insurance.
d. The average and median percentages of total revenues reported as
spent on uncompensated care were 7% and 4%, respectively. The
averages ranged from 6% to 9%; the medians ranged from 3% to 6%.
Although the median percentages generally increased with revenue
size, there was no correlation between size and the average
percentage of total revenue spent on uncompensated care. The
percentage of hospitals reporting uncompensated care expenditures at
3% or less of total revenues was 43% overall, and ranged from 33% to
49%, decreasing as hospital size increased. The percentage of
hospitals reporting uncompensated care expenditures at 5% or less of
48
For a description of the revenue size categories, see Section II.D, above.
66
total revenues was 58% overall, ranging from 49% to 61%, with no
correlation to revenue size.
e. Uncompensated care represented the largest community benefit
expenditure for the overall group (56%) and for each revenue size.
However, the percentage of overall community benefit expenditures
reported as spent on uncompensated care decreased with revenue
size, ranging from 35% for hospitals with revenues over $500 million to
93% for hospitals with revenues under $25 million. The mix of
community benefit expenditures among uncompensated care, medical
research, medical education and training, and community programs
varied considerably across revenue size categories.
f. The average and median percentages of total revenues reported as
spent on medical research, and on medical education and training,
varied considerably across revenue sizes. Average and median
percentages of total revenues spent on medical education and training
and on medical research were largest for hospitals with over $500
million in revenues. 15 hospitals reported 93% of the aggregate
reported medical research expenditures. This group reported 58% of
the aggregate reported medical education and training expenditures.
g. There was considerable variation across revenue sizes regarding
community program expenditures. However, each revenue size
category reported spending most of its community program
expenditures on improving access to health care and other health care
promotion.
h. The median percentage of total revenue reported as spent on
aggregate community benefit expenditures increased with revenue
size, ranging from 3% for hospitals with revenues under $25 million to
11% for hospitals with revenues over $500 million. The average
percentage generally increased with revenue size. The overall median
and average percentages were 5.5% and 9.2%, respectively.
i. The percentage of hospitals reporting spending less than 2%, and less
than 5%, of total revenues on community benefit expenditures
decreased with revenue size. 34% of hospitals with revenues under
$25 million reported spending less than 2% of revenues on community
benefit expenditures, compared to 5% of hospitals with revenues over
$250 million. 60% of hospitals with revenues under $25 million
reported spending less than 5% of total revenues on community
benefit expenditures, compared to 47% overall.
2. Patient Mix (Based on Type of Insurance Coverage) by Revenue
Size
67

Overall, hospitals reported that 43% of their patients had private insurance, 31%
were covered by Medicare, 15% were covered by Medicaid, 3% were covered by
other public insurance programs, and 8% were uninsured.
49
The following figures
show breakouts of this distribution of types of patient insurance coverage across
the five revenue categories.
Figure 50. Distribution of Health Insurance Coverage by Revenue Size Categories*
Category of Health Insurance Coverage
Revenue Size Category
Private
Insurance
(%)
Medicare
(%)
Medicaid
(%)
Other
Public
Insurance
(%)
No
Health
Insurance
(%)
Under $25M 35.1% 37.2% 15.6% 4.6% 9.2%
$25M under $100M 43.2% 30.1% 15.4% 2.5% 7.4%
$100M under $250M 46.5% 31.7% 13.1% 2.9% 6.8%
$250M under $500M 47.1% 27.5% 14.7% 2.1% 7.8%
Over $500M 45.5% 23.4% 20.6% 2.8% 8.3%
All patients 43.3% 31.0% 15.1% 2.9% 7.7%
* Some hospitals reported total patient amounts that did not equal the total number of
patients reported in the various health insurance coverage categories.
49
According to the U.S. Census Bureau, the percentage of individuals without health insurance in
2005 was 15.3%. U.S. Census Bureau, Current Population Survey, 2006 Annual Social and
Economic Supplement (as revised March 2007).
68

Figure 51. Percentage of Patients with Insurance Coverage by Total Revenue Category,
by Type of Coverage
(n=479)
35%
37%
16%
5%
9%
43%
30%
15%
3%
7%
32%
13%
3%
7%
47%
28%
15%
2%
8%
23%
21%
3%
8%
31%
15%
3%
8%
47%
46%
43%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
Private
Insurance
Medicare Medicaid Other
Insurance
Uninsured
Insurance Coverage
Percentage of Patients
Under $25M $25M under $100M $100M under $250M
$250M under $500M Over $500M Totals
69

Figure 52. Percentage of Patients by Type of Insurance Coverage,
by Total Revenue Size
(n=479)
47%
47%
46%
43%
31%
16%
15%
15%
2%
3% 3%
9%
7%
7%
8%
43%
35%
37%
23%
28%
32%
30%
15%
13%
21%
3%3%
5%
8%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Totals
Revenue Size
Percentage of Patients
Private Insurance Medicare Medicaid Other Public Insurance Uninsured
The distribution of types of coverage across the various revenue categories is
similar to the distribution of the entire group. However, the hospitals with total
revenues over $500 million reported a smaller percentage of patients with
coverage through Medicare (23% vs. 31%) and a larger percentage of patients
with coverage through Medicaid (21% vs. 15%) compared with the total group.
Hospitals with total revenue under $25 million reported a smaller percentage of
patients with private insurance (35% vs. 43%) and a larger percentage of
patients with coverage through Medicare (37% vs. 31%) compared with the total
group. Each revenue size category reported 7% to 9% of patients with no
insurance coverage.
3. Number and Percentage of Hospitals Reporting Community
Benefit Expenditures, by Expenditure Type within Revenue Size
The table below shows the percentages of hospitals that reported the various
types of community benefit expenditures.
70

Figure 53. Number and Percentage of Hospitals Reporting Community Benefit
Expenditures by Expenditure Category and Revenue Size
Revenue Size
Category of Under $25 M $25M to $100M to $250M to $500M and Aggregate
Community Under $100M Under 250M Under $500M Over
Benefit
(N = 485)
Expenditure
N % of all N % of all N % of all N % of all N % of all % of
hospitals
in
hospitals
in
hospitals
in
hospitals
in
hospitals
in
N all
each
category
each
category
each
category
each
category
each
category
hospitals
▪ Uncompensated 80 93% 166 96% 127 95% * >95% * >90% 466 95%
Care
▪ Medical, 41 48% 125 72% 122 92% 57 93% 33 92% 378 77%
Education &
Training
▪ Medical
*
Less
than
*
Less
than
37 28% 30 49% 24 67% 104 21%
Research
10% 10%
▪ Lectures, 53 62% 143 83% 118 89% 50 82% 23 64% 387 79%
seminars &
education
▪ Medical 58 67% 132 76% 116 87% 46 75% 25 69% 377 77%
screening
▪ Newsletter/ 42 49% 137 79% 116 87% 55 90% 24 67% 374 76%
publications
▪ Improving 30 35% 88 51% 87 65% 49 80% 19 53% 273 56%
access to
healthcare
▪ Immunization 36 42% 70 40% 63 47% 19 31% 14 39% 202
41%
programs
▪ Other 15 17% 61 35% 49 37% 22 36% 7 19% 154 31%
healthcare
promotion
▪ Studies on 13 15% 45 26% 44 33% 26 43% 11 31% 139 28%
community's
unmet health-
care needs
*Not shown to prevent potential identification of respondent hospitals.
Each revenue size reported a higher participation rate for providing
uncompensated care than for any other type of community benefit. The
percentage of hospitals in the under $25 million revenue category that reported
expenditures for medical education and training and for medical research is
significantly less than the percentages reported for the other revenue groups.
The same is true for several of the community program expenditures (e.g.,
newsletter and publications, improving access to healthcare care, and studies on
unmet health needs). The percentage of hospitals reporting medical research
71

and medical education and training expenditures generally increased with
revenue size.
4. Aggregate Uncompensated Care by Revenue Size
The aggregate uncompensated care expenditures reported by 466 hospitals as a
percentage of total revenues was 6.41%.
50
Uncompensated care expenditures
were not evenly distributed by the hospitals in the study, but were concentrated
in a relatively small number of hospitals. 14% of the hospitals reported 63% of
the aggregate uncompensated care expenditures; 26% of the hospitals reported
82% of the aggregate uncompensated care expenditures.
Percentage of patients. Figure 54 shows the reported average and median
percentages of patients receiving uncompensated care, by revenue size groups.
Figure 54. Percentage of Patients Receiving Uncompensated Care by Revenue Size
Revenue Size Number Average Median
of hospitals (%) (%)
Under $25M 73 9.2 2.7
$25M - under $100M 159 8.1 2.5
$100M - under $250M 123 9.1 4.0
$250M - under $500M 58 12.9 9.8
$500M and over 30 16.6 5.3
Total 443 9.8 3.4
Note: Table only includes those hospitals that reported the number of
patients receiving uncompensated care.
Figure 54 shows that the average percentage of patients receiving
uncompensated care was 9.8 percent, with a median of 3.4 percent. With the
exception of the under $25 million group, the average percentage of patients
receiving uncompensated care increased as hospital revenue size increased.
The medians did not correlate with revenue size.
Percentage of revenues
. Figure 55 and Figure 56 illustrate the average and
median percentages of total revenue reported as spent on uncompensated care
for each revenue size group.
50
This reflects the total reported uncompensated care expenditures divided by total reported
revenues for the entire group of 466 hospitals. This differs from the average and median
percentages of individual hospitals’ percentages reported below (e.g., Figure 55).
72

Figure 55. Percentage of Total Revenue Spent on Uncompensated Care by Revenue Size
(Average and Median)
(n=466)
Revenue Size Average Median
Under $25 Million 9.3% 3.1%
$25 Million to under
$100 Million
6.6% 3.2%
$100 Million to under
$250 Million
6.4% 4.3%
$250 Million to under
$500 Million
8.5% 5.5%
Over $500 Million 5.6% 4.7%
Total 7.2% 3.9%
Figure 56. Percentage of Total Revenue Spent on Uncompensated Care
(Average and Median)
(n=466)
7.2%
6.6%
9.3%
6.4%
8.5%
5.6%
3.1%
3.2%
4.3%
3.9%
5.5%
4.7%
0.0%
1.0%
2.0%
3.0%
4.0%
5.0%
6.0%
7.0%
8.0%
9.0%
10.0%
Under $25
Million
$25 Million
under $100
Million
$100
Million
under $250
Million
$250
Million
under $500
Million
Over $500
Million
Total
(n=466)
95%*
Total Revenue
*
Percentage of respondents reporting uncompensated care amounts
Percentage of Total Revenue Spent on Uncompensated Care
Average Median
As measured by medians, the percentage of revenue spent on uncompensated
care increases over the lower four total revenue categories, but declines
somewhat in the largest total revenue category. As measured by averages, the
percentage of total revenue spent on uncompensated care is highest in hospitals
with revenue under $25 million (9.3%) and hospitals with total revenues between
$250 million and $500 million (8.5%), and lower in the other three categories.
Except for hospitals with total revenues over $500 million there is a sizeable
difference between the average and median percentages of total revenue spent
on uncompensated care.
73

Figure 57, below, shows the percentage of hospitals within each revenue size
category that reported uncompensated care as a percentage of total revenues
within certain ranges.
Figure 57. Number and Percentage of Hospitals with Reported Uncompensated Care as a
Percentage of Total Revenue by Revenue Size
Revenue Size
Uncompensated
Care
Expenditure as
Percentage
< $25M
$25M <
$100M
$100M <
250M
$250M <
500M
≥ $500M
Overall
of Total Revenues
% % % % % N %
≤ 1%
26 20 17 12 9 87 19
Over 1% - ≤ 3% 23 28 20 22 24 112 24
Over 3% - ≤ 5% 11 13 18 15 27 71 15
Over 5% - ≤ 10% 16 21 22 23 27 99 21
> 10% 24 17 22 28 12 97 21
Total 100 100 100 100 100 466 100
The number of hospitals is not included in each category to prevent potential identification of respondent hospitals.
Figure 58. Distribution of Hospitals by Revenue Size Based on Percentage of Total
Revenues Spent on Uncompensated Care
(Averages)
(n=466)
16%
24%
28%
13%
17%
20%
18%
22% 22%22%
15%
23%
28%
9%
24%
27% 27%
12%
19%
21%
26%
23%
11%
21%
20%
17%
12%
21%
15%
24%
0%
5%
10%
15%
20%
25%
30%
0.00% - 1.0% 1.01% - 3.0% 3.01% - 5.0% 5.01% -
10.0%
Over 10.0%
Percentage of Total Revenue Spent
* Percentage of respondents reporting uncompensated care amounts
Percentage of Hospitals
Under $25M $25M under $100M $100M under $250M
$250M under $500M Over $500M Total (n=466) 95%*
74

Figure 59. Distribution of Hospitals by Revenue Size Based on Percentage of Total
Revenue Spent on Uncompensated Care
(Averages)
(n=466)
20%
17%
12%
9%
19%
28%
20%
22%
24% 24%
27%
16%
21%
22%
23%
24%
28%
26%
23%
15%
15%
18%
13%
11%
21%
27%
21%
12%
22%
17%
0%
5%
10%
15%
20%
25%
30%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
(n=466)
95%*
Revenue Size
*Percentage of respondents reporting uncompensated care amounts
Percentage of Hospitals
0.01% - 1.0% 1.01% - 3.0% 3.01% - 5.0% 5.01% - 10.0% Over 10.0%
Figure 59, above, shows that almost half (49%) of the hospitals in the under $25
million revenue category reported expenditures in the two lowest percentage of
revenue categories (i.e., less than 3%). More than half (51%) of the hospitals in
the $250 to $500 million revenue category reported expenditures in the two
highest percentages of revenue categories (i.e., more than 5%). 58% of all
hospitals reported that uncompensated care expenditures were less than 5% of
total revenues. While not included in the chart to prevent potential identification
of respondent hospitals, a small percentage of hospitals in four of the revenue
sizes reported expenditures greater than 50% of revenues.
Figure 60. Percentage of Hospitals Reporting Uncompensated Care Expenditures at or
Less Than Specified Percentages of Revenue Levels
Revenue Size ≤1% ≤3% ≤5% ≤10%
Under $25 million 26% 49% 60% 76%
$25 million to under $100 million 20% 49% 61% 83%
$100 million to under $250 million 17% 37% 55% 77%
$250 million to under $500 million 12% 34% 49% 72%
Over $500 million 9% 33% 60% 87%
Total 19% 43% 58% 79%
As Figure 60 shows, between one third and one half of the hospitals in each
revenue size category reported 3% or less of total revenues as spent on
75

uncompensated care. Approximately half (49%) or more of each category
reported 5% or less of total revenues as spent on uncompensated care.
See Section VI.C.2, below, for an analysis of the reporting of various shortfalls
and bad debt as uncompensated care by revenue size.
5. Aggregate Medical Research Expenditures by Revenue Size
117 of the hospitals reported conducting medical research, although only 104
hospitals actually reported an amount of medical research expenditures. The
aggregate medical research expenditures reported by the 104 hospitals that
reported such amounts was 3.48% of total revenues.
51
The average and median
percentages of medical research expenditures as a percentage of total revenues
were 1.6% and 0.2%, respectively.
A group of 15 hospitals reported 93% of the overall reported medical research
expenditures. See Section VI.B, below, for an analysis of community benefit
expenditures of this group.
Figure 61, below, shows the average and median percentage of total revenue
reported as spent by hospitals on medical research expenditures broken out by
revenue size.
51
This represents the total medical research expenditures divided by the total revenues for the
entire group of 104 hospitals. This differs from the median and average percentages of the
individual hospitals’ percentages.
76

Figure 61. Percentage of Total Revenue Spent on Medical Research by Revenue Size
(Averages and Medians)
(n=104)
1.6%
3.9%
1.6%
0.1%
0.8%
0.8%
0.2%
1.2%
0.2%
0.0%
0.4%
0.1%
0.0%
0.5%
1.0%
1.5%
2.0%
2.5%
3.0%
3.5%
4.0%
4.5%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Totals
Revenue Size
Percentage of Total Revenue Spent on Medical Research
Average Median
In general, there is a significant difference between the average and the median
percentages reported as spent by revenue size categories on medical research.
The largest hospitals, those with total revenue in excess of $500 million, reported
spending the largest percentage of total revenue measured by average (3.9%)
and median (1.2%). The next highest percentage was the second smallest
revenue category of hospitals, those with total revenues between $25 million and
$100 million, which was comparable to the overall group. All other categories
reported spending smaller percentages of their total revenue on medical
research.
Figure 62 illustrates the percentage of total revenue reported as spent on
medical research by those hospitals reporting such expenditures.
77

Figure 62. Distribution of Hospitals by Revenue Size Based on Percentage of Total
Revenue Spent on Medical Research
(n=104)
31%
62%
33%
21%
41%
38%
19%
37%
13%
24%
23%
16%
27%
54%
29%
8%
3% 3%
13%
6%
0%
10%
20%
30%
40%
50%
60%
70%
$0 to under
$100M (n=13)
5%*
$100M under
$250M (n=37)
28%*
$250M under
$500M (n=30)
49%*
Over $500M
(n=24) 67%*
Total (n=104)
21%*
Revenue Size
*Percentage of respondents reporting Medical Research amounts
Percentage of Hospitals
0% - .10% 0.11% - 0.50% .51% - 10.0% Over 10%
Figure 62 shows that 67% of the hospitals in the largest revenue category (over
$500 million) reported spending more than 0.5% of revenues on medical
research.
52
6. Aggregate Medical Education and Training Expenditures by
Revenue Size
77% of hospitals reported medical education and training expenditures. The
aggregate medical education and training expenditures reported as spent by
these hospitals was 3.37% of total revenues.
53
Figure 63 shows the average and median percentage of total revenues reported
as spent by hospitals on medical education and training broken out by total
revenue categories.
52
The two smallest revenue sizes were combined to prevent potential identification of respondent
hospitals.
53
This represents the total medical education and training expenditures divided by the total
revenues for the entire group of 378 hospitals. The group of 15 hospitals that reported 93% of the
aggregate reported medical research expenditures also reported 58% of the aggregate reported
medical education and training expenditures. See section VI.B, below.
78

Figure 63. Percentage of Total Revenue Spent on Medical Education and Training
by Revenue Size
(Averages and Medians)
(n=378)
0.5%
2.2%
4.5%
1.3%
1.6%
0.2%
1.3%
0.3%
0.5%
0.1%
3.8%
0.1%
0.0%
0.5%
1.0%
1.5%
2.0%
2.5%
3.0%
3.5%
4.0%
4.5%
5.0%
Under
$25M
(n=41)
48%*
$25M
under
$100M
(n=125)
72%*
$100M
under
$250M
(n=122)
92%*
$250M
under
$500M
(n=57)
93%*
Over
$500M
(n=33)
92%*
Total
(n=378)
77%*
Revenue Size
*Percentage of respondents reporting medical education/training amounts
Percentage of Total Revenue Spent on Medical Education and Training
Average Median
The average and median percentages of medical education and training
expenditures reported by 378 hospitals as a percentage of total revenues were
1.3% and 0.3%, respectively. Figure 63 above shows that larger hospitals as
measured by total revenue reported spending a greater percentage of their total
revenue on medical education and training than smaller ones.
Figure 64 shows the percentage of total revenue spent on medical education and
training within revenue size groups.
79

Figure 64. Distribution of Hospitals by Revenue Size Based on Percentage of Total
Revenue Spent on Medical Education and Training
(Averages)
(n=378)
40%
28%
30%
38%
14%
27%
12%
0%
7%
22%
39%
42%
19%
45%
14%
46%
23%
44%
10%
11%
16%
13%
12%
0%
12%
4%
21%
12%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
Under $25M
(n=41)
$25M under
$100M
(n=125)
$100M
under
$250M
(n=122)
$250M
under
$500M
(n=57)
Over $500M
(n=33)
Total
(n=378)
Revenue Size
Percentage of Hospitals
0.0% - .10% (n=113) 0.11% - .50% (n=102) .51% - 1.0% (n=46)
0.0% - 1.0% (n=4) 1.01% - 4.0% (n=71) Over 4.0% (n=46)
The two smallest revenue size groups (under $25 million and $25 million to $100
million) reported significantly larger percentages (90% and 78%, respectively) of
hospitals with medical education and training expenditures under 0.50% of total
revenues. On the other hand, the two largest revenue size groups ($250 million
to $500 million and over $500 million) reported significantly larger percentages of
hospitals with such expenditures over 1% of their total revenues (60% and 87%,
respectively). The three smallest percentage of revenue categories were
combined into a single category (0% - 1%) for the over $500 million revenue size
to prevent potential identification of respondent hospitals.
7. Aggregate Community Program Expenditures by Revenue Size
The following table summarizes community program expenditures by revenue
size.
80

Figure 65. Amount and Percentage of Community Program Expenditures by Expenditure
Category and Revenue Size
Revenue Size
Community Under $25 M $25M to $100M to $250M to $500M and Aggregate
Program Under $100M Under 250M Under $500M Over
Expenditure
(N = 70) (N = 161) (N = 127) (N = 61) (N = 29) (N = 448)
Amount % of Amount % of Amount % of Amount % of Amount % of Amount % of
(in $ total (in $ total (in $ total (in $ total (in $ total (in $ total
million) CPE million) CPE million) CPE million) CPE million) CPE million) CBE
▪ Other healthcare 1.2 18% 37.9 32% 74.2 48% 14.1 12% 118.1 61% 245.5 3%
promotion
▪ Improving access 2.6 40% 44.0 37% 43.8 28% 63.8 56% 53.3 27% 207.5 2%
to healthcare
▪ Lectures, seminars, 0.8 12% 7.8 7% 15.0 10% 18.2 16% 12.4 6% 54.2 1%
and education
▪ Medical 1.2 18% 14.8 12% 6.1 4% 6.2 5% 4.1 2% 32.4 0.3%
screening
▪ Newsletter/ 0.5 8% 5.2 4% 12.2 8% 9.5 8% 4.5 2% 31.9 0.3%
publications
▪ Immunization 0.2 3% 8.1 7% 1.6 1% 0.9 1% 1.3 1% 12.1 0.13%
Programs
▪ Studies on
community's
0.01 0.2% 2.2 2% 2.2 1% 1.3 1% 0.7 0% 6.4 0.07%
unmet healthcare
needs
Total Community
Program
Expenditures
6.5 100% 120.0 100% 155.1 100% 114.0 100% 194.4 100% 590.0 6%
Figure 66, below, shows the distribution of community program expenditures
broken out by expenditure category and revenue size.
81

Figure 66. Percentage of Community Program Expenditures
by Expenditure Category and Revenue Size
(n=448)
3%
12%
8%
18%
7% 7%
2%
4%
32%
1%
10%
28%
8%
48%
16%
56%
61%
40%
0.2%
18%
37%
12%
1%
4%
12%
5%
8%
1%
1%
2%
6%
27%
0%
1%
2%
0%
10%
20%
30%
40%
50%
60%
70%
Medical Screening
I
mmunizat
i
on
P
rogr
ams
L
ec
ture
s
an
d
S
emin
ars
Unmet Heal
t
hcare Needs
Improving Acces
s
to Healthcare
News
l
et
t
er
s
and Pub
li
c
at
io
ns
Other H
e
althc
a
re Promotion
Community Programs
Percentage of Subtotal of Community Program Expenditures
Under $25M (n=70) $25M under $100M (n=161) $100M under $250M n=127)
$250M under $500M (n=61) Over $500M (n=29)
Figure 65 and Figure 66 illustrate there is considerable variation across the
revenue size categories regarding expenditures for the various components of
community programs.
Figure 67, below, shows the average and median percentages of total revenues
spent on community programs by revenue size.
82

Figure 67. Percentage of Total Revenue Spent on Community Programs by Revenue Size
(n=448)
0.90
1.19
0.88
0.56
0.68
0.94
0.21
0.22
0.21
0.28
0.17
0.22
0.00
0.20
0.40
0.60
0.80
1.00
1.20
1.40
Under
$25M
(n=70)
$25M
under
$100M
(n=161)
$100M
under
$250M
(n=127)
$250 M
under
$500M
(n=61)
Over
$500M
(n=29)
Totals
(n=448)
Revenue Size
Percentage of Total Revenue Spent
Average Median
8. Aggregate Community Benefit Expenditures by Revenue Size
As previously discussed, the entire respondent group reported aggregate
community benefit expenditures of $9.4 billion. These expenditures were not
evenly distributed by the hospitals in the study, but were concentrated in a
relatively small number of hospitals. 9% of the hospitals reported 60% of the
aggregate community benefit expenditures; 19% of the hospitals reported 78% of
the aggregate community benefit expenditures.
Figure 68 and Figure 69 show a breakout of the categories of community benefit
expenditures for five revenue categories of hospitals, and shows the differences
in community benefit expenditure profiles across the revenue size groups.
83

Figure 68. Amount and Percentage of Total Community Benefit Expenditures by
Expenditure Category and Revenue Size
Revenue Size
Under $25 M $25M to $100M to $250M to $500M and Aggregate
Community Under $100M Under 250M Under $500M Over
Benefit
(N = 485)
Expenditure
Amount % of Amount % of Amount % of Amount % of Amount % of Amount % of
(in $ total (in $ total (in $ total (in $ total (in $ total (in $ total
million) CBE million) CBE million) CBE million) CBE million) CBE million) CBE
▪ Uncompensated 104.2 93% 591.1 77% 1,316.9 74% 1,638.7 72% 1,576.5 35% 5,227.4 56%
Care
▪ Medical, 1.4 1% 41.8 5% 275.7 15% 445.3 19% 1,400.4 32% 2,164.6 23%
Education &
Training
▪ Medical
0.0 0.0% 11.0 1% 38.6 2% 90.0 4% 1,272.6 29% 1,412.2 15%
Research
▪ Community 6.5 6% 120.0 16% 155.1 9% 114.0 5% 194.4 4% 590.0 6%
Programs
Total Community
Benefit Expenditures
112.1 100% 763.9 100% 1,786.3 100% 2,288.0 100% 4,443.9 100% 9,394.2 100%
Figure 68 shows the distribution of reported community benefit expenditures
across the revenue size categories.
54
For example, hospitals with revenues
under $25 million comprised 17% of the hospitals, but reported 1% of aggregate
community benefit expenditures. Hospitals with revenues over $500 million
comprised 7% of the hospitals, but reported 47% of aggregate community benefit
expenditures.
54
The mix of community benefit expenditures changes when the group of 15 hospitals reporting
93% of aggregate reported medical research expenditures is isolated. See Section VI.B, below.
84
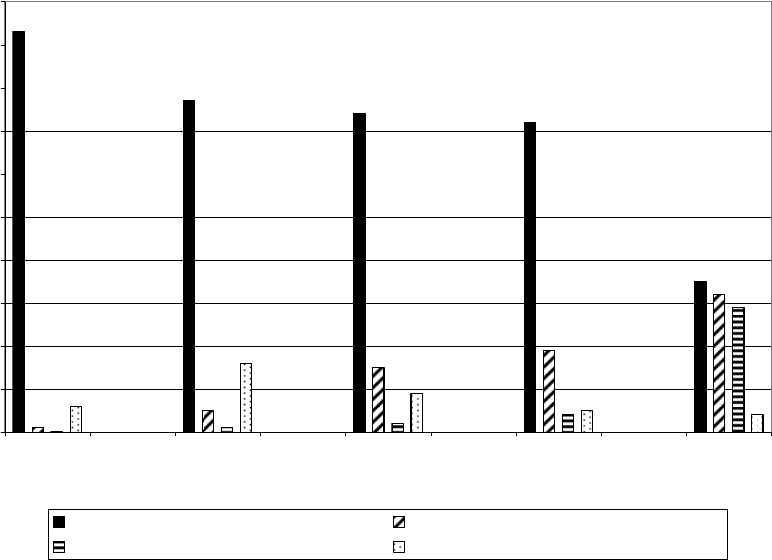
Figure 69. Percentage of Community Benefit Expenditures by Expenditure Category and
Revenue Size
(n=485)
93%
77%
74%
72%
35%
5%
15%
19%
32%
0%
1%
2%
4%
6%
16%
9%
5%
4%
1%
29%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Under $25M $25M under
$100M
$100M under
$250M
$250M under
$500M
Over $500M
Revenue Size
Percentage of Overall Community Benefit Expenditure
Uncompensated Care (n=466) Medical Education and Training (n=378)
Medical Research (n=104) Community Programs (n=448)
Uncompensated care as a percentage of aggregate community benefit
expenditures decreased as revenues increased. The smallest hospitals by total
annual revenue reported spending the largest percentage of their community
benefit expenditure dollars (93%) on uncompensated care. The largest hospitals
by total annual revenue reported spending the smallest percentage of their
community benefit expenditure dollars (35%) on uncompensated care. The three
middle categories are between these two percentages, ranging from 72% of
community benefit expenditure dollars reported as spent on uncompensated care
to 77% of community benefit expenditure dollars spent on uncompensated care.
Conversely, the largest hospitals by total annual revenue reported spending a
larger percentage of their community benefit expenditures on medical education
and training (32%) and on medical research (29%). The percentage of total
community benefit expenditure dollars reported as spent on medical education
and training increased (from 1% to 32%) as revenue size increased. The
percentage of total community benefit expenditure dollars reported as spent on
medical research also increased as revenue size increased.
85

Figure 70 and Figure 71, below, show the average and median percentage of
total revenue spent on community benefit expenditures by expenditure category
and revenue size.
55
Figure 70. Average and Median Percentage of Total Revenue Spent on Community Benefit
Expenditures by Expenditure Category and Revenue Size
Revenue Size
Category of Under $25 M $25M to $100M to $250M to $500M and Aggregate
Community Under $100M Under 250M Under $500M Over
Benefit
Expenditure
(N = 485)
Average Median Average Median Average Median Average Median Average Median Average Median
(%) (%) (%) (%) (%) (%) (%) (%) (%) (%) (%) (%)
·Uncompensated 9.33 3.12 6.63 3.18 6.44 4.33 8.47 5.53 5.62 4.68 7.21 3.88
Care (N=466)
·Medical Education 0.21 0.11 0.52 0.13 1.33 0.48 2.16 1.55 4.49 3.84 1.34 0.34
& Training (N=378)
·Medical Research
0.06 0.06 1.58 0.38 0.79 0.04 0.82 0.23 3.92 1.16 1.61 0.22
(N=104)
·Total Community
Program
0.90 0.21 1.19 0.22 0.88 0.21 0.56 0.28 0.68 0.17 0.94 0.22
Expenditures
(N=448)
Total Community
Benefit
Expenditures
9.86 3.36 8.00 3.98 8.43 6.04 11.31 8.92 12.42 10.54 9.18 5.50
55
The results change when the group of 15 hospitals that reported 93% of aggregate reported
medical research expenditures is isolated. See Section VI.B, below.
86

Figure 71. Average and Median Total Revenue Spent on Community Benefit Expenditures
by Expenditure and Revenue Size
(n=485)
10%
8% 8%
11%
12%
9%
3%
4%
6%
9%
11%
6%
0%
2%
4%
6%
8%
10%
12%
14%
Under
$25M
$25M
under
$100M
$100M -
under
$250M
$250M
under
$500M
Over
$500M
Total
Revenue Size
Percentage of Total Revenue Spent
Average Median
The average and median reported aggregate community benefit expenditures as
a percentage of total revenues were 9% and 6%, respectively, for the entire
group. The highest reported average and median amounts were for hospitals
with revenues over $500 million (12% and 11%, respectively). The median
percentages increased with revenue size, ranging from 3% for hospitals with
revenues under $25 million to 11% for hospitals with revenues over $500 million.
Figure 72 and Figure 73, below, show the average and median percentages of
total revenues spent on various community benefit expenditures by expenditure
and revenue size.
87

Figure 72. Percentage of Total Revenue Spent on Various Community Benefit
Expenditures by Expenditure and Revenue Size Categories
(Averages)
(n=485)
6.6%
6.4%
8.5%
5.6%
7.2%
0.5%
1.3%
4.5%
0.1%
0.8%
3.9%
1.6%
0.7%
9.9%
8.0%
8.4%
12.4%
9.2%
9.3%
0.2%
2.2%
1.3%
1.6%
0.8%
1.2%
0.9%
0.9%
0.9%
0.6%
11.3%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250 under
$500M
Over
$500M
Aggregate
Revenue Size
Average Percentage of Total Revenue Spent
Uncompensated Care (n=466) Medical Education and Training (n=378)
Medical Research (n=104) Total Community Program Expenditures(n=448)
Total CBE (n=485)
88
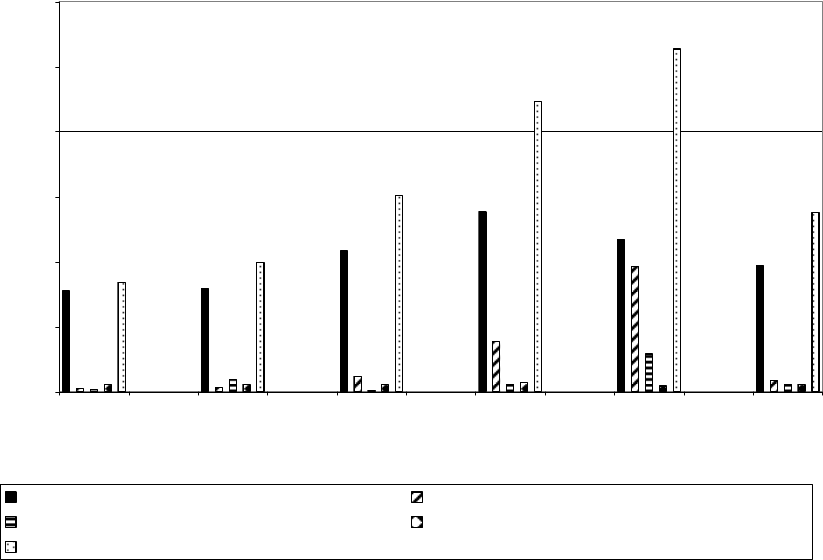
Figure 73. Percentage of Total Revenue Spent on Various Community Benefit
Expenditures by Expenditure and Revenue Size Categories
(Medians)
(n=485)
3.1%
3.2%
4.3%
5.5%
4.7%
3.9%
0.5%
1.6%
3.8%
0.3%
0.0%
1.2%
0.2%
0.2%
3.4%
4.0%
6.0%
8.9%
10.5%
5.5%
0.1% 0.1%
0.2%
0.2%
0.1%
0.4%
0.2%
0.3%
0.2%
0.2%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
Under
$25M
$25M
Under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Aggregate
Revenue Size
Median Percentage of Total Revenue Spent
Uncompensated Care (n=466) Medical Education and Training (n=378)
Medical Research (n=104) Total Community Program Expenditures (n=448)
Total CBE (n=485)
The figures above show that hospitals in the smallest revenue size category
(under $25 million) reported spending the largest average percentage of
revenues on uncompensated care and the smallest average percentage of
revenues for medical research. Hospitals in the largest revenue category
reported spending the smallest average percentage of revenues on
uncompensated care and the largest percentages on medical, education and
training and medical research compared with the other revenue categories.
9. Aggregate Community Benefit Expenditures as Percentage of
Revenues
This section summarizes the distribution of aggregate community benefit
reporting across revenue sizes. Figure 74, Figure 75, and Figure 76 show the
distribution of hospitals by revenue size, with reported community benefit
expenditures within specified percentages of total revenue ranges. Figure 77
displays the cumulative percentage of hospitals within each revenue size that
reported aggregate community benefit expenditures as a percentage of total
revenues, at or less than specified levels (e.g., less than 5% of total revenues).
The $250 million to under $500 million and $500 million and over categories were
combined in these figures to prevent potential identification of respondent
hospitals.
89

Figure 74. Number and Percentage of Hospitals with Reported Community Benefit
Expenditures as a Percentage of Total Revenue by Revenue Size
Revenue Size
Total Community
Benefit
Expenditure as
Percentage
< $25M
$25M - <
$100M
$100M - < $250M ≥ $250M
Overall
of Total Revenues
N % N % N % N % N %
< 2% * 34 * 30 16 12 5 5 101 21
2% - < 5% * 26 * 26 40 30 21 22 128 26
5% - < 10% * 17 * 23 35 26 25 26 113 23
10% - < 20% * 13 * 13 30 23 35 36 99 21
≥ 20% * 10 * 8 12 9 11 11 44 9
Total * 100 * 100 133 100 97 100 485 100
* Not shown to prevent potential identification of respondent hospitals.
Figure 74, above, shows that in the two smallest revenue categories (under $100
million), 60% and 56% of the hospitals, respectively, reported spending less than
5% of total revenues on community benefit expenditures. Overall, 47% of all
hospitals reported spending less than 5% of total revenues on community benefit
expenditures.
Figure 75. Percentage of Hospitals with Reported Community Benefit Expenditures as a
Percentage of Total Revenue by Revenue Size
(n=485)
34%
17%
10%
30%
26%
23%
13%
8%
12%
30%
26%
9%
5%
22%
36%
11%
21%
26%
21%
9%
13%
26%
23%
26%
23%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Under 2% 2.0% Under
5.0%
5.0% Under
10.0%
10.0 % Under
20.0%
Over 20.0%
Percentage of Total Revenue Ranges
Percentage of Hospitals
Under $25M $25M under $100M $100M under $250M Over $250M Total
90

Figure 76. Percentage of Hospitals with Reported Community Benefit Expenditures as a
Percentage of Total Revenue by Revenue Size
(n=485)
30%
5%
21%
26%
30%
23%
36%
21%
8%
9%
11%
12%
34%
26%
22%
26%
26%
26%
23%
17%
23%
13%
13%
10%
9%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Under $25M $25M under
$100M
$100M under
$250M
Over $250M Total
Total Revenue Categories
Percentage of Hospitals
Under 2% 2.0% Under 5.0% 5.0% under 10.0% 10.0% Under 20.0% Over 20.0%
A relatively large percentage of hospitals in the over $250 million revenue size
category reported total community benefit expenditures of more than 10% of total
revenues (47% compared with 30% for all hospitals).
Figure 77, below, shows, on a cumulative basis, the percentage of hospitals
reporting community benefit expenditures at or less than specified percentages
of revenue levels.
Figure 77. Percentage of Hospitals Reporting Community Benefit Expenditures at or Less
Than Specified Percentages of Revenue Levels
Revenue Size <2% <5% <10%
Under $25 million 34% 60% 77%
$25 million to under $100 million 30% 56% 79%
$100 million to under $250 million 12% 42% 68%
$250 million and over 5% 27% 53%
Total 21% 47% 70%
Figure 77 shows that 21% of all hospitals reported spending less than 2% of total
revenues on aggregate community benefit expenditures; 47% reported spending
less than 5% of total revenues on community benefit expenditures. The larger
hospital categories included lower percentages of hospitals that reported
community benefit expenditures at the under 2% and under 5% of revenue
levels. The smallest hospital groups included the highest percentages of
91
hospitals that reported community benefit expenditures below the 2% and 5% of
revenue levels.
92
VI. OTHER COMMUNITY BENEFIT REPORTING - BAD DEBT AND
SHORTFALLS, RESEARCH, INCOME AND HEALTH INSURANCE
COVERAGE LEVELS
A. Overview and Summary of Key Findings
Section VI summarizes the study’s other demographic breakdowns of
uncompensated care and community benefit expenditures. Section VI.B reports
certain community benefit expenditure data for the group of 15 hospitals that
reported 93% of the medical research expenditures, and analyzes the impact this
group had on the overall results. Section VI.C provides uncompensated care
breakdowns by community type and revenue size and analyzes reporting
differences depending on whether shortfalls and bad debt are included in
uncompensated care. Section VI.D includes a discussion of reported community
benefit expenditures depending upon per capita income and insurance coverage
levels in the communities surrounding the respondent hospitals.
The key findings of this section are:
1. A group of 15 hospitals, comprising 3% of all hospitals in the study,
reported 93% of aggregate medical research expenditures and 58% of
aggregate medical education and training expenditures reported by all
hospitals in the study. These hospitals had a materially different
community benefit mix than did the other hospitals, with medical research
expenditures comprising 45% of their total community benefit
expenditures, followed by medical education and training (28%),
uncompensated care (22%), and community programs (5%). Although
this group of 15 hospitals reported lower uncompensated care
expenditures as a percentage of revenue than the overall group (6%
average and 3% median, respectively, compared to 7% and 4%,
respectively, for the overall group), it reported higher community benefit
expenditures as a percentage of revenue than the overall group (19%
average and median, respectively, compared to 9% and 6%, respectively,
for the overall group).
2. Greater percentages of hospitals reported including bad debts and self
pay shortfalls in uncompensated care than any other types of shortfalls.
This was the case overall and for each community type and revenue size.
3. Rural hospitals (CAH and non-CAH) reported higher percentages of
hospitals including private insurance and self pay shortfalls in
uncompensated care than did the other community types. Urban and
suburban hospitals (high population and other) reported higher
percentages of hospitals including bad debt in uncompensated care.
93
4. The treatment of bad debt as uncompensated care varied slightly more
across revenue size categories than it did across community types. The
treatment of a particular shortfall as uncompensated care varied more
across community types than across revenue size categories.
5. The study did not obtain information regarding the breakdown of reported
uncompensated care amounts across bad debt or specific types of
shortfalls. Accordingly, the study does not assess the impact that uniform
treatment by all respondent hospitals would have on the uncompensated
care or aggregate community benefit expenditure levels of the overall
group or across the community types or revenue size categories.
6. The study did not find a correlation between community benefit
expenditure levels and per capita income levels of the area surrounding
the hospital. The average and median percentages of revenues spent on
uncompensated care by the hospitals in the low per capita income
categories were less than those reported by the overall group, and
generally were less than those reported by hospitals in areas with per
capita incomes at or above state or federal averages.
7. The study suggests a correlation between community benefit expenditure
levels and the health insurance coverage levels of the area surrounding
the hospital. The average and median percentages of total revenues
reported as spent on community benefit expenditures increased as the
surrounding area’s health coverage level decreased (uninsured rate
increased). The percentage of hospitals reporting spending more than 5%
of total revenues on community benefit expenditures also increased as
health insurance coverage levels decreased (uninsured rates increased).
B. Hospitals Reporting Largest Amounts of Medical Research
Expenditures
A group of 15 hospitals, comprising 3% of the hospitals, reported 93% of
aggregate medical research expenditures. Each of these hospitals reported
more than $10 million in medical research expenditures.
For purposes of this section, this group of 15 is referred to as “research
hospitals”. The classification is not dependent on whether the hospital considers
itself a research hospital. As the case with the report in general, this data has
limited use for several reasons, including the relatively small size of this group,
that the information reported was not independently verified, and the different
measurements and components of uncompensated care included by the
respondent hospitals. A material percentage of this group was children’s
hospitals which also impacted the results.
94

The average and median medical research expenditure amounts of the 15
medical research hospitals ($87.9 million and $44.9 million, respectively) were
significantly higher than those reported by the remaining 89 hospitals reporting
medical research expenditure amounts ($1 million and $0.3 million, respectively).
The average and median percentages of revenue reported as spent on medical
research by the medical research hospitals (8.3% and 7.1% respectively) were
higher than that reported by the other hospitals (0.5% and 0.1%, respectively)
and the overall group (1.6% and 0.2%, respectively).
Patient insurance coverage. In general, the research hospitals reported a higher
percentage of patients with private insurance (49%) and a lower percentage of
patients with Medicare (16%). The lower percentage of Medicare, approximately
half that of the overall group, may be affected by the material percentage of
children’s hospitals included in the group.
Community benefit expenditures mix. The chart below compares the community
benefit expenditure mix of the group of 15 hospitals to the mix of all other
hospitals in the study, then to the overall group.
95

Figure 78. Community Benefit Expenditure Mix
22%
71%
56%
28%
21%
23%
45%
1%
15%
5%
7%
6%
0%
10%
20%
30%
40%
50%
60%
70%
80%
Medical Research Hospitals Other Overall
Hospital Category
Percentage of Overall Community Benefit Expenditures
Uncompensated Care Medical Education & Training
Medical Research Community Programs
The group of 15 research hospitals is the only demographic in the study that
did not report uncompensated care as its largest component of community
benefit expenditures. When the group of 15 research hospitals was removed
from the overall group, the overall mix changed, with uncompensated care
increasing from 56% to 71%, and medical research decreasing from 15% to
1% of aggregate reported community benefit expenditures.
Percentage of revenues spent on other components of community benefit.
• Uncompensated care: Three research hospitals reported no
uncompensated care amounts. The average and median percentages of
revenues reported as spent on uncompensated care by the group of
medical research hospitals that reported uncompensated care
expenditures (6.2% and 3.3%, respectively) were less than the average
and median for the other hospitals and the overall group (both 7.2% and
3.9%, respectively).
96

• Medical education and training: The medical research hospitals
reported 58% of the aggregate medical education and training
expenditures reported overall. The average and median percentages of
revenues reported as spent on medical education and training by the
medical research hospitals (4.9% and 3.8%, respectively) were higher
than reported by the other hospitals (1.2% and 0.3%, respectively) and the
overall group (1.3% and 0.3% respectively).
• Community program expenditures: The average percentage of
revenues reported as spent on community program expenditures was
similar to the other hospitals and the overall group. The median was
significantly less (.03% in the case of medical research hospitals and 0.2%
for other hospitals and overall).
Aggregate community benefit expenditures. The average and median
percentages of revenues reported as spent on community benefit expenditures
by the medical research hospitals (19% for both) were higher than reported by
the other hospitals (9% and 5%, respectively) and the overall group (9% and 6%,
respectively).
Excess revenues. The medical research hospitals reported higher average and
median annual total revenues as well as average and median excess revenue
amounts.
Figure 79. Annual Total Revenues, Total Expenses, and Excess/Deficit Revenues
Annual Total Revenues Annual Total Expenses Annual Excess/Deficit Revenue
Aggregate Average Median Aggregate Average Median Aggregate Average Median
Hospital
Category
(Billion $) (Million $) (Million $) (Billion $) (Million $) (Million $) (Billion $) (Million $) (Million $)
Medical
Research
(N = 15)
15.3 1,021.7 995.2 14.3 952.4 913.6 1.0 69.4 57.9
Other
(N = 473)
72.2 152.6 85.1 69.2 146.3 83.2 3.0 6.4 2.3
Total
(N = 488)
87.5 179.4 89.4 83.5 171.0 87.1 4.1 8.3 2.5
The aggregate excess revenues as a percentage of total revenues was 6.8% for
the research hospitals, compared to 4.6% for the overall group. Eight of the 15
hospitals reported a deficit or positive excess revenues less than 5% of total
revenues. Seven reported excess revenues as a percentage of revenues greater
than 5%.
Percentage of hospitals with uncompensated care and community benefit
expenditures at or less than certain revenue levels. All 15 medical research
hospitals reported community benefit expenditures greater than 5% of revenues.
40% reported community benefit expenditures greater than 20%. Three
hospitals reported no uncompensated care expenditures. Of the remaining
hospitals in the group, four reported uncompensated care expenditures in each
of the following ranges: over 1% and ≤3%; over 3% and ≤5%; over 5%.
97

C. Analysis of Bad Debt and Shortfalls as Uncompensated Care
1. Reporting of Shortfalls and Bad Debt by Community Type
Between 18% and 20% of hospitals reported that they included the following
items in their calculation of uncompensated care: the difference between hospital
charges and the amount private insurance paid or allowed for services (private
insurance shortfalls); the difference between hospital charges and the amount
Medicare paid or allowed for services (Medicare shortfalls); the difference
between hospital charges and the amount Medicaid allowed for services
(Medicaid shortfalls); and the difference between hospital charges and the
amount other public insurance programs allowed for services (other public
program shortfalls). 51% of hospitals reported that they included the difference
between hospital charges and the amount paid by individuals without insurance
in their calculation of uncompensated care (self pay shortfalls). 44% of the
hospitals reported including bad debt in uncompensated care.
Figure 80 below shows the percentage of hospitals in each community type that
reported including these various amounts in uncompensated care.
Figure 80. Percentage of Hospitals that Include Various Shortfall Amounts or Bad Debt in
Uncompensated Care by Community Type
(n=489)
12%
28%
31%
15%
14%
28%
16%
19%
14%
22%
32%
14%
47%
53%
62%
47%
51%
44%
19%
19%
20%
24%
20%
18%
34%
18%
34%
48%
35%
47%
0%
10%
20%
30%
40%
50%
60%
70%
High
Population
(n=94)
Critical
Access (n=68)
Rural Non-
CAH (n=78)
Other (n=249) Totals (n=489)
Community Type
% of Hospitals Including Shortfalls or Bad Debts
Private Insurance (n=483) Medicare (n=483) Medicaid (n=484)
Other Public Insurance (N=483) Self Pay (n=479) Bad Debts (n=482)
98

In all categories, fewer hospitals reported including Medicare and Medicaid
shortfalls than reported including self pay shortfalls and bad debt in
uncompensated care. In most cases, the percentage of hospitals that reported
including self pay shortfalls in uncompensated care was more than twice the
percentage of hospitals that reported including Medicare, Medicaid, private
insurance or other public program shortfalls in uncompensated care. A lower
percentage of hospitals in both groups of rural hospitals reported including bad
debt in uncompensated care (34% for CAHs and 35% for non-CAH rural) than
was included by the other groups (47% for high population areas and 48% for
other urban and suburban hospitals). A greater percentage of rural hospitals
(28% for CAHs and 31% for non-CAHs) as compared with the other groups (12%
for high population and 15% for other urban and suburban) reported including
private insurance shortfalls in uncompensated care.
Figure 81 displays the results grouped by type of shortfall or bad debt instead of
by community type.
Figure 81. Percentage of Hospitals that Include Various Shortfall Amounts or Bad Debt in
Uncompensated Care by Type of Coverage
(n=489)
12%
14%
16%
14%
47% 47%
28%
24%
19%
22%
53%
31%
28%
34%
32%
62%
14%
47%
48%
18%
51%
44%
34%
35%
18%
19%
15%
20%
20%
19%
0%
10%
20%
30%
40%
50%
60%
70%
Private
Insurance
Medicare Medicaid Other
Public
Insurance
Self Pay Bad Debts
Types of Insurance
% of Hospitals Including Shortfalls or Bad Debts
High Population (n=94) Critical Access (n=68) Rural Non-CAH (n=78)
Other (n=249) Total (n=489)
The figure shows that greater percentages of hospitals across all community
types reported including shortfalls from self pay patients and bad debt than from
Medicare and Medicaid.
The following highlights various reported components of uncompensated care.
99
• Bad debt as uncompensated care: A smaller percentage of both groups
of rural hospitals reported including bad debt in uncompensated care
compared with the other groups.
• Medicare shortfalls as uncompensated care: A larger percentage of
both groups of rural hospitals reported including the difference between
hospital charges and the amount Medicare paid or allowed for services in
uncompensated care compared with the other groups.
• Medicaid shortfalls as uncompensated care: Non-CAH rural hospitals
reported the highest percentage of hospitals including the difference
between hospital charges and the amount Medicaid paid or allowed for
services in uncompensated care. The amount reported by non-CAH rural
hospitals (34%) is much higher than reported by any other group.
• Other public insurance shortfalls (other than Medicare and Medicaid)
in uncompensated care: A higher percentage of both types of rural
hospitals (CAH and non-CAH) reported including the difference between
hospital charges and the amount other public insurance programs paid or
allowed in uncompensated care compared with the other groups.
• Self pay shortfalls as uncompensated care: At least 47% of the
hospitals in each community type reported including the difference
between hospital charges and the amount paid by self-pay patients for
services as uncompensated care. Hospitals in the rural-non CAH
category reported the highest percentage (62%).
• Private insurance shortfalls as uncompensated care: The percentage
of rural hospitals that reported including the difference between hospital
charges and the amount private insurance paid or allowed for services in
uncompensated care was higher than that reported by hospitals in the
other groups.
2. Reporting of Shortfalls and Bad Debt by Revenue Size
Figure 82 shows the percentage of hospitals in various revenue size categories
that reported including shortfall amounts or bad debt in uncompensated care.
The two largest revenue sizes ($250 million to $500 million and over $500
million) were combined to prevent potential identification of respondent hospitals.
100

Figure 82. Percentage of Hospitals that Include Various Shortfall Amounts or Bad Debt in
Uncompensated Care by Revenue Size
(n=489)
24%
16%
19%
18%
19%
20%
21%
19%
20%
21%
20%
21%
17% 17%
19%
18%
55%
47%
50%
53%
51%
35%
48%
58%
44%
19%
18%
19%
27%
41%
0%
10%
20%
30%
40%
50%
60%
70%
Under $25M $25M under
$100M
$100M under
$250M
Over $250M Totals
% of Hospitals Including Shortfalls or Bad Debts
Private Insurance (n=483) Medicare (n=483) Medicaid (n=484)
Other Public Insurance (n=483) Self Pay (n=479) Bad Debts (n=482)
Figure 82 shows that the percentage of hospitals that reported including
Medicare or Medicaid shortfalls was materially less than the percentage that
reported including shortfalls from self pay patients or bad debt. This variance
was more pronounced in hospitals that reported total revenues of more than
$250 million, but was less pronounced in hospitals that reported total revenues
under $25 million. Although not displayed in these figures to prevent potential
identification of respondent hospitals, hospitals in the over $500 million revenue
size had the highest percentage of hospitals including bad debt in
uncompensated care and the smallest percentages of hospitals including private
insurance, Medicare, Medicaid, or other public insurance in uncompensated
care.
Figure 83 displays the results grouped by type of shortfall or bad debt instead of
by revenue size.
101

Figure 83. Percentage of Hospitals that Include Various Shortfall Amounts or Bad Debt in
Uncompensated Care by Type of Shortfall or Bad Debt
(n=489)
24%
27%
21%
55%
41%
19%
17%
47%
35%
50%
48%
19% 19%
53%
58%
19%
20%
44%
21%
19%
19%
17%
18%
20%
18%
21%
16%
18%
20%
51%
0%
10%
20%
30%
40%
50%
60%
70%
Private
Insurance
(n=483)
Medicare
(n=483)
Medicaid
(n=484)
Other
Public
Insurance
(n=483)
Self Pay
(n=479)
Bad Debts
(n=482)
% of Hospitals Including Shortfalls or Bad Debts
Under $25M $25M under $100M $100M under $250M Over $250M Totals
The following highlights various reported components of uncompensated care.
• Bad debt as uncompensated care: By revenue size, with the exception
of the under $25 million group, the percentage of hospitals including bad
debt in uncompensated care increased as hospital size increased.
• Medicare shortfalls as uncompensated care: Hospitals in the under
$25 million revenue category reported the highest percentage including
Medicare shortfalls in uncompensated care. Although not displayed in the
figures to prevent potential identification of respondent hospitals, the
percentage of hospitals in the over $500 million revenue category was
lower than that reported by all other groups.
• Medicaid shortfalls as uncompensated care: Although not displayed in
the figures to prevent potential identification of respondent hospitals,
hospitals in the $250 million to under $500 million revenue category
reported the highest percentage of hospitals including Medicaid shortfalls
in uncompensated care. Hospitals in the over $500 million revenue
category reported a smaller percentage compared with the other groups.
The percentage reported by the remaining groups was very similar.
102
• Other public insurance shortfalls (other than Medicare and Medicaid)
in uncompensated care: Hospitals in the $25 million to under $250
million revenue categories reported percentages very similar to the total
group. Although not displayed in the figures to prevent potential
identification of respondent hospitals, hospitals in the largest revenue
category (over $500 million) reported a smaller percentage of hospitals
including other public insurance shortfalls in uncompensated care.
• Self pay shortfalls as uncompensated care: By revenue size
categories, the percentages reported by the groups were similar, ranging
from 47% ($25 million to under $100 million) to 55% (under $25 million).
• Private insurance shortfalls as uncompensated care: With the
exception of the over $500 million revenue category, the percentage of
hospitals that reported including private insurance shortfalls was similar
ranging from 18% to 24%. Although not displayed in the figures to prevent
potential identification of respondent hospitals, the percentage reported by
the over $500 million category was smaller (9%).
3. Reporting Differences when Shortfalls and Bad Debt are Included
in Uncompensated Care
This section compares aggregate uncompensated care amounts reported by
hospitals depending upon whether they included or excluded particular items of
uncompensated care.
Figure 84, below, shows the median percentage of revenue reported as spent on
all uncompensated care, depending on whether the hospital included or excluded
the relevant shortfall or bad debt expense in uncompensated care. For example,
the first two bars in the chart show that for the 92 hospitals that reported
including private insurance shortfalls in uncompensated care, the median
percentages of aggregate reported uncompensated care as a percentage of total
revenues was 3.1%, contrasted with a median of 3.7% for the 391 hospitals that
did not include private insurance shortfalls in uncompensated care.
The median percentage of revenues reported as spent on uncompensated care
was relatively similar for respondents that reported including payment shortfalls
from private insurance, Medicare, other public insurance, and individuals without
insurance in their calculation of uncompensated care and those that did not.
However, greater differences are shown in the median percentage of revenue
reported as spent on uncompensated care, depending upon whether
organizations included Medicaid shortfalls or bad debt expense in
uncompensated care.
103
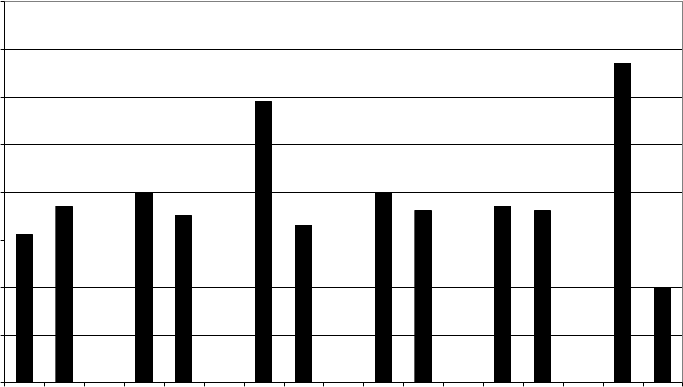
Figure 84. Reporting Differences When Shortfalls and Bad Debt are Included in
Uncompensated Care
(Median % of Revenue Spent)
3.1%
3.7%
4.0%
3.5%
5.9%
3.3%
4.0%
3.6%
3.7%
3.6%
6.7%
2.0%
0.0%
1.0%
2.0%
3.0%
4.0%
5.0%
6.0%
7.0%
8.0%
Private Insurance - Yes (n=92
)
Pri
v
a
t
e I
n
s
u
ran
c
e
- No
(
n=39
1
)
Medicare - Yes (n=98)
Medi
c
are
-
No (n=385)
Med
ic
a
id
-
Y
es
(n
=98
)
Me
dicaid
- N
o
(
n=38
6
)
O
t
h
er Pu
bl
ic
Insur
an
c
e -
Y
es
(n
=8
6)
O
t
he
r Pu
bli
c
Insura
nce
-
No (n= 39
7)
Sel
f
-Pay
- Ye
s
(n=242)
Self-Pay (n=237)
Bad
debt - Yes (n=2
1
3)
Bad
debt - No (n=269)
Median % of Total Revenue
Spent on Uncompensated Care
The median percentage of revenue reported as spent on uncompensated care of
respondents that included the difference between what Medicaid paid or allowed
for services and hospital charges reported was 5.9% while the median
percentage of those that did not include these amounts was 3.3%. The median
percentage of revenue reported as spent on uncompensated care of respondents
that included bad debt expense in uncompensated care was 6.7% while the
median percentage of those that did not include bad debt in uncompensated care
was 2%.
Figure 85 shows the average percentage of revenue reported as spent on
uncompensated care was relatively similar for respondents that reported
including payment shortfalls from private insurance, other public insurance, and
individuals without insurance, in their calculation of uncompensated care and
those that did not. However, greater differences are shown in the average
percentage of revenue reported as spent on uncompensated care, depending on
whether organizations included shortfalls from Medicare, Medicaid or bad debt
expense in uncompensated care.
104

Figure 85. Reporting Differences When Shortfalls and Bad Debts are Included in
Uncompensated Care
(Average % of Revenue Spent)
7.0%
6.9%
11.6%
5.6%
12.5%
5.5%
7.7%
6.8% 6.8%
7.1%
9.7%
4.8%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
P
rivate
I
n
s
u
ra
nce -
Y
es
(n
=92
)
P
ri
v
a
t
e I
nsur
an
c
e
-
No
(n
=39
1)
Me
dicare
- Ye
s
(n=9
8
)
M
e
di
c
ar
e -
No (n=3
85
)
Me
d
ic
a
id -
Y
es
(n
=98)
Medicaid - No (n=386)
O
ther Pub
l
ic
Insurance
- Ye
s
(n=86)
Ot
h
er Pu
b
lic Insura
n
c
e
-
No (n=397)
S
efl-P
a
y
- Ye
s
(n=2
4
2)
S
el
f
-P
ay
-
No (n=
23
7)
B
ad de
b
t
- Yes (n=21
3
)
B
ad de
b
t
- N
o
(
n=26
9
)
Average % of Total Revenue
Spent on Uncompensated Care
The average percentage of revenue spent on uncompensated care was higher
for respondents that reported including bad debt, Medicare, and Medicaid
shortfalls than for those that excluded such items.
D. Comparison of Community Benefit Expenditures Across Various
Income and Health Insurance Coverage Levels
1. Overview
This section examines whether there is a correlation between the level of
community benefit expenditure and the income or health insurance coverage
level of the community where the hospital is located. In looking at the
connection between income levels and community benefit expenditures, the
study focused on per capita income levels, using both a statewide and
nationwide comparison. The possible connection between community benefit
expenditures and health insurance coverage levels was also analyzed under two
approaches. The first looked at insurance coverage rates within counties. The
second compared the county coverage rate with coverage rates nationwide.
56
56
Two approaches were utilized to examine the possible connection between income and health
insurance coverage levels to gauge the validity of the results and to determine whether a different
methodology would produce materially different results.
105

2. Community Benefit Expenditures Across Community Per Capita
Income Levels
Demographic information was collected from the US Census Bureau for each of
the areas where the 485 respondent hospitals that reported community benefit
expenditures were located. This information was collected and tabulated both by
state and by county using the ZIP Code for each hospital’s address that was on
the questionnaire. Information collected included population, per capita
income,
57
levels of insurance coverage,
58
and percentage of the population living
in poverty.
Utilizing the information collected from the US Census Bureau, hospitals were
classified based upon the per capita income of the surrounding geographic area,
as designated by the county in which each hospital was located. Two different
methods were employed to divide the sample into per capita income categories.
State per capita income method
The first method categorized hospitals based on how the per capita income in its
county compared to the statewide per capita income (referred to as the “state per
capita income” method). Under the state per capita income method, the
hospitals were divided into the following categories:
• Below state average: includes respondents in counties where the per
capita income was more than 5% below the per capita income of the
corresponding state (276 hospitals);
• At state average: includes respondents in counties where the per capita
income was within 5% above or below the per capita income of the
corresponding state (89 hospitals); and
• Above state average: includes respondents in counties where the per
capita income was more than 5% higher than the per capita income of the
corresponding state (120 hospitals).
59
57
Per capita income information was drawn from the U.S. Census Bureau's 2000 Census of
Population and Housing. Per capita income is the average money income received in 1999
computed for every man, woman, and child in a geographic area. It is derived by dividing the total
income of all people 15 years old and over in a geographic area by total population in that area.
Income is not collected for people under 15 years old even though those people are included in
the denominator of per capita income.
58
Information on health coverage was drawn from the U.S. Census Bureau's 2000 Small Area
Health Insurance Estimates (SAHIE). The Census Bureau defines persons insured as those who
have health insurance coverage, including private health insurance, Medicaid, Medicare, and/or
State Children's Health Insurance Program (but not including the Indian Health Service). Persons
uninsured are those who are not categorized as insured through any of those programs. The
SAHIE are experimental estimates. The SAHIE is a new program at the Census Bureau and the
first ever set of estimates was released in July, 2005.
59
5% above or below was arbitrarily selected to represent a material deviation from the state
average. This resulted in a greater distribution of hospitals in the “below state average” group
than in the other groups. This might be the result of a study sample with a disproportionately
106

Figure 86, below, shows the percentage of total revenues reported as spent on
community benefit expenditures across per capita income categories under the
state per capita income method.
higher percentage of hospitals in areas with low per capita income amounts, or our selection of
5% as not accurately distinguishing “below” or “above” hospitals from the norm.
107

Figure 86. STATE PER CAPITA INCOME METHOD
Percentage of Total Revenues Spent on Community Benefit Expenditures
Across Various Per Capita Income Categories
(Averages and Medians)
8.6%
8.0%
10.4%
8.9%
4.7%
6.7%
5.7%
5.4%
0%
2%
4%
6%
8%
10%
12%
Per capita income below
state average (N = 276)
Per capita income at
state average (N = 89)
Per capita income above
state average (N = 120)
Overall (N = 485)
State Per Capita Income Category
Percentage of Total Revenues Spent on Community Benefit Expenditure
s
Average Median
The results indicate that hospitals in areas with per capita income above the
state average reported spending a higher percentage of their total revenue on
community benefit expenditures (average, 10.4% and median, 5.7%) than did
respondents in areas with per capita income below the state average (average,
8.6% and median, 4.7%). The average and median percentages for the overall
group of 485 hospitals were 8.9% and 5.4%, respectively.
108

Figure 87 illustrates the percentage of hospitals within each of various ranges of
total revenue spent on community benefit expenditures across the three per
capita income categories under the state per capita income method.
Figure 87. STATE PER CAPITA INCOME METHOD
Distribution of Community Benefit Expenditures Across Per Capita Income Categories
26%
16%
13%
21%
26%
24%
33%
27%
21%
27%
23%
23%
17%
29%
23%
21%
9%
5%
9%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Per capita income below
state average (N = 276)
Per capita income at state
average (N = 89)
Per capita income above
state average (N = 120)
Overall (N = 485)
State Per Capita Income Category
Percentage of Hospitals within Various Community Benefit Expenditure/Annual
Total Revenue Ranges
CBE < 2% 2% ≤ CBE < 5% 5% ≤ CBE < 10% 10% ≤ CBE < 20% CBE ≥ 20%
The chart does not show a clear correlation between per capita income and the
level of community benefit expenditure. The percentage of hospitals that
reported community benefit expenditures at less than 2% of revenues (i.e., the
lowest percentage of revenue category) was highest (26%) when per capita
income was below the state level and lowest (13%) when the per capita income
was above the state level.
109
U.S. per capita income method
The second approach used to classify hospitals into per capita income categories
was based on how the per capita income in the respondent’s county compared to
the per capita income of U.S. counties nationally (referred to as the “U.S. per
capita income” method). Under the U.S. per capita income method the hospitals
were divided into the following categories:
• Low per capita: includes respondents in counties where the per capita
income was in the bottom 25% of U.S. counties nationwide (120
hospitals);
• High per capita: includes respondents in counties where the per capita
income was in the top 25% of U.S. counties nationwide (121 hospitals);
and
• Average per capita: includes respondents in the remaining U.S. counties
that were not described in either of the above two categories (244
hospitals).
60
Figure 88 shows the percentage of total revenues spent on community benefit
expenditures across the per capita income categories under the U.S. per capita
income method.
60
This method forced a bell curve distribution to test whether the results would vary compared to
the state per capita income method.
110

Figure 88. U.S. PER CAPITA INCOME METHOD
Percentage of Annual Total Revenues Spent on Community Benefit Expenditures
Across Various Per Capita Income Categories
(Averages and Medians)
8.0%
9.4%
8.9%
8.9%
4.2%
5.9%
5.0%
5.4%
0%
1%
2%
3%
4%
5%
6%
7%
8%
9%
10%
Low per capita income
(N = 120)
Average per capita
income (N = 244)
High per capita income
(N = 121)
Overall (N = 485)
U.S. Per Capita Income Category
Percentage of Total Revenues Spent on Community Benefit Expenditures
Average Median
The chart shows relatively similar percentages for each group. The results
indicate that respondent hospitals in areas with low per capita income under the
U.S. per capita income method reported spending a slightly lower percentage of
111
their total revenue on community benefit expenditures (average, 8.0% and
median, 4.2%) than did respondents in either of the two other per capita income
categories. These results differed somewhat from those under the state per
capita income method under which the amount of community benefit expenditure
by the hospitals with per capita income below the state level was very similar to
that of the overall group. The state per capita income method also showed a
less uniform distribution in the averages and medians for the various groups than
the chart above.
Figure 89 illustrates the percentage of hospitals that fall into various ranges of
total revenue spent on community benefit expenditures across the three U.S. per
capita income categories.
112

Figure 89. U.S. PER CAPITA INCOME METHOD
Distribution of Community Benefit Expenditures Across Per Capita Income Categories
30%
18%
19%
21%
23%
28%
30%
27%
23%
25%
19%
23%
15%
22%
24%
21%
9%
8%
8%
8%
0%
5%
10%
15%
20%
25%
30%
35%
Low per capita income
(N = 120)
Average per capita
income (N = 244)
High per capita income
(N = 121)
Overall (N = 485)
U.S. Per Capita Income Category
Percentage of Hospitals within Various Community Benefit Expenditure/Annual Total Revenue
s
Ranges
CBE < 2% 2% ≤ CBE < 5% 5% ≤ CBE < 10% 10% ≤ CBE < 20% CBE ≥ 20%
This chart illustrates a similarity among all three categories in the percentage of
hospitals that reported spending 20% or more of total revenue on community
benefit expenditures (8%-9%). The percentage of hospitals that reported
spending less than 2% of total revenues on uncompensated care was highest for
hospitals in the low per capita income categories. This is consistent with the state
per capita income method.
113

Based on the reported data, both the state and U.S. per capita income method
suggest that there does not appear to be a correlation in the study group
between per capita income of the surrounding area and the amount of
community benefit expenditures incurred by the hospital.
3. Community Benefit Expenditures Across Community Health
Insurance Coverage Levels
This section analyzes the extent to which aggregate community benefit
expenditures varied depending upon the insurance coverage levels (uninsured
rate) of the hospital’s surrounding area.
Hospitals were analyzed based upon levels of insurance coverage in the county
where the hospital is located. Two different methods were employed to divide the
sample into insurance coverage rate categories. Both methods categorize
respondents into three categories: high, medium, and low health coverage rates.
County uninsured rate method
Under the first method (referred to as the “county uninsured rate” method),
hospitals were divided into the following categories based on the uninsurance
rate of the county where located:
• Low health coverage rate: includes counties where more than 13% of
the population was uninsured (152 hospitals);
• Medium health coverage rate: includes counties where between 9% and
13% of the population was uninsured (228 hospitals); and
• High health coverage rate: includes counties where less than 9% of the
population was uninsured (105 hospitals).
61
Figure 90 shows the percentage of revenues spent on community benefit
expenditures by hospitals as categorized under the county uninsured rate
method.
61
The coverage rates were selected based on the distribution of the coverage rates of the
counties of the hospitals in the study.
114

Figure 90. COUNTY UNINSURED RATE METHOD
Percentage of Annual Total Revenues Spent on Community Benefit Expenditures
Across Health Coverage Categories
(Averages and Medians)
11.1%
8.3%
7.2%
8.9%
7.4%
5.0%
4.1%
5.4%
0%
2%
4%
6%
8%
10%
12%
Low health coverage
rate (N = 152)
Medium health coverage
rate (N = 228)
High health coverage
rate (N = 105)
Overall (N = 485)
County Health Coverage Rate Category
Percentage of Total Revenues Spent on Community Benefit Expenditure
s
Average Median
The results indicate that respondents in areas with low health coverage rates
(higher uninsured rates) reported higher levels of community benefit
expenditures. Under this method, the percentage of revenues reported as spent
on community benefit expenditures increased as the percentage of uninsured
individuals increased. Hospitals in low health coverage areas (higher uninsured
rates) reported an average community benefit expenditure amount of 11.1% of
their total revenue (median 7.4%) while hospitals in high health coverage areas
115

(lower uninsured rates) reported an average community benefit expenditure of
7.2% of total revenue (median 4.1%).
Figure 91 further illustrates the distribution of hospitals within varying community
benefit expenditures across the different county health coverage rates under the
county uninsured rate method.
Figure 91. COUNTY UNINSURED RATE METHOD
Distribution of Community Benefit Expenditures Across Health Coverage Categories
13%
24%
26%
21%
25%
26%
33%
27%
24%
24%
18%
23%
23%
22%
16%
21%
15%
5%
7%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Low health coverage
rate (N = 152)
Medium health coverage
rate (N = 228)
High health coverage rate
(N = 105)
Overall (N = 485)
County Health Coverage Rate Category
Percentage of Hospitals within Various Community Benefit Expenditure/Annual
Total Revenue Ranges
CBE < 2% 2% ≤ CBE < 5% 5% ≤ CBE < 10% 10% ≤ CBE < 20% CBE ≥ 20%
The chart shows that the low health coverage group reported a higher
percentage of hospitals spending at least 20% of revenues on community benefit
116

expenditures. The largest percentage of hospitals spending less than 2% of
revenues on community benefit expenditures was in the high health coverage
(lower uninsured rates) group. The percentage of hospitals reporting <5% of
total revenues on community benefit expenditures decreased as insurance
coverage levels decreased. These results suggest a connection between
community benefit expenditure levels and the uninsured rate of the area
surrounding the hospital (i.e., expenditures generally increased as the uninsured
rate increased).
Nationwide comparison method
The second method used to assess the possible correlation of community benefit
expenditures to health insurance coverage levels categorized the hospitals by
comparing the county’s percentage of insured individuals with the percentage for
counties nationwide (referred to as the “nationwide comparison method”). Under
this method, the communities were divided into the following three categories:
• Low health coverage rate: includes counties where the percentage of
the population insured was in the bottom 25% of counties nationwide (119
hospitals);
• High health coverage rate: includes counties where the percentage of
the population insured was in the top 25% of counties nationwide (118
hospitals); and
• Medium health coverage rate: includes the remaining counties that were
not included in either of the above two categories (248 hospitals).
62
Figure 92 reports the percentages of revenues spent on community benefit
expenditures across these health insurance coverage categories.
62
This method forced a bell curve distribution to test whether the results would vary compared to
the county uninsured rate method.
117

Figure 92. NATIONWIDE COMPARISON METHOD
Percentage of Annual Total Revenue Spent on Community Benefit Expenditures
Across Health Coverage Categories
(Averages and Medians)
8.6%
7.2%
8.9%
7.7%
5.4%
4.2%
5.4%
11.2%
0%
2%
4%
6%
8%
10%
12%
Low health coverage
rate (N = 119)
Medium health
coverage rate (N = 248)
High health coverage
rate (N = 118)
Overall (N = 485)
Nationwide Health Coverage Rate Category
Percentage of Total Revenues Spent on Community Benefit Expenditure
s
Averag e Median
The results under this method are similar to those under the county uninsured
rate method. As under the county uninsured rate method, the results indicate
that respondents in areas with low health coverage rates reported higher levels
of community benefit expenditures. Hospitals in low health coverage areas
118

reported an average community benefit expenditure amount of 11.2% of their
total revenue (median 7.7%) while hospitals in high health coverage areas
reported spending an average of 7.2% of their total revenue (median 4.2%) on
community benefit expenditures.
Figure 93 shows the distribution of hospitals by the health coverage rate category
determined under the nationwide comparison method and percentage of
revenues spent on community benefit expenditures.
Figure 93. NATIONWIDE COMPARISON METHOD
Distribution of Community Benefit Expenditures Across Health Coverage Categories
14%
23%
25%
21%
24%
26%
35%
27%
24%
23%
19%
23%
25%
21%
15%
21%
13%
6%
7%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Low health coverage rate
(N = 119)
Medium health coverage
rate (N = 248)
High health coverage rate
(N = 118)
Overall (N = 485)
Nationwide Health Coverage Rate Category
Percentage of Hospitals within Various Community Benefit Expenditure/Annual Total
Revenue Ranges
CBE < 2% 2% ≤ CBE < 5% 5% ≤ CBE < 10% 10% ≤ CBE < 20% CBE ≥ 20%
119

This distribution is similar to that under the county uninsured rate method. As the
charts above show, a greater percentage of hospitals in the low health coverage
rate category spent more than 20% of revenues on community benefit
expenditures. Hospitals in the high health coverage rate category had the
greatest percentage of hospitals that reported spending less than 5% of
revenues on community benefit expenditures. This was consistent with the
results under the county uninsured rate method, and suggests a connection
between community benefit expenditure levels and the uninsured rate of the area
surrounding the hospital (i.e., expenditures generally increased as the uninsured
rate increased).
4. Interaction Between Per Capita Income and Health Insurance
Coverage
The figures presented earlier in this section suggest that there does not appear
to be a correlation between per capita income and the aggregate amount of
community benefit expenditure for the various hospitals, but there does appear to
be a correlation between the amount spent on community benefit expenditures
and the health insurance coverage rate (or uninsured rate) of the surrounding
community.
63
The figures below show the distribution of the hospitals as categorized under the
per capita and health insurance coverage methods described above.
Figure 94 shows the distribution of the hospitals as categorized by the state per
capita income method and the two health insurance coverage categories. Figure
95 shows the distribution of the hospitals by the U.S. per capita income method
and the two health insurance coverage categories.
Figure 94. Distribution of Hospitals as Categorized by the State Per Capita Income Method
and Health Insurance Coverage Categories
Health Coverage under County Uninsured Rate
Method
Health Coverage under Nationwide Comparison
Method
State per
capita
income
Low health
coverage
rate
Medium
health
coverage
rate
High health
coverage
rate
Overall Low health
coverage
rate
Medium
health
coverage
rate
High health
coverage
rate
Overall
Below
state
level
91 140 45 276 73 148 55 276
At state
level
24 45 20 89 16 50 23 89
Above
state
level
37 43 40 120 30 50 40 120
Total 152 228 105 485 119 248 118 485
63
The study focused on comparing aggregate community benefit expenditures rather than on
components thereof, such as uncompensated care.
120

Figure 95. Distribution of Hospitals as Categorized by the U.S. Per Capita Income Method
and Health Insurance Coverage Categories
Health coverage under County Uninsured Rate
method
Health coverage under Nationwide Comparison
method
U.S. per
capita
income
Low health
coverage
rate
Medium
health
coverage
rate
High health
coverage
rate
Overall Low health
coverage
rate
Medium
health
coverage
rate
High health
coverage
rate
Overall
Low per
capita
55 56 9 120 49 61 10 120
Average
per capita
76 107 61 244 53 118 73 244
High per
capita
21 65 35 121 17 69 35 121
Total 152 228 105 485 119 248 118 485
121

VII. EXECUTIVE COMPENSATION
A. Overview
The executive compensation component of the study was twofold. It included an
analysis of the results of the executive compensation questions included in the
questionnaire. Section VII.B discusses these results. The executive
compensation component of the project also included examination of 20
hospitals from the study selected based, in part, on responses provided to the
questionnaire. These results are discussed in Section VII.C, below.
B. Summary of Compensation Practices as Reported by Responding
Hospitals
This section summarizes respondent data from Part III – Compensation Practices
of the questionnaire. Part III of the questionnaire requested information on the
compensation practices of the respondents with respect to their officers,
directors, trustees and key employees, and any business relationships with such
persons.
Not every hospital answered every question, and much of the data is based on
fewer than 489 responses. Throughout this section, the number of responses
that underlie the particular data are included.
64
Section 4958, the intermediate sanction on excess benefit transactions, provides
that an excess benefit transaction occurs when a disqualified person (any person
in a position to exercise substantial influence over the affairs of the tax exempt
organization) receives an economic benefit from an exempt organization that
exceeds the value of consideration received by the organization. Rather than
revoking the charity’s tax-exempt status, section 4958 allows the IRS to impose
an excise tax against the disqualified person and possibly the organization
manager. The section 4958 regulations provide a three-pronged rebuttable
presumption process (independent governing body, reliance on comparable data,
and adequate documentation) that public charities may use when establishing
what appropriate compensation is for a disqualified person.
65
While the questionnaire did not specifically ask about whether the hospitals were
using the rebuttable presumption, Questions 3 through 8 asked for information
relevant to the process. The responses to the questions asked (particularly
Question 3 and Question 8) indicate that use of the rebuttable presumption
appears to be widespread.
64
In some cases, the number of responses is not included to prevent potential identification of
respondent hospitals.
65
Treas. Reg. section 53.4958-6. See also, H. Rep. No. 104-506, 104
th
Cong., 2d Sess. at 56-57.
122
List and compensation of officers, directors, trustees, and key employees
(Question 1)
Question 1 asked the hospital to provide the names and titles of the hospital’s
officers, directors, trustees and key employees, and the amounts of salary and
other compensation paid to each. For this purpose, salary was described to
include all forms of cash and non-cash compensation received whether paid
currently or deferred. Other compensation was described to include
contributions to employee benefit plans and deferred compensation plans and
expense allowances from non-accountable plans.
There was some variation in the data reported on the questionnaires. While
many did provide information concerning all of their officers, directors, trustees
and key employees, others only provided information about some of those
individuals and a few provided no information. Hospitals that were part of
systems or had management companies frequently reported that some or all of
the compensation for their officers, directors, trustees and key employees was
paid by other entities, and in some instances reported those amounts and in
others did not. Thus, there are instances where the hospital identified its officers,
directors, trustees and key employees, but provided no compensation amounts.
There were also instances where the hospital reported compensation data, but
did not provide the individual’s positions.
Much of this variation in reporting is consistent with certain problems the IRS has
encountered generally with Form 990 reporting of executive compensation, in
particular, a lack of clarity regarding which persons to report, and how to report
compensation paid by certain other organizations. The changes made to the
redesigned Form 990 executive compensation reporting, including clearer
definitions of officer, director, trustee, and key employee, as well as reporting of
compensation paid by related or by other organizations and management
companies, will help improve uniform reporting in this area. The IRS
will follow-up with certain of these organizations through review by our Review of
Operations unit (ROO) after the redesigned Form 990 filings are received to
determine whether improvements have been made to the reporting of
compensation paid to top management officials and other executives.
While other compensation data was reviewed, such as Forms 990, to select
organizations for examination, the following analysis only includes data reported
on the questionnaire. The respondents' data was reviewed to determine the
average and median reported salary, other compensation, and total
compensation of the organizations' top management officials. The question
regarding compensation amounts for officers, directors, trustees, and key
employees did not ask the organizations to identify a top management official.
For this purpose, however, persons listed in the responses as "CEO" or "Chief
Executive Officer" were treated as the top management official. If no person was
listed as CEO or Chief Executive Officer, persons listed in the questionnaire
123
responses as "President," "Executive Director," or "Administrator" were treated
as the top management official.
Based on review of the responses, 421 of the respondents listed a person with a
title that, under the convention described above, was regarded as a top
management official and reported a compensation amount from all sources
greater than zero for such person. In 352 (84%) of those cases, the identified top
management official had the highest compensation reported on the questionnaire
for that hospital. The average and median salary paid to the top management
official were $408,927 and $323,858, respectively, while the average and median
other compensation were $81,504 and $34,611. When looking at total
compensation paid to the top management official, the average and median were
$490,431 and $377,256, respectively.
The identified top management official had the highest compensation reported on
the questionnaire for 75% of the critical access hospitals, compared to 85% for
the other three community types. Across revenue size, the hospitals reported
paying the identified top management official the highest compensation as
follows:
Under $25 million 72%
$25 - $100 million 84%
$100 - $250 million 92%
$250 - $500 million 87%
Over $500 million 71%
The average and median salary, other compensation, and total compensation
was lower for the rural hospitals (CAH and non-CAH) than for the suburban and
urban hospitals (high population and other urban and suburban). Among the
community types, critical access hospitals had the lowest average compensation
amounts and the hospitals in the highest population areas had the highest
average compensation amounts. The average and median salary, other
compensation, and total compensation increased as revenue levels increased.
The following charts show the average and median salary and other
compensation reported for the top management official, by community type and
then by revenue size.
124

Figure 96. Salary and Other Compensation Reported for the Top Management Official
by Community Type
(Average and Median)
$650.2
$152.6
$289.5
$427.5
$408.9
$480.2
$144.5
$234.3
$358.6
$323.9
$130.4
$25.0
$36.2
$93.0
$81.5
$55.6
$16.9
$19.1
$47.3
$34.6
$0.0
$100.0
$200.0
$300.0
$400.0
$500.0
$600.0
$700.0
$800.0
High
Population
Critical
Access
Hospitals
Rural - Non
CAH
Other Total
Compensation in Thousands
Average Salary Reported Median Salary Reported
Average Other Compensation Reported Median Other Compensation Reported
Figure 97. Salary and Other Compensation Reported for Top Management Official
by Revenue Size
(Average and Median)
$289.6
$465.3
$642.1
$877.2
$408.9
$125.8
$237.1
$401.1
$543.6
$700.1
$323.9
$88.5
$215.2
$81.5
$13.1
$24.5
$51.0
$85.0
$87.6
$34.6
$149.7
$48.2
$148.4
$21.3
$0.0
$100.0
$200.0
$300.0
$400.0
$500.0
$600.0
$700.0
$800.0
$900.0
$1,000.0
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
Compensation in Thousands
Average Salary Reported Median Salary Reported
Average Other Compensation Reported Median Other Compensation Reported
125

The following charts show the average and median total compensation reported
for the top management official, by community type and then by revenue size.
Figure 98. Total Compensation Reported for the Top Management Official
by Community Type
(Average and Median)
$177.6
$520.5
$490.4
$565.5
$169.0
$256.9
$425.9
$377.3
$325.7
$780.6
$0.0
$100.0
$200.0
$300.0
$400.0
$500.0
$600.0
$700.0
$800.0
$900.0
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Total Compensation in Thousandths
Average Median
126

Figure 99. Total Compensation Reported for Top Management Official
by Revenue Size
(Average and Median)
$337.8
$553.7
$790.5
$1,092.4
$490.4
$377.3
$171.0
$139.5
$263.4
$461.3
$642.4
$786.1
$0.0
$200.0
$400.0
$600.0
$800.0
$1,000.0
$1,200.0
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
Total Compensation in Thousandths
Average Median
Formal written compensation policy (Question 2)
Question 2 asked whether the hospital had a formal written compensation policy.
349 (73%) of 481 respondents reported having such a policy. This is generally
consistent across community types, ranging from 64% to 79% of the hospitals
having a formal written compensation policy. However, when looking at revenue
size, only 54% of the hospitals with revenues under $25 million had a formal
written compensation policy, while 87% of the hospitals with revenues between
$250 million and $500 million did. The following charts show the percentage of
hospitals that reported having a written compensation policy, first by community
type and then by revenue size.
127

Figure 100. Percentage of Hospitals that Reported Having a Written Compensation Policy
by Community Type
67%
64%
79%
75%
73%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Percentage of Hospitals
128

Figure 101. Percentage of Hospitals that Reported Having a Written Compensation Policy
by Revenue Size
54%
75%
74%
69%
73%
87%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
Percentage of Hospitals
Approval of compensation in advance (Question 3)
in advance by
at
ilar
rganization officials responsible for establishing compensation
ed who set the compensation for officers, directors, trustees, and
Question 3 asked whether compensation was approved
individuals that did not have a conflict of interest with the compensation
arrangement being approved. 469 (98%) of 479 respondents reported th
compensation was approved in advance by individuals that did not have a
conflict of interest with the compensation arrangement being approved. Sim
results were observed across community type and revenue size.
O
(Question 4)
Question 4 ask
key employees of the hospital – officers, the board of directors, a compensation
committee, or others. The organization was instructed to check all that applied.
For many respondents, compensation was determined by a combination of the
categories.
129

Figure 102. Individual or Entity Reported to Determine Compensation
(n=478)
31%
63%
56%
32%
0%
10%
20%
30%
40%
50%
60%
70%
Officers (n=147) Board Of Directors
(n=300)
Compensation
Committee
(n=268)
Other (n=154)
Percentage of Hospitals
Many of the organizations selecting “other” provided supplemental explanations
which included one or more of the listed categories (for example, identifying
specific officers that determined compensation). Also, some distinguished the
Executive Committee of the Board as determining compensation, rather than the
entire Board or a specific Compensation Committee. Some hospitals reported
that the Human Resources Division determined compensation in a number of
instances. Others reported that compensation was determined by the parent or
another affiliated organization.
Compared to other community types, critical access hospitals reported the Board
of Directors as setting compensation more often than the other groups (82%
compared with 63% overall), while less than half of the hospitals located in the
high population areas (48%) reported such. Of the community types, critical
access hospitals reported the lowest incidence of the Compensation Committee
setting compensation, while the urban and suburban hospitals (both those
located in the high population areas and elsewhere) reported the highest. As the
revenues increased for the hospitals, the percentage of hospitals that identified
the Board of Directors as setting compensation generally decreased, while the
percentage that identified the Compensation Committee significantly increased.
Figure 103 and Figure 104, below, show the distribution of the individual or entity
responsible for determining compensation, by community type and then by
revenue size.
130

Figure 103. Distribution of Individual or Entity Reported to Determine Compensation by
Community Type
34%
32%
30%
31%
48%
82%
68%
61%
63%
68%
25%
47%
63%
56%
36%
38%
31%
32%
28%
25%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Percentage of Hospitals
Officers Board of Directors Compensation Committee Other
131

Figure 104. Distribution of Individual or Entity Reported to Determine Compensation
by Revenue Size
34%
35%
24%
36%
22%
31%
80%
67%
53%
59%
47%
63%
22%
51%
66%
74%
92%
56%
27%
34%
36%
31%
25%
32%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
Percentage of Hospitals
Officers Board of Directors Compensation Committee Other
Resources and methods used to establish compensation (Question 5)
Question 5 asked what resources and methods the hospital used to determine
compensation amounts, identifying seven choices. 478 hospitals responded to
this question. The chart below shows the percentage of respondents that
indicated using each of the seven listed resources, with 87% of the respondents
identifying the use of published surveys to determine compensation amounts and
9% identifying written offers. Published surveys was the most frequently
reported tool, and written offers was the least frequently reported tool, across
each community type and revenue size category.
132

Figure 105. Tools Used to Determine Compensation
(n=478)
87%
28%
21%
36%
48%
9%
19%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Pub
lished
S
uv
e
y
s
(n=41
9)
Internet Re
s
e
a
rc
h
(n
=1
32)
P
ho
ne Sur
v
ey
(
n=102)
O
ut
s
id
e
E
x
p
ert
(Related) (n=17
1)
O
u
tside
Exper
t
(U
n
related)
(n=2
2
9)
Writ
ten Of
f
e
rs
(n=41
)
O
ther
(
n=91)
Percentage of Hospitals
91 hospitals (19%) selected “other” and provided an additional explanation. In a
number of instances, the hospital’s additional explanation was to identify the
particular survey or expert relied upon. For example, some hospitals relied upon
Form 990 data.
The rural hospitals (both CAH and non-CAH) reported the highest percentages of
hospitals using phone surveys to determine compensation amounts and the
lowest percentages of use of an outside expert. Hospitals located in the high
population areas reported the highest use of an outside expert report prepared
by an expert employed by the hospital (referred to in the figures as “related”).
The reported use of internet research and phone surveys generally declined as
hospitals increased in revenue size, while the reported use of outside experts
generally increased with revenue size.
133

Figure 106. Distribution of Reported Use of Tools to Determine Compensation Amounts
by Community Type
94%
85%
87% 87%
29%
18% 18%
21%
52%
18%
29%
36% 36%
31%
52%
48%
16%
4%
11%
6%
9%
18%
20%
86%
25%
33%
28%
27%
28%
29%
40%
55%
19%
13%
21%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Percentage of Hospitals
Published Survey Internet Research Phone Survey
Outside Expert - Related Outside Expert - Unrelated Written Offers
Other
134

Figure 107. Distribution of Reported Use of Tools to Determine Compensation Amounts
by Revenue Size
96%
89%
80%
87%
86%
87%
42%
44%
69%
36%
28%
47%
51%
69%
48%
7%
18%
16%
24%
15%
22%
19%
32%
21%
14%
28%
23%
40%
32%
27%
14%
15%
21%
11%
33%
9%
50%
10%
7%
9%
11%
9%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Total
Percentage of Hospitals
Published Survey Internet Research Phone Survey
Outside Expert - Related Outside Expert - Unrelated Written Offers
Other
Factors included in comparability data used by the organization
ed hospitals to show which of six identified factors were included
(Question 6)
Question 6 ask
in the comparability data used by the hospital. Respondents were also asked
whether each factor was used for all employees described in section
4958(f)(1).
66
For each of the six identified factors, at least 90% of the
respondents indicated they considered that factor, with 71% indicating that they
considered all of the factors. The responses are summarized below.
66
Section 4958(f)(1) defines disqualified persons subject to the excess benefit transaction tax.
135

Figure 108. Factors Included in Comparability Data
91%
99%
93%
97%
90%
4%
0%
20%
40%
60%
80%
100%
120%
Education
and
E
x
pe
ri
ence
(
n=436
)
Specific
Responsibil
it
ie
s
(n=475
)
Geographic Area (n=447)
Similar Ser
v
ices (
n
=463)
B
eds,
Ad
m
issions,
or
O
ut
pa
t
ien
t
Visit
s
(n=43
2)
O
ther Factors (n=21)
Percentage of Hospitals
Hospitals that selected a given factor typically reported that they used that factor
in their comparability analysis for all section 4958(f)(1) employees. Where
hospitals indicated that other factors were considered that were not separately
listed in the question, the most common explanation was that the hospital also
considered entities with similar levels of revenue in determining comparability.
The most common explanation offered by hospitals for not considering factors
was that the use of the factor depended upon whether the hospital was recruiting
new hires or setting compensation for incumbents. For example, responses
indicated that when recruiting new hires and using a national recruitment
program, comparability might not be limited to entities in similar geographic
areas, but when determining annual compensation for incumbents, education
and experience might not be considered.
Among the community types, the rural non-critical access hospitals reported the
lowest percentage of hospitals taking into account all of the identified factors,
while those in the high population areas reported the highest, although the
differences were modest. There was a slightly greater variation across revenue
size, with the hospitals with revenue between $100 million and $250 million
reporting the highest percentage considering all factors and the hospitals with
revenue exceeding $500 million reporting the lowest.
136

Figure 109. Percentage of Hospitals that Considered all Comparability Factors
by Community Type
73%
70%
66%
72%
71%
60%
65%
70%
75%
80%
High Population CAH Rural - Non CAH Others Total
Percentage of Hospitals
Figure 110. Percentage of Hospitals that Considered all Comparability Factors
by Revenue Size
68% 68%
77%
75%
64%
71%
60%
65%
70%
75%
80%
Under $25M $25M - Under
$100M
$100M - Under
$250M
$250M - Under
$500M
$500M and Over Total
Percentage of Hospitals
137

As Figure 111 and Figure 112 demonstrate, there was little variation in the
consideration of specified factors across community types or revenue size
groups.
Figure 111. Percentage of Hospitals that Considered Comparability Factors
by Community Type
Community Type
Edu & Exp Responsibility Same Area
Similar
Srvc
Similar Bed
#
High Population 92% 100% 95% 97% 90%
CAH 93% 98%* >95% 94% 91%
Rural - Non CAH 91% 98%* 94% 95% 91%
Others 91% <100% 91% 98% 90%
Total (N = 479)
91%
99%
*All rural
hospitals
93%
97%
90%
*Both groups of rural hospitals (CAH and non-CAH) were combined to prevent potential identification of
respondent hospitals.
Figure 112. Percentage of Hospitals that Considered Comparability Factors
by Revenue Size
Revenue Size
Edu & Exp Responsibility Same Area
Similar
Srvc
Similar Bed
#
Under $25M 95% 98%* 95% 93% 88%
$25M - Under $100M 91% 98%* 97% 96% 91%
$100M - Under $250M 91% 100% 95% 98%* 92%
$250M - Under $500M 90% 100% 82% 98%* 88%
$500M and Over 89% 100% 83% 100% 89%
Total (N = 479)
91%
99%
*Under
$100M
93%
97%
*$100M -
<$500M
90%
*Revenue sizes were combined to prevent potential identification of respondent hospitals.
Use of other tax-exempt hospitals as comparability data (Question 7)
Question 7 asked whether the hospital’s comparability data included information
from other tax-exempt hospitals. 100% of 478 respondents indicated that their
comparability data included information from other tax-exempt hospitals. The
questionnaire did not ask about comparability data from for-profit hospitals.
Setting compensation within the range of comparability data (Question 8)
Question 8 asked whether the hospital set compensation within the range of
comparability data. Nearly all of 478 respondents reported that compensation
was set within the range of the comparability data.
Business relationships with officers, directors, trustees, and key
employees (Question 9)
Question 9 asked whether the hospital had a business relationship with any of its
officers, directors, trustees or key employees, other than through their position as
officers, directors, trustees, or key employees, and to describe any such
relationships. 303 (65%) of 468 reported having at least one such business
relationship. Figure 113 and Figure 114 display the results by community type
and revenue size. The two most commonly reported types of business
relationships were the furnishing of goods, services or facilities by the officer,
138

director, trustee or key employee to the hospital and doing business with an
entity in which the officer, director, trustee or key employee is a partner or
investor.
Compared with rural hospitals (CAH and non-CAH), a higher percentage of
urban and suburban hospitals (high population and other urban and suburban
hospitals) reported having a business relationship with its officers, directors,
trustees or key employees. The percentage of hospitals indicated having a
business relationship with its officers, directors, trustees or key employees
generally increased as revenue size increased, with less than half of the
responding hospitals with less than $25 million in revenue indicating that they
had such a relationship and over 80% of the hospitals with revenues exceeding
$250 million doing so.
Figure 113. Percentage of Hospitals Reporting a Business Relationship with its Officers,
Directors, Trustees, or Key Employees by Community Type
66%
49%
59%
70%
65%
0%
10%
20%
30%
40%
50%
60%
70%
80%
High
Population
Critical
Access
Rural - Non-
CAH
Other Total
Percentage of Hospitals
139

Figure 114. Percentage of Hospitals Reporting a Business Relationship with its Officers,
Directors, Trustees, or Key Employees by Revenue Size
48%
58%
71%
86%
82%
65%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Under
$25M
$25M
under
$100M
$100M
under
$250M
$250M
under
$500M
Over
$500M
Totals
Percentage of Hospitals
C. Summary of Examinations
1. Overview of Examination Component of the Project
The examination component of the Hospital Compliance Project is part of
Exempt Organization’s ongoing review of executive compensation in the
tax-exempt sector.
67
In this study, the focus of the examinations was three-fold:
(1) to follow up on the questionnaire responses regarding how organizations
determined compensation, (2) to determine whether organizations were utilizing
the rebuttable presumption, and (3) to determine whether the compensation so
determined should be subject to tax as an excess benefit transaction under
section 4958. Twenty hospitals from the study were selected for the examination
component of the project.
To select the twenty hospitals to be included, IRS revenue agents and specialists
reviewed the Forms 990, questionnaire responses, and other compensation
information to identify the hospitals within the study that paid greater
67
In 2007, EO issued its report on the Executive Compensation Compliance Initiative. Included
in its recommendations were that future initiatives should focus on the correlation between
satisfaction of the rebuttable presumption by an organization and the reasonableness of
compensation paid to its disqualified persons by such an organization. Accordingly, this initiative
included an executive compensation component focusing on these issues.
140

compensation amounts relative to the size and type of the organization. Their
review focused on the highest paid and/or top management official, although in
some cases they included up to four additional highly paid officials per
organization in their review.
The process used to examine executive compensation of these twenty
organizations was that regularly used to examine compensation paid by taxable
and tax-exempt organizations to their officers, directors, trustees, key employees,
and other high level officials. Accordingly, the examining agents used traditional
risk analysis to assess whether they would request additional information from
the organizations, conduct sampling of expense accounts and other
compensation-related items, and seek the involvement of specialists to assist in
conducting these examinations.
2. Examination Results
a. Overview
The twenty hospitals examined as part of this project constitute a small pool.
Therefore, to prevent potential identification of examined hospitals, in many
instances the findings below are discussed in generalities. Furthermore, the
findings are not based on statistical sampling and cannot be applied to the
general population. They merely reflect the organizations selected and are not
representative of any portion of the hospital sector.
While the hospitals examined were selected based upon identifying highly paid
individuals, consideration was given to the size and nature of the hospital. The
twenty hospitals represent a reasonable cross section of the study’s overall
hospital group in terms of community type and revenue size. The hospitals are
classified by community types and revenue size groups as follows:
68
Community types:
• High population – 6 hospitals (30%)
• Rural (CAH and non-CAH) – 4 hospitals (20%)
• Other urban and suburban – 10 hospitals (50%)
Revenue sizes:
• Under $250 million – 8 hospitals (40%)
• $250 million - $500 million – 9 hospitals (45%)
• Over $500 million – 3 hospitals (15%).
In some instances, information concerning compensation was in the possession
of another organization (e.g., a parent of the organization) so the organization
68
Certain categories were combined to prevent potential identification of the examined hospitals.
141

that possessed such information was the entity examined, rather than the original
respondent to the questionnaire.
b. Compensation amounts reported
As discussed above, the hospitals were selected for examination because they
were identified as paying identified individuals greater compensation amounts,
relative to the size and nature of the hospital. The examinations also reviewed
compensation paid by other entities.
The total compensation paid by the twenty hospitals examined (including by
related entities or common paymasters) to the individuals identified during the
examination selection process is included in the table below. The twenty
hospitals reported paying a total of $45.2 million, or 88% of the total of $51.3
million compensation paid to these individuals. The other 12% was paid by
related entities, supporting organizations, or common paymasters. In those
instances where compensation is paid by other entities, the average and median
amount paid is 47% of the average and median amount paid by the hospitals
examined.
69
Figure 115. Total Compensation Paid to Identified Highly Compensated Individuals of
Examined Hospitals
Description
Paid by
Hospitals
Examined
Paid by
Other
Entities
Total Paid by
Examined
Hospitals and
Other Entities
Salaries $30,704,177 $4,963,715 $35,667,892
Deferred Compensation $6,333,625 $285,886 $6,619,511
Other Compensation $8,190,340 $832,360 $9,022,700
Total Compensation $45,228,142 $6,081,961 $51,310,103
Statistics of Total Compensation
- Average $753,802 $357,762 $801,720
- Median $522,203 $246,402 $578,808
Total compensation paid to the CEO/President, the CFO/VP Finance, and all
other identified highly compensated individuals is included in the following chart.
These amounts include payments made by other entities. Primarily due to
identifying relatively high paid individuals through the examination selection
process, the average and median compensation paid to the CEO/President in the
examined hospitals is substantially higher than the average and median salary
reported for the top management officials on the questionnaires.
69
The average and median compensation amounts paid by other entities are based on
compensation paid to individuals reported to have received compensation from another entity.
The calculation did not take into account cases in which no compensation was paid by another
entity (thus, resulting in higher average and median amounts than if such cases had been taken
into account).
142

Figure 116. Total Compensation to Identified Highly Compensated Individuals of
Examined Hospitals by Position Title
CEO/President
CFO/VP
Finance
All Other
Identified
Individuals
Total
Salaries $17,088,894 $12,070,679 $6,508,319 $35,667,892
Deferred Compensation $5,022,047 $1,285,109 $312,355 $6,619,511
Other Compensation $6,895,815 $1,494,154 $632,731 $9,022,700
Total Compensation $29,006,756 $14,849,942 $7,453,405 $51,310,103
Statistics of Total Compensation
- Average $1,381,274 $571,152 $438,436 $801,720
- Median $1,270,671 $549,347 $264,037 $578,808
c. How compensation was determined
The twenty examinations followed up on the questionnaire and looked at how
compensation was determined, including review of the supporting
documentation. The examinations confirmed that all twenty hospitals had a
written conflict of interest policy that they adhered to.
85% of the hospitals examined had a written compensation policy, as compared
to 73% of the hospitals that responded to the questionnaire. While in most cases
if the hospital had a written compensation policy it followed that policy in all
circumstances covered by its terms, there were a few instances where the
hospital did not.
In all cases, compensation was approved in advance, nearly always by
individuals that did not have a conflict of interest with the compensation
arrangement being approved. This is comparable to the 98% of hospitals
responding to the questionnaire that indicated that compensation was approved
in advance by individuals that did not have a conflict of interest with the
compensation arrangement being approved.
In 85% of the hospitals examined, hospitals had employment contracts with
disqualified persons and in nearly all such cases the contract amount was found
to be reasonable.
The amount of compensation was determined by the Compensation Committee
at nearly all of the examined hospitals, with slightly over half of the examined
hospitals also having compensation determined by the Board of Directors. This
contrasts with the 56% of responding hospitals that indicated that the
compensation was determined by the Compensation Committee on the
questionnaire and compares similarly to the 63% of the questionnaire
respondents that indicated the Board of Directors determined compensation.
Few of the hospitals examined had compensation amounts determined by
143

officers. As was indicated in questionnaire responses, there were instances
where the compensation was determined by an affiliated entity or by an
Executive Committee.
70% of the examined hospitals used published surveys to establish
compensation amounts (compared to 87% of the questionnaire respondents).
45% of the examined hospitals used an outside expert report prepared by an
expert employed by an unrelated organization compared to 48% of the hospitals
responding to the questionnaire. 65% of the examined hospitals used an outside
expert report prepared specifically for the hospital by an expert employed by the
hospital for that purpose (compared to 36% of the responding hospitals). None
of the examined hospitals used phone surveys to determine compensation
amounts (compared to 21% of the responding hospitals).
Figure 117. Examination Results - Tools Used to Determine Compensation
70%
15%
0%
65%
45%
15%
0%
10%
20%
30%
40%
50%
60%
70%
80%
Published Surveys Internet Phone Survey Outside Expert -
Related
Outside Expert -
Unrelated
Written offers
Percentage of hospitals
45% of the examined hospitals considered all of the identified factors included in
comparability data, compared to 71% of the hospitals responding to the
questionnaire. All of the examined hospitals used the specific responsibilities of
the position, while only 60% used similar number of beds, admissions or
out-patient visits in their comparability data. Although not all of the examined
hospitals considered each of the remaining three identified factors, at least
three-quarters of the examined hospitals considered each of them. As with the
questionnaire responses, the most common factor considered other than the
listed factors was similar levels of revenue. The factors were used consistently
for all disqualified persons in 80% of the examined hospitals.
144

In all cases the examined organizations obtained comparability data involving
tax-exempt hospitals, although not every examined hospital obtained
comparability data regarding tax-exempt hospitals for all components of the
compensation that was paid.
Nearly all of the examined hospitals set their actual compensation within the
range of the comparability data.
Although 65% of the hospitals responding to the questionnaire indicated having a
business relationship with any of its officers, directors, trustees or key
employees, other than through their position as officers, directors, trustees, or
key employees, a business relationship existed in only 40% of the hospitals
examined. Most of these cases involved the furnishing of goods, services or
facilities, although there were also instances involving loans and the sale or lease
of property. In all cases where the business relationship was reviewed, no
excess benefit transaction was found.
d. Rebuttable presumption analysis
After reviewing the process used by the hospital to establish compensation, the
IRS then determined whether that process met the rebuttable presumption
procedure described in Treasury Regulation section 53.4958-6.
70
This process
involves three factors – an independent body to review and establish the amount
of compensation in advance of actual payment, use of permissible comparability
data to establish the compensation, and contemporaneous documentation of the
process used to establish the compensation in the particular instance. Under the
Regulations, compensation determined pursuant to a process that satisfies the
rebuttable presumption requirements is presumed to be reasonable in amount,
and the IRS has the burden of proving that the compensation is excessive for
section 4958 excess benefit transaction tax purposes. If the rebuttable
presumption is not met, the burden is on the organization to prove that the
compensation is reasonable.
Organizations met the requirements of the rebuttable presumption process in
85% of the examined hospitals.
e. Information reporting and potential assessment of section 4958
excise tax
The compensation paid to the identified highly paid individuals was reviewed to
determine whether the section 4958 excise tax should be assessed. In the case
of the 85% of hospitals that met the rebuttable presumption, the burden of proof
was on the IRS to show that compensation was not reasonable. This review
included analysis of compensation data and surveys available to the IRS in
addition to the comparables used by the organizations in setting compensation.
70
See H. Rep. No. 104-506, 104
th
Cong., 2d Sess. at 56-57.
145
The IRS determined that no excess benefit tax should be assessed in these
instances. The IRS may assess 4958 excess tax in certain other case(s), but to
prevent potential identification of examined hospitals, specific details cannot be
provided.
The IRS also reviewed whether compensation paid to the identified highly
compensated individuals was properly reported on various federal forms. Nearly
all of the examined hospitals properly reported compensation on Form 990. For
Forms 941 and W-2, all compensation was properly reported. The Forms 1040
for the identified highly compensated individuals were also reviewed where
appropriate. In all cases where the Form 1040 was reviewed, compensation was
reported correctly.
146
VIII. FORM 990, SCHEDULE H, HOSPITALS
A. Overview of Schedule H, Hospitals
Form 990, Schedule H, Hospitals, will be used beginning with 2008 tax years to
report information by an organization that operates one or more facilities that are
licensed, registered, or similarly recognized by a state as a hospital. For years
before 2008, the Form 990 did not provide for the reporting of community benefit
activities or request important information regarding how nonprofit hospitals
serve the public consistent with the tax exemption. Beginning with 2008 tax
years, organizations operating one or more hospitals are required to report
community benefit and other information pertinent to exempt status on Schedule
H.
Schedule H includes six parts: Part I, Charity Care and Certain Other Community
Benefits at Cost; Part II, Community Building Activities; Part III, Bad Debt,
Medicare, & Collection Practices; Part IV, Management Companies and Joint
Ventures; Part V, Facility Information; and Part VI, Supplemental Information. A
copy of Schedule H is appended hereto as Appendix C.
An organization must file a single Schedule H that aggregates information for the
tax year from the following:
1. Hospitals directly operated by the organization.
2. Hospitals operated by disregarded entities of which the organization is the
sole member.
3. Other facilities or programs of the organization or any of the entities
described in 1 or 2, even if provided by a facility that is not a hospital or if
provided separately from the hospital’s license.
4. Hospitals operated by any joint venture taxed as a partnership, to the
extent of the organization’s proportionate share of the joint venture.
Although information from all of the above sources is aggregated for purposes of
Schedule H, the organization is required to list in Part V, Facility Information,
each of its facilities that is required to be licensed, registered, or similarly
recognized as a health care facility under state law, whether operated directly by
the organization or indirectly through a disregarded entity or joint venture taxed
as a partnership. In addition, the organization must report in Part VI summary
information describing the number of other types of facilities for which it reports
information on Schedule H (e.g., 2 rehabilitation clinics, 4 diagnostic centers).
B. Description of Schedule H, Parts I through VI
The following summarizes certain important information required to be reported
on Schedule H:
147
• Part I, Charity Care and Certain Other Community Benefits at Cost
(Optional for 2008)
o Requires reporting of charity care policies, the availability of
community benefit reports, and the cost of charity care and other
community benefit programs
o Eight separate categories of community benefit are reportable in
Part I: charity care at cost, unreimbursed Medicaid, unreimbursed
other means-tested government programs, community health
improvement services and community benefit operations, health
professions education and training, subsidized health services,
research, and cash and in kind contributions to community groups
• Part II, Community Building Activities (Optional for 2008)
o Provides for reporting the cost of various kinds of community
building activities, including physical improvements and housing,
economic development, community support, environmental
improvements, community health improvement advocacy, coalition
building, workforce development, and leadership development and
training for community members
• Part III, Bad Debt, Medicare, & Collection Practices (Optional for 2008)
o Requires reporting of bad debt expense and Medicare shortfalls at
cost, and other information relating to such items
o Medicare shortfall reporting in Part III is limited to expenses
reportable on Medicare cost reports, although other revenue and
expense information for other Medicare programs is to be reported
in Part VI
o Also requests certain information regarding the organization’s debt
collection practices
• Part IV, Management Companies and Joint Ventures (Optional for 2008)
o Requires information regarding certain joint ventures and
management companies in which the organization’s officers,
directors, trustees, key employees, and physicians have an
aggregate ownership percentage exceeding 10% of such entity
• Part V, Facility Information
o The organization must separately list each facility that is licensed,
registered, or similarly recognized by a state as a health care
facility (hospital or otherwise) (Required for 2008)
o The organization must provide a narrative description of other
facilities for which items are otherwise reported on the Schedule H
(Optional for 2008)
• Part VI, Supplemental Information (Optional for 2008)
o Requires information pertinent to determining how the organization
is serving its communities, including community needs
assessments, education of patients about eligibility for charity care
and government assistance programs, relationships with others in
an affiliated system, and descriptions that supplement responses to
the other parts of the schedule
148
C. Transition Relief
Schedule H is phased in beginning in 2008. For 2008 tax years, only Part V,
Facility Information, is required to be completed so that basic identifying
information regarding the organization’s facilities is collected. All other parts of
Schedule H are optional for 2008. The entire Schedule H must be completed for
tax years beginning in 2009.
D. Promoting Uniform Reporting through Schedule H
As the study demonstrates, the reporting of community benefit by organizations
operating nonprofit hospitals has varied widely, both as to types of programs and
expenditures classified as community benefit and the measurement of
community benefits. Schedule H was designed to provide uniformity regarding
the types and amounts of programs and expenditures reported as community
benefit by nonprofit hospitals. It does so by providing clear standards regarding
the types of programs and expenditures the filing organization is to report as
community benefit in Part I, how to measure community benefit expenditures (by
cost rather than by charges), and the treatment of two of the most significant
areas of disparity reported in the study (bad debt and Medicare shortfalls).
Hospitals filing Schedule H are required to use the most accurate costing method
available to them to report the cost of community benefit on Schedule H.
Schedule H also provides organizations the opportunity to explain what amounts
of bad debt expense, Medicare shortfalls, and community building activities it
believes should be treated as community benefit even though the schedule does
not permit it to treat them as community benefit at this time. Because not all
aspects of community benefit are capable of quantitative measure, Part VI of the
schedule requires the organization to provide certain information regarding non-
quantifiable aspects of community benefit, and allows the organization to
supplement the required information with other information it considers relevant
to explaining how it benefits the communities it serves through the promotion of
health.
Much of the information requested in the Hospital Study Questionnaire is
included in Schedule H. The following describes which portions of Part II –
Operations, of the Questionnaire are included in the Schedule H.
• Question 1 (type of hospital) – incorporated in Part V, the list of
facilities, where the organization is to report the type of each facility
that is licensed, registered, or similarly recognized as a health care
facility by a state.
• Questions 2 through 8 (patients) – although similar information was
included in the Schedule H discussion draft released in June 2007
(e.g., revenue information for each type of insurance or government
149
program, including self pay patients), the final Schedule H does not
require this information.
• Questions 9 through 14 (emergency room) – portions incorporated in
Part V by indicating whether the facility has an emergency room that
is open at all times or at specified times.
• Questions 15 through 18 (board of directors) – portions incorporated
in Part VI, question 6 regarding a description of how the community
board furthers the organization’s exempt purposes; also, Part VI of the
Form 990’s core form contains a governance section required to be
completed by all organizations, including those operating hospitals.
• Questions 19 and 20 (medical staff privileges) - portions incorporated
in Part VI, question 6 regarding a description of how the organization’s
open medical staff furthers the organization’s exempt purposes.
• Questions 21 through 29 (medical research) – cost of medical
research that constitutes community benefit is to be reported in Part I,
line 7i.
• Questions 30 through 33 (professional medical education and
training) – cost of health professions education that constitutes
community benefit is to be reported in Part I, line 7f.
• Questions 34 through 42 (uncompensated care)
o Questions regarding charity care policies, and the cost of
charity care, Medicaid, and other means-tested government
programs, were incorporated in Part I of the schedule.
o Questions regarding bad debt and Medicare shortfalls were
incorporated in Part III of the schedule, which requires
reporting at cost.
• Questions 43 through 56 (billing and collection practices) – questions
regarding collection practices were incorporated in Part III of the
schedule.
• Questions 57 through 72 (community programs)
o Questions regarding medical screening programs,
immunization programs, educational programs for the
community, and newsletters or publications are contained in
Part I, line 7e regarding treatment of such items as community
health improvement services and community benefit
operations.
o Questions regarding unmet health care needs of the
community and improving access to health care are
incorporated in Part VI, question 2 (describe how the
organization assesses the health care needs of the
communities it serves), question 3 (describe how the
organization informs and educates persons about eligibility for
assistance under public programs or charity care), question 4
(describe the communities served by the organization,
including geographic and demographic constituents), and
question 6 (provide other information regarding how the
150
organization furthers its exempt purposes), as well as Part I,
line 7e (establishing community need for programs reported as
community health improvement services and community
benefit operations, and improving access to health services).
151
IX. SUMMARY OF FINDINGS BY DEMOGRAPHIC
This section provides a summary of the findings of the study overall and by
community type, revenue size and other selected areas. These findings relate to
patient mix, total revenues and excess revenues, various community benefit
expenditures (including uncompensated care, research, education and training,
and community programs), and executive compensation.
Demographics and Community Benefit Profile for All Hospitals in the Study
• Patient mix – private insurance (43%), Medicare (31%), Medicaid (15%),
uninsured (8%), and other public programs (3%)
• Annual total revenues - $179 million (average) and $89 million (median)
o Distribution - 53% with revenues under $100 million (17% under $25
million); 27% with revenues between $100 million and $250 million;
20% with revenues over $250 million (7% over $500 million)
• Excess revenues were 4.6% of total revenues, but increased with total
revenue size
o 3.3% (under $25 million) to 5.5% (over $500 million)
o Average and median excess revenue amounts were $8.3 million and
$2.5 million, respectively
o 60% of hospitals reported excess revenues less than 5% of total
revenues
21% reported a deficit (total expenses greater than revenues)
19% reported positive excess revenues less than 2.5% of
revenues; 39% reported positive excess revenues less than 5%
of total revenues
o Excess revenues were concentrated in a small number of the most
profitable hospitals – 16% of the hospitals (those reporting at least $15
million in excess revenues) reported 77% of the excess revenues
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 9.2% and 5.5%, respectively
o Mix across types of community benefit expenditure – 56% of reported
expenditures were uncompensated care, followed by medical
education and training (23%), medical research (15%), and community
programs (6%)
The mix changes as follows when the 15 hospitals reporting
93% all of the reported research expenditures is removed from
the group: 71% of reported community benefit expenditures
were uncompensated care, followed by medical education and
training (21%), community programs (7%), and medical
research (1%)
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 10% and 3%, respectively (compared to 8% of uninsured
patients).
152
o Average and median percentage of total revenues reported as spent
on uncompensated care were 7.2% and 3.9%, respectively
o 95% of hospitals reported uncompensated care; 44% reported treating
bad debt and 51% reported treating uninsured shortfalls as
uncompensated care; lesser percentages reported shortfalls from
private insurance (19%), Medicare (20%), Medicaid (20%), other public
programs (18%) as uncompensated care
• Research, education, and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (1.3% and 0.3%); medical
research (1.6% and 0.2%); community programs (0.9% and 0.2%)
o 77% of hospitals reported medical education and training, 21%
reported medical research, and 92% reported community program
expenditures
• Comparison of community benefit expenditure and uncompensated care
levels to specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (21%);
under 5% of total revenues (47%)
o Uncompensated care under or equal to 1% of total revenues (19%);
under or equal to 3% of total revenues (43%); under or equal to 5% of
total revenues (58%)
By Community Type
The community benefit expenditure profile (i.e., the mix of uncompensated care,
medical research, medical education and training, and community program
expenditures) of the hospitals in the study varied materially depending upon the
community type (CAH, rural (non-CAH), other urban and suburban, and high
population). This variation tended to be greatest when comparing CAH hospitals
to high population hospitals. CAHs often resembled rural (non-CAH) hospitals,
but there were important differences between the two types in some areas. In
general, the profile of the group of other urban and suburban hospitals generally
reflected that of the overall group, in large part because of its sample size. Rural
hospitals as a group (CAH and non-CAH) reported lower average and median
percentages of aggregate community benefit expenditures than did urban and
suburban hospitals (high population and other urban and suburban hospitals).
High Population Hospitals
High population hospitals were the largest of the hospitals in terms of average
and median annual total revenues. They had a higher proportion of Medicaid
patients, and a lower proportion of Medicare patients, than the other hospitals.
High population hospitals reported the highest average and median percentages
of aggregate community benefit expenditures, uncompensated care, medical
education and training, and medical research, as a percentage of total revenues.
They also had the highest percentage of hospitals reporting medical research
and medical education and training expenditures. These hospitals are located in
153
the largest 26 urban areas in the U.S.; they comprised 19% of the hospitals in the
study.
• Patient mix – private insurance (44%), Medicare (28%), Medicaid (19%),
uninsured (8%), and other public programs (4%)
• Annual total revenues – the average and median total revenues were $389
million and $196 million, respectively; they comprised 41% of aggregate total
revenues overall – on average, these hospitals had over twice the revenues
of those overall
• Excess revenues – excess revenues as a percentage of total revenues was
4.5% (compared to 4.6% overall)
o The average and median excess revenue amounts were $17.5 million and
$4.2 million, respectively (greater than any other community type)
o 22% of these hospitals reported a deficit, and 69% reported a deficit or
positive excess revenues less than 5% of total revenues
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 12.7% and 9.8%, respectively (both the
largest of all community types)
o Mix across types of community benefit expenditure– 42% of reported
community benefit expenditures were uncompensated care, followed by
medical education and training (26%), medical research (25%), and
community programs (7%)
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 11% and 6%, respectively (highest of all community types)
o Average and median percentage of total revenues reported as spent on
uncompensated care were 7.9% and 4.8%, respectively (highest of any
community type)
o 96% of these hospitals reported providing uncompensated care; a lesser
percentage reported treating all types of shortfalls as uncompensated
care, but a greater percentage reported treating bad debt as
uncompensated care, compared to overall
• Research, education and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (2.7% and 1.6% - highest of
all community types); medical research (3.2% and 0.4% - highest of all
community types); community programs (1.7% and 0.2%)
o 86% of hospitals reported medical education and training, and 40%
reported medical research expenditures (both were the highest of all
community types); 95% reported community program expenditures of
some type
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (11%); under
5% of total revenues (32%)
154
o Uncompensated care under or equal to 1% of total revenues (8%); under
or equal to 3% of total revenues (33%); under or equal to 5% of total
revenues (52%)
Critical Access Hospitals (CAHs)
CAHs were the smallest of the hospitals in terms of average and median annual
total revenues across community types. They had a higher proportion of
Medicare patients than did the other hospitals, but lower proportions of private
insurance and Medicaid patients than the others. CAHs reported the lowest
average and median percentages of aggregate community benefit expenditures,
uncompensated care, medical education and training, and medical research, as
a percentage of total revenues. They also had the lowest percentage of
hospitals reporting medical research and medical education and training
expenditures.
• CAH refers to those hospitals designated as such under federal law; they
comprised 14% of hospitals in the study
• Patient mix – private insurance (38%), Medicare (36%), Medicaid (13%),
uninsured (8%), and other public programs (3%)
• Annual total revenues – the average and median total revenues for CAHs
were $29 million and $20 million, respectively; CAHs comprised 2% of
aggregate total revenues overall (smallest of community types based on
revenues)
• Excess revenues – excess revenues as a percentage of total revenues was
3.5% (lowest of the community types)
o the average and median excess revenue amounts for CAHs were $1.0
million and $0.5 million, respectively (also lowest of the community types)
o 34% of all CAHs reported a deficit, and 66% reported a deficit or positive
excess revenues less than 5% of total revenues
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 6.3% and 2.8%, respectively
o Mix across types of community benefit expenditures – 77% of reported
community benefit expenditures were uncompensated care, followed by
community programs (19%), medical education and training (4%), and
medical research (0%)
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 7% and 2%, respectively (lowest of the community types)
o Average and median percentage of total revenues reported as spent on
uncompensated care were 5.6% and 2.1%, respectively (lowest of the
community types)
o 94% of CAHs reported providing uncompensated care; a greater
percentage of CAHs reported treating most types of shortfalls as
uncompensated care, but a lesser percentage reported treating bad debt
as uncompensated care, compared to overall
• Research, education and community programs
155
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (0.2% and 0.1%); medical
research (0% and 0%) (both lowest of all community types); community
programs (1% and 0.3%)
o 60% of CAHs reported medical education and training; 91% reported
community program expenditures of some type
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (39%); under
5% of total revenues (61%)
o Uncompensated care under or equal to 1% of total revenues (31%); under
or equal to 3% of total revenues (59%); under or equal to 5% of total
revenues (67%)
Rural (non-CAH) Hospitals
This group was the second smallest community type in terms of average and
median annual total revenues, after CAHs. Rural (non-CAH) hospitals had a
relatively low percentage of Medicaid patients compared to the other community
types, and reported the lowest percentage of uninsured patients of all the
community types. The community benefit expenditure and uncompensated care
profile for this group resembled that of CAHs, in that they generally reported
relatively low average and median aggregate community benefit expenditures,
uncompensated care, medical education and training, and medical research, as
a percentage of total revenues, when compared to the other hospitals (except for
CAHs). However, rural (non-CAH) hospitals reported higher percentages of
medical education and training expenditures, and lower percentages of
community program expenditures, as a percentage of total revenues, than did
CAHs.
• Includes those hospitals outside the urban and suburban areas that were not
designated as CAHs; they comprised 16% of hospitals in the study
• Patient mix – private insurance (44%), Medicare (33%), Medicaid (13%),
uninsured (7%), and other public programs (3%)
• Annual total revenues – the average and median total revenues were $93
million and $68 million, respectively; these hospitals comprised 8% of
aggregate total revenues overall – on average, these rural hospitals had
greater revenues than CAHs
• Excess revenues – excess revenues as a percentage of total revenues was
6.0% (highest of any community type)
o the average and median excess revenue amounts were $5.6 million and
$3.4 million, respectively (greater than CAHs)
o 13% reported a deficit and 42% reported a deficit or positive excess
revenues less than 5% of total revenues (both were lowest percentages of
any community type)
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 8.4% and 3.2%, respectively
156
o Mix across types of community benefit expenditures – 76% of reported
community benefit expenditures were uncompensated care, followed by
medical education and training (17%), community programs (6%), and
medical research (1%)
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 8% and 2%, respectively
o Average and median percentage of total revenues reported as spent on
uncompensated care were 7.6% and 2.7%, respectively
o 96% of these hospitals reported providing uncompensated care; a greater
percentage reported treating all types of shortfalls as uncompensated
care, but a lesser percentage reported treating bad debt as
uncompensated care, compared to overall
• Research, education and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (0.6% and 0.2%); medical
research (0.5% and 0.3%); community programs (0.6% and 0.2%)
o 72% of hospitals reported medical education and training; 96% reported
community program expenditures of some type
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (31%); under
5% of total revenues (57%)
o Uncompensated care under or equal to 1% of total revenues (25%); under
or equal to 3% of total revenues (52%); under or equal to 5% of total
revenues (65%)
Other Urban and Suburban Hospitals
This group was the second largest community type in terms of average and
median annual total revenues, after high population hospitals, and its average
and median total revenue measures closely resembled those of the overall
responding group. Its patient mix was nearly identical to that of the overall
responding group. This community type generally was around the middle (rather
than on the high or low ends) with respect to most measures of aggregate
community benefit expenditures, uncompensated care, medical education and
training, and medical research, as a percentage of total revenues. Its mix of
community benefit expenditures differed from the overall group, however. Other
urban and suburban hospitals reported higher aggregate community benefit
expenditures as uncompensated care and lower expenditures as medical
research as compared to the overall group.
• Includes those hospitals located in urban and suburban areas other than in
the largest 26 urban areas in the U.S.; they comprised 51% of the hospitals in
the study
• Patient mix – private insurance (44%), Medicare (30%), Medicaid (15%),
uninsured (8%), and other public programs (3%)
157
• Annual total revenues – the average and median total revenues were $169
million and $114 million, respectively; they comprised 48% of aggregate total
revenues overall – on average, this group’s revenue profile was close to that
of the overall group
• Excess revenues – excess revenues as a percentage of total revenues was
4.6% (same as that for overall group)
o the average and median excess revenue amounts were $7.7 million and
$3.1 million, respectively (similar to overall group)
o 20% of these hospitals reported a deficit, and 60% reported a deficit or
positive excess revenues less than 5% of total revenues
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 8.9% and 5.8%, respectively (similar to
that of overall group)
o Mix across types of community benefit expenditures – 69% of reported
community benefit expenditures were uncompensated care, followed by
medical education and training (21%), community programs (5%), and
medical research (5%)
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 10% and 5%, respectively
o Average and median percentage of total revenues reported as spent on
uncompensated care were 7.3% and 4.3%, respectively (similar to overall
group)
o 95% of these hospitals reported providing uncompensated care; a lesser
percentage reported treating all types of shortfalls as uncompensated
care, but a greater percentage reported treating bad debt as
uncompensated care, compared to overall
• Research, education and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (1.3% and 0.4%); medical
research (0.7% and 0.1%); community programs (0.8% and 0.2%)
o 80% of hospitals reported medical education and training, and 24%
reported medical research expenditures; 89% reported community
program expenditures of some type (lowest of the community types)
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (17%); under
5% of total revenues (46%)
o Uncompensated care under or equal to 1% of total revenues (17%); under
or equal to 3% of total revenues (39%); under or equal to 5% of total
revenues (55%)
Group of 15 Hospitals Reporting Highest Medical Research Expenditures
This group of 15 hospitals comprised 3% of all hospitals in the study, but
reported 93% of all medical research expenditures and 58% of all medical
158
education and training expenditures. This group reported larger total revenues
and excess revenues than did the other hospitals in the study, and reported a
materially different community benefit mix than did the other hospitals (e.g., it
was the only demographic that did not report uncompensated care as its largest
component of community benefit expenditures). The group’s higher reported
medical research expenditures materially increased the reported overall average
medical research expenditures, and altered the community benefit mix, of the
overall group.
• Annual total revenues – the average and median total revenues were both
$1.0 billion, compared to $179 million and $89 million, respectively, for the
overall group
• Excess revenues – the average and median excess revenues were $69
million and $58 million, respectively, compared to $8 million and $3 million,
respectively, for the overall group. Excess revenues as a percentage of total
revenues was 7%, compared to 5% overall.
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were both 19%, compared to 9% and 6%,
respectively, for the overall group
o Mix across types of community benefit expenditures – 45% of
aggregate community benefit expenditures were medical research,
followed by medical education and training (28%), uncompensated
care (22%), and community programs (5%)
o The community benefit mix for the overall group changed when this
group of hospitals was removed, with uncompensated care increasing
from 56% to 71% of overall community benefit expenditures, medical
education and training decreasing from 23% to 21%, medical research
decreasing from 15% to 1%, and community program expenditures
increasing from 6% to 7%
• Uncompensated care
o The average and median percentages of revenues reported as spent
on uncompensated care for the group of 15 hospitals was 6% and 3%,
respectively, compared to 7% and 4% respectively, for the overall
group
• Research, medical education and training expenditures
o The average and median percentages of revenues reported as spent
on medical research were 8.3% and 7.1%. The overall average and
median percentages for the overall group decreased from 1.6% and
0.2%, respectively, to 0.5% and 0.1%, respectively, when these
hospitals were removed from the overall group.
o The average and median percentages of revenues reported as spent
on medical education and training were 4.9% and 3.8%, respectively,
compared to 1.3% and 0.3%, respectively, overall.
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
159
o All hospitals in the group of 15 reported community benefit
expenditures greater than 5% of revenues
o Three hospitals in the group reported no uncompensated care; of the
remaining 12 hospitals in the group, four reported uncompensated care
expenditures in each of the following ranges: over 1% but less than or
equal to 3%, over 3% but less than or equal to 5%, and over 5%.
By Hospital Size (Annual Total Revenues)
The community benefit profile of the hospitals in the study generally followed a
pattern across the hospital size categories: the largest percentage of community
benefit expenditures was reported as spent on uncompensated care, generally
followed by medical education and training, community program expenditures,
and medical research. However, the relative percentages spent on each type of
community benefit expenditure varied across the hospital size categories.
Less than $25 million revenue size
This group had the highest percentage of uninsured patients and patients
covered by Medicare or other public insurance, and the lowest percentage of
patients covered by private insurance. This group had the lowest participation
rates in medical research and medical education and training, and generally had
relatively low participation rates in the various community programs. This group
had the lowest median percentage, but the highest average percentage, of total
revenues reported as spent on uncompensated care. The group of hospitals with
total revenues under $25 million reported the highest percentage of aggregate
community benefit expenditures spent on uncompensated care, and the lowest
percentages spent on medical research and medical education and training.
• Comprised 17% of hospitals in the study.
• Patient mix – private insurance (35%), Medicare (37%), Medicaid (16%),
uninsured (9%), and other public programs (5%).
• Annual total revenues – the average and median total revenues were $14
million and $15 million, respectively. Comprised 1% of total revenues.
• Excess revenues – excess revenues as a percentage of total revenues was
3.3% (lowest of the revenue sizes)
o the average and median excess revenue amounts were $0.5 million and
$0.3 million, respectively (also lowest of the revenue sizes)
o 35% of all hospitals in this revenue category reported a deficit (highest of
all revenue sizes), and 63% reported a deficit or positive excess revenues
less than 5% of total revenues
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 9.9% and 3.4%, respectively.
o Mix across types of community benefit expenditures – 93% of reported
community benefit expenditures were uncompensated care, followed by
community programs (6%), medical education and training (1%), and
medical research (0%).
• Uncompensated care
160

o Average and median percentage of patients provided uncompensated
care were 9.2% and 2.7%, respectively.
o Average and median percentage of total revenues reported as spent on
uncompensated care were 9.3% and 3.1%, respectively (highest average
percentage, but lowest median percentage of the revenue sizes).
o 93% reported providing uncompensated care; a greater percentage
reported treating most types of shortfalls as uncompensated care, but a
lesser percentage reported treating bad debt as uncompensated care,
compared to overall.
• Research, education and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (0.2% and 0.1%); medical
research (0.1% and 0.1%); community programs (0.9% and 0.2%)
o 48% reported medical education and training (compared to 77% overall);
82% reported community program expenditures of some type.
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues (34%); under
5% of total revenues (60%).
o Uncompensated care under or equal to 1% of total revenues (26%); under
or equal to 3% of total revenues (49%); under or equal to 5% of total
revenues (60%).
Over $500 million revenue size
71
The hospitals with total revenues over $500 million had the highest percentage of
Medicaid patients and the lowest percentage of Medicare patients. This group
had a participation rate in uncompensated care that was less than that of the
other hospital size groups, and in medical research that was greater than that of
the other groups. It had a relatively high participation rate in medical education
and training, and relatively low participation rates in most of the community
program expenditure types. This group had relatively high average and median
percentages of total revenues reported as spent on community benefit
expenditures. The group of hospitals with total revenues over $500 million had
relatively high percentages of aggregate community benefit expenditures
reported as spent on medical education and training and medical research, and
relatively low percentages reported as spent on uncompensated care and
community programs. This group’s average and median percentages of total
revenues spent on medical research and medical education and training were
the largest reported percentages of all of the hospital size categories.
• Comprised 7% of hospitals in the study.
• Patient mix – private insurance (46%), Medicare (23%), Medicaid (21%),
uninsured (8%), and other public programs (3%); lowest percentage of
Medicare and highest percentage of Medicaid of all revenue sizes.
71
Certain information included in this section is not displayed in the figures included earlier in the
report to prevent potential identification of respondent hospitals.
161
• Annual total revenues – the average and median total revenues for the group
were $964 million and $735 million, respectively. Comprised 40% of
revenues of all hospitals.
• Excess revenues – excess revenues as a percentage of total revenues was
5.5% (highest of the revenue sizes)
o The average and median excess revenue amounts were $53.4 million and
$38.3 million, respectively (also highest of the revenue sizes).
o 50% of the hospitals in this category reported a deficit or positive excess
revenues less than 5% of total revenues.
• Community benefit expenditure profile
o Average and median community benefit expenditures reported as a
percentage of total revenues were 12.4% and 10.5%, respectively.
o Mix across types of community benefit expenditures – 35% of reported
community benefit expenditures were uncompensated care, followed by
medical education and training (32%), medical research (29%), and
community programs (4%).
• Uncompensated care
o Average and median percentage of patients provided uncompensated
care were 16.6% and 5.3%, respectively.
o Average and median percentage of total revenues reported as spent on
uncompensated care were 5.6% and 4.7%, respectively.
o More than 90% reported providing uncompensated care; the greatest
percentage reported treating bad debt as uncompensated care, but the
lowest percentage reported treating private insurance, Medicare, Medicaid
and other public insurance as uncompensated care, compared to overall
• Research, education and community programs
o Average and median expenditures as percentage of total revenues,
respectively: medical education and training (4.5% and 3.8%) (highest of
any revenue size); medical research (3.9% and 1.2%) (highest of any
revenue size); community programs (0.7% and 0.2%)
o 92% reported medical education and training ; 67% reported medical
research expenditures (highest of any revenue size); 81% reported
community program expenditures of some type
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 5% of total revenues (19%)
o Uncompensated care under or equal to 1% of total revenues (9%); under
or equal to 3% of total revenues (33%); under or equal to 5% of total
revenues (60%)
Other Revenue Size Categories ($25 million to $500 million)
In general, the hospitals in the middle three revenue size categories (covering
$25 million to $500 million) reported data similar to the overall group of hospitals.
In this section, these three revenue size categories ($25 million to $100 million,
$100 million to $250 million and $250 million to $500 million) are discussed
together as there are few significant variations between the groups.
162
• The remaining three revenue size groups comprised 75% of the hospitals in
the study.
• Patient mix was similar to the overall group.
• Annual total revenues of the three groups comprised 59% of revenues of all
hospitals.
• Excess revenues as a percentage of total revenues ranged from 3.8% to
4.4%
• The percentage of hospitals that reported a deficit decreased as revenue size
increased.
• Within the three revenue sizes, the average and median community benefit
expenditures reported as a percentage of total revenues increased with revenue
size.
• Uncompensated care
o Within the three revenue sizes, the average and median percentages of
patients provided uncompensated care increased with revenue size.
o The percentage of hospitals within the three revenue sizes providing
uncompensated care was at least 95%. The percentage of community
benefit expenditures represented by uncompensated care ranged from
72% to 77%.
• Research, education and community programs
o Percentages of hospitals within the three revenue sizes providing
education and training ranged from 72% to 93%; providing research
ranged from under 10% to 49%; and providing community programs
ranged from 93% to 100%.
o Percentage of hospitals that reported conducting education and training
and medical research increased with revenue size.
• Comparison of community benefit expenditures and uncompensated care to
specified percentage of revenue levels
o Community benefit expenditures under 2% of total revenues for the three
revenue sizes ranged from under 10% to 30%; under 5% of total revenues
ranged from under 35% to 56%. The percentages decreased as revenue
size increased.
o Uncompensated care under or equal to 1% of total revenues for the three
revenue sizes ranged from 12% to 20%; under or equal to 3% of total
revenues ranged from 34% to 49%; under or equal to 5% of total revenues
ranged from 49% to 61%. The percentages decreased as revenue size
increased.
Other Findings and Observations
• Excess revenues analysis
o Excess revenues as a percentage of total revenues varied by community
type. The largest percentage (6%) was reported by the rural-non CAH
group of hospitals. The lowest was reported by CAHs (3.5%).
o Excess revenues as a percentage of total revenues increased with
revenue size (3.3% for smallest to 5.5% for largest; 4.6% overall). The
percentage of hospitals reporting a deficit decreased with revenue size.
163
• Community benefit expenditure analysis
• Overall community benefit expenditures
o High population hospitals reported spending a significantly higher
percentage of average and median total revenues on community
benefit expenditures compared with the other community types.
The lowest percentage was reported by CAHs.
o With the exception of the under $25 million category, the average
percentages of revenue spent on community benefit expenditures
increased with revenue size. The median percentages increased
with revenue size for all categories.
• Uncompensated care
o High population hospitals reported highest average and median
percentages of revenues spent on uncompensated care, and
highest average and median percentage of patients receiving
uncompensated care compared with all other community types.
CAHs reported spending the lowest average and median
percentages of revenue on uncompensated care and the lowest
average and median percentage of patients receiving
uncompensated care.
o Smaller hospitals tended to report spending higher percentages of
aggregate community benefit expenditures on uncompensated
care. The average and median percentages of revenue spent on
uncompensated care varied by revenue size. The highest average
was reported by hospitals in the under $25 million category (9.3%).
The average percentage of patients receiving uncompensated care
generally increased by revenue size, while the medians varied.
• Research
o High population hospitals reported conducting significantly more
research than any other community type.
o The percentage of hospitals that reported conducting medical
research increased with revenue size, with hospitals in the over
$500 million category reporting the highest average and median
percentages of revenues (3.9% and 1.2%, respectively).
• Concentration of expenditures
o Uncompensated care, medical research, and aggregate community
benefit expenditures were not evenly distributed by the hospitals in
the study, but were concentrated in a relatively small number of
hospitals. 14% of the hospitals reported 63% of the aggregate
uncompensated care expenditures; 26% of the hospitals reported
82% of the aggregate uncompensated care expenditures. 9% of
the hospitals reported 60% of the aggregate community benefit
expenditures; 19% of the hospitals reported 78% of the aggregate
community benefit expenditures. 15 hospitals reported 93% of the
aggregate reported medical research expenditures. This group
also reported 58% of the aggregate reported medical education and
training expenditures.
164
Per Capita Income and Health Insurance Coverage
• Per capita income categories
o Hospitals were divided into categories (below state average, at state
average, and above state average) based on comparison of county per
capita income and statewide per capita income.
o In a separate comparison, hospitals were divided into categories (low
per capita, high per capita, average per capita) based on comparison
of county per capita income and income of all U.S. counties.
o Key findings – There does not appear to be a correlation between
community benefit expenditures and per capita income levels.
However, under both methods, hospitals in the lower income
categories reported average and median percentages of revenues
spent on community benefit expenditures slightly lower than the overall
group. Hospitals in the lower income levels had the highest
representation in the lowest percentage of revenues spent on
community benefit expenditures category (i.e., community benefit
expenditures less than 2% of revenues).
• Health insurance coverage levels
o Hospitals were divided into categories (low health coverage rate,
medium health coverage rate, high health coverage rate) based on the
uninsured rate of the county where located.
o In a separate comparison, hospitals were divided into the same
categories based on the comparing the county’s percentage of insured
individuals with the percentages for counties nationwide.
o Key findings – The results suggest a correlation between community
benefit expenditures and health insurance coverage levels. The
average and median percentages of total revenues reported as spent
on community benefit expenditures increased as the health coverage
level decreased. Hospitals with low health coverage rates (high
percentage of uninsured individuals) reported the highest percentage
of hospitals reporting community benefit expenditures greater than
20% of revenues.
Executive Compensation Findings by Community Types
• The average and median salary, other compensation, and total
compensation was lower for rural hospitals (CAH and non-CAH) than for
the suburban and urban hospitals (high population and other urban and
suburban).
• The average and median total compensation amounts, respectively,
reported by the respondents in the study for the top management official
were as follows:
o For critical access hospitals - $178,000 and $169,000
o For non-CAH rural hospitals - $326,000 and $257,000
o For other urban and suburban hospitals - $521,000 and $426,000
o For high population hospitals - $781,000 and $566,000
165
o Overall, $490,000 and $377,000
Executive Compensation Findings by Revenue Size Categories
• The average and median salary, other compensation, and total
compensation increased as revenue levels increased.
• The average and median total compensation amounts, respectively,
reported by the respondents in the study for the top management official
were as follows:
o Revenues under $25 million - $171,000 and $140,000
o Revenues from $25 million to $100 million - $338,000 and
$263,000
o Revenues from $100 million to $250 million - $554,000 and
$461,000
o Revenues from $250 million to $500 million - $791,000 and
$642,000
o Revenues over $500 million - $1,092,000 and $786,000
o Overall, $490,000 and $377,000
Summary Tables of Certain Demographics and Reported Data
The following charts provide an overview of key demographics and community
benefit expenditure information reported by the hospitals in the study.
166

Figure 118. Summary of Reported Data - Demographic Information
Item
High
Population
CAHs Rural – non
CAHs
Other Urban
& Suburban
Revenues
under $25M
Revenues
over $500M
Overall
Number of hospitals 94 68 78 249 85 36 489
% of total hospitals 19% 14% 16% 51% 17% 7% 100%
Average total revenues
($M)
$389 $29 $93 $169 $14 $964 $179
Median total revenues
($M)
$196 $20 $68 $114 $15 $735 $89
% of hospitals with total
revenues < $100 M
25% * * 45% 100% 0% 53%
% of hospitals with total
revenue >$250 M
40% * * 21% 0% 100% 20%
% of total revenues 41% 2% 8% 48% 1% 40% 100%
% of total excess
revenues
40% 2% 11% 48% 1% 47% 100%
Average excess
revenues ($M)
$18 $1 $6 $8 $1 $53 $8
Median excess
revenues ($M)
$4 $1 $3 $3 $0 $38 $3
Excess revenues as %
of total revenues
5% 4% 6% 5% 3% 6% 5%
% hospitals with deficit
excess revenues
22% 34% 13% 20% 35% * 21%
% of hospitals with
excess revenue <2.5%
of total revenue
47% 44% 28% 40% 51% * 40%
% of hospitals with
excess revenue <5% of
total revenue
69% 66% 42% 61% 64% * 60%
% of patients with
Medicare
28% 36% 33% 30% 37% 23% 31%
% of patients with
Medicaid
19% 13% 13% 15% 16% 21% 15%
% of patients uninsured 8% 8% 7% 8% 9% 8% 8%
% of patients with
private insurance
44% 38% 44% 44% 35% 46% 43%
% of patients with other
public insurance
4% 3% 3% 3% 5% 3% 3%
M=million. * Not shown to prevent potential identification of respondent hospitals.
167

Figure 119. Summary of Reported Information - Community Benefit Expenditure Data
Item High
Population
CAHs Rural –
non CAHs
Other Urban
& Suburban
Revenues
under
$25M
Revenues
over
$500M
Overall
Community benefit expenditures as
% of total revenue (average)
13% 6% 8% 9% 10% 12% 9%
Community benefit expenditures as
% of total revenue (median)
10% 3% 3% 6% 3% 11% 6%
% of hospitals with community
benefit expenditures <2% of total
revenue
11% 39% 31% 17% 34% * 21%
% of hospitals with community
benefit expenditures <5% of total
revenue
32% 61% 57% 46% 60% * 47%
Uncompensated care as % of
community benefit expenditures
42% 77% 76% 69% 93% 35% 56%
Medical education & training as % of
community benefit expenditures
26% 4% 17% 21% 1% 32% 23%
Research as % of community benefit
expenditures
25% 0% 1% 5% 0% 29% 15%
Community program expenditures as
% of community benefit expenditures
7% 19% 6% 5% 6% 4% 6%
Uncompensated care as % of total
revenue (average)
8% 6% 8% 7% 9% 6% 7%
Uncompensated care as % of total
revenue (median)
5% 2% 3% 4% 3% 5% 4%
% of hospitals with uncompensated
care ≤ 1% of total revenue
8% 31% 25% 17% 26% 9% 19%
% of hospitals with uncompensated
care ≤ 3% of total revenue
33% 59% 52% 39% 49% 33% 43%
% of hospitals with uncompensated
care ≤5% of total revenue
52% 67% 65% 55% 60% 60% 58%
% of patients receiving
uncompensated care (average)
11% 7% 8% 10% 9% 17% 10%
% of patients receiving
uncompensated care (median)
6% 2% 2% 5% 3% 5% 3%
% of hospitals including bad debt as
uncompensated care
47% 34% 35% 48% 41% * 44%
% of hospitals including Medicare
shortfalls as uncompensated care
14% 24% 28% 19% 27% * 20%
% of hospitals including Medicaid
shortfalls as uncompensated care
16% 19% 34% 18% 21% * 20%
% of hospitals including private
insurance shortfalls as
uncompensated care
12% 28% 31% 15% 24% * 19%
% of hospitals including uninsured
shortfalls as uncompensated care
47% 53% 62% 47% 55% * 51%
% of hospitals including other public
program shortfalls as
uncompensated care
14% 22% 32% 14% 21% * 18%
* Not shown to prevent potential identification of respondent hospitals.
168
X. KEY OBSERVATIONS AND LESSONS LEARNED
Key Observations
1. There are multiple reasons why community benefit reporting varied across the
demographics. The study observed differences in a demographic group’s
general treatment of an activity as community benefit (e.g., lower percentages of
high population hospitals generally treated Medicare and other shortfalls as
uncompensated care than did other hospitals) and varying costing methodologies
used by the hospitals. Undoubtedly other factors, including many not analyzed in
this study, contributed to these variations. These factors and limitations must be
considered when reviewing the study’s findings. The new Form 990 Schedule H
reporting should reduce much of this variation in reporting.
2. Any revised standard would affect the different types and sizes of hospitals
differently depending upon the types of activities required to be taken into
account as community benefit, the quantitative measure (if any), and the extent
to which it provides exceptions or special rules to address special circumstances
and demographics (e.g., an exception from a quantitative standard if the
nonprofit hospital is the sole provider in the community).
3. A significant percentage of the hospitals in the study reported uncompensated
care and aggregate community benefit expenditures that were below various
“percentage of revenues” levels. For example, although the reported data is
subject to a number of limitations, the data indicates that a significant percentage
of all types and sizes of hospitals in the study would fail to satisfy an exemption
standard requiring uncompensated care expenditures of at least 3% of total
revenues, or aggregate community benefit expenditures of at least 5% of total
revenues. In large part, this is attributable to the concentration of
uncompensated care and aggregate community benefit expenditures in a
relatively small number of hospitals. The data also suggests that an attempt to
draw bright lines could have disproportionate impacts on hospitals depending
upon their size, where they are located, their community benefit mix, and other
hospital and community demographics.
4. Financial capacity also varied within the sample. In general, smaller
hospitals, including CAHs, had lower profit margins than larger hospitals in the
study. Also, the percentage of hospitals reporting deficits decreased as revenue
size increased.
5. Those respondent hospitals that reported information regarding how they
established executive compensation, including use of the rebuttable presumption
procedure, almost unanimously reported that they complied with key elements of
that procedure. High levels of compliance with the procedure were confirmed in
the examinations. The hospitals selected for examinations generally were
selected because they reported executive compensation amounts at relatively
high levels compared to other hospitals of similar size and type. The traditional
169
risk analysis and examination methodologies used in these examinations
confirmed widespread compliance with reasonable compensation standards.
More work must be done to assess the impact that the rebuttable presumption
procedure (including the use of for profit comparables) and the initial contract
exception (which provides that the Section 4958 excise tax does not apply to an
initial contract between an organization and a disqualified person) are having on
establishing executive compensation amounts and the ability of the IRS to
challenge compensation paid by many tax-exempt organizations.
6. Beginning with the 2009 tax year (2010 filing season), the Form 990,
Schedule H, Hospitals, should promote uniform and accurate reporting of
quantitative and qualitative community benefit information by tax-exempt
hospitals. Looking ahead, particular areas of inquiry are expected to include the
following: (a) accuracy of costing methodologies used to measure community
benefit; (b) medical research funded by for-profit organizations or not made
widely available to the public; (c) amounts reported as bad debt that are actually
attributable to charity care; (d) treating portions of Medicare shortfalls or certain
community building activities as community benefit; and (e) review of non-
quantifiable aspects of community benefit.
Lessons Learned
1. Many of the questionnaire’s questions proved to be ambiguous or difficult to
answer without a supplemental explanation, and some were criticized as being
judgmental or value laden. In future initiatives, the IRS will strive to work more
closely with other experts in designing the questions to be asked of the
respondents in the study, and will consider using pilots and samples to test a
draft questionnaire before implementation of the final questionnaire.
2. Studies of this nature are subject to disclosure rules designed to prevent
direct or indirect disclosure of a taxpayer’s identity or taxpayer information. This
caused the IRS to combine or omit certain data in the report, or sometimes use
general descriptions by using terms such as “nearly all” or “a few” instead of
referring to specific numbers or percentages. This was especially true in the
case of the study’s reporting of executive compensation examinations. The IRS
will more carefully consider disclosure issues at the front end as it designs future
questionnaires and studies.
3. The comprehensive nature of the study and the large volume of data
received, including significant amounts through narrative descriptions and
attachments, resulted in it taking longer to analyze the data and complete the
report than was expected. The release of an interim report to summarize the
aggregate data as reported to the IRS proved to be a valuable tool, both in
helping the IRS determine which areas required further work, and in assuring
transparency to the public regarding the process. The IRS anticipates using
interim reports in those future compliance initiatives it expects will take a
substantial period of time to complete. Further, studies of this nature require
170
dedication of significant resources of IRS personnel that must be trained for the
study’s specific tasks, and more training specific to the study should be built in at
the front end of these initiatives to maximize the quality and quantity of
information obtained from the study.
4. The questionnaire’s response rate was high and the overall quality of
responses was very good. The quality of the report is of course dependent on
the quality of responses and the willingness of the respondents to participate in
the study. The IRS will study ways to assure that response rates remain high in
future initiatives.
5. In areas where the tax-exempt organizations being studied operate in
competition with or along side of for-profit organizations, it would also be helpful
to have a deeper understanding of those for-profit organizations. Future
initiatives should attempt to take into account relevant studies or other bodies of
knowledge regarding such organizations, whenever possible.
6. The classification of respondents into various categories to analyze reported
data across certain demographics is helpful and interesting, but its utility depends
upon the soundness of the classifications. Although some classifications cannot
be determined until the data is received and preliminarily analyzed, to the extent
possible, the IRS should build possible classification criteria into the design of the
initial questionnaire.
171
APPENDIX A. LIST OF CHARTS AND TABLES
Below is a list of charts and tables (by Figure number) included in the Final
Report. In virtually all cases, information provided by community type is also
provided by revenue size in a corresponding figure.
Figure 1 through Figure 21 include general demographic information. Figure 1
shows overall patient insurance coverage. Figure 2 through Figure 7 show
financial information by revenue size. This information by community type is
included in Figure 8 through Figure 13. Figure 14 through Figure 16 display the
overlap between community type and revenue size. Figure 17 through Figure 21
include financial information by excess revenue categories.
Figure 22 through Figure 24 show patient information by community type. This
information is shown by revenue size in Figure 50 through Figure 52. Figure 25
through Figure 49 show reported community benefit expenditure information and
analysis, both on an aggregate basis and by the various components of
community benefit by community type. This same information is shown by
revenue size in Figure 53 through Figure 77.
Figure 78 and Figure 79 relate to the group of 15 hospitals that provided 93% of
the aggregate medical research expenditures. Figure 80 through Figure 85 show
the analysis of the inclusion of bad debt and various shortfalls in uncompensated
care. Figure 86 through Figure 89 show community benefit expenditures across
various income levels. Figure 90 through Figure 93 show community benefit
expenditures across various health insurance coverage levels. Figure 94 and
Figure 95 show the overlap between the income and health insurance coverage
groups.
Figure 96 through Figure 117 relate to the executive compensation portion of the
project.
Figure 118 and Figure 119 show a summary of demographics and reported
community benefit expenditure data.
FIGURE 1. AVERAGE PERCENTAGE OF INSURANCE COVERAGE................................................................ 22
FIGURE 2. DISTRIBUTION OF HOSPITALS BY AGGREGATE ANNUAL REVENUES........................................ 23
FIGURE 3. ANNUAL TOTAL REVENUES, TOTAL EXPENSES, AND EXCESS/DEFICIT REVENUE BY REVENUE
SIZE..................................................................................................................................................... 24
FIGURE 4. AVERAGE AND MEDIAN OF ANNUAL TOTAL REVENUES BY REVENUE SIZE .............................. 25
FIGURE 5. AVERAGE AND MEDIAN OF ANNUAL EXCESS REVENUE BY REVENUE SIZE ............................. 26
FIGURE 6. EXCESS REVENUE AS A PERCENTAGE OF TOTAL REVENUE .................................................... 27
FIGURE 7. DISTRIBUTION OF EXCESS REVENUE AS A PERCENTAGE OF ANNUAL TOTAL REVENUE BY
REVENUE SIZE.................................................................................................................................... 27
FIGURE 8. DISTRIBUTION OF HOSPITALS AND TOTAL REVENUES BY COMMUNITY TYPE.......................... 28
FIGURE 9. ANNUAL TOTAL REVENUES, TOTAL EXPENSES, AND EXCESS/DEFICIT REVENUE BY
COMMUNITY TYPE .............................................................................................................................. 29
FIGURE 10. AVERAGE AND MEDIAN ANNUAL TOTAL REVENUE BY COMMUNITY TYPE ............................. 30
FIGURE 11. AVERAGE AND MEDIAN ANNUAL EXCESS REVENUE BY COMMUNITY TYPE........................... 31
172
FIGURE 12. EXCESS REVENUE AS A PERCENTAGE OF TOTAL REVENUE BY COMMUNITY TYPE ............. 32
FIGURE 13. DISTRIBUTION OF EXCESS REVENUES AS A PERCENTAGE OF ANNUAL TOTAL REVENUE BY
COMMUNITY TYPE .............................................................................................................................. 32
FIGURE 14. NUMBER OF HOSPITALS BY REVENUE SIZE AND COMMUNITY TYPE...................................... 33
FIGURE 15. NUMBER OF HOSPITALS BY COMMUNITY TYPE AND REVENUE SIZE...................................... 33
FIGURE 16. NUMBER OF HOSPITALS BY REVENUE SIZE AND COMMUNITY TYPE...................................... 34
FIGURE 17. DISTRIBUTION OF HOSPITALS AND AGGREGATE EXCESS REVENUE BY EXCESS REVENUE
SIZE..................................................................................................................................................... 35
FIGURE 18. ANNUAL TOTAL REVENUES, TOTAL EXPENSES, AND EXCESS/DEFICIT REVENUES BY EXCESS
REVENUE SIZE.................................................................................................................................... 35
FIGURE 19. AVERAGE AND MEDIAN ANNUAL TOTAL REVENUE BY EXCESS REVENUE SIZE .................... 36
FIGURE 20. AVERAGE AND MEDIAN ANNUAL EXCESS REVENUE BY EXCESS REVENUE SIZE.................. 37
FIGURE 21. DISTRIBUTION OF EXCESS REVENUE AS A PERCENTAGE OF ANNUAL TOTAL REVENUE BY
EXCESS REVENUE SIZE...................................................................................................................... 38
FIGURE 22. DISTRIBUTION OF HEALTH INSURANCE COVERAGE BY COMMUNITY TYPE............................ 42
FIGURE 23. PERCENTAGE OF PATIENTS WITH INSURANCE COVERAGE BY COMMUNITY TYPE, ............... 42
FIGURE 24. PERCENTAGE OF PATIENTS WITH INSURANCE COVERAGE BY TYPE, BY COMMUNITY TYPE
............................................................................................................................................................ 43
FIGURE 25. NUMBER AND PERCENTAGE OF HOSPITALS REPORTING COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE CATEGORY AND COMMUNITY TYPE ............................................ 45
FIGURE 26. PERCENTAGE OF PATIENTS RECEIVING UNCOMPENSATED CARE BY COMMUNITY TYPE .... 46
FIGURE 27. PERCENTAGE OF TOTAL REVENUE SPENT ON UNCOMPENSATED CARE BY COMMUNITY
TYPE (AVERAGE AND MEDIANS)........................................................................................................ 47
FIGURE 28. PERCENTAGE OF REVENUE SPENT ON UNCOMPENSATED CARE BY COMMUNITY TYPE
(AVERAGES AND MEDIANS)................................................................................................................ 47
FIGURE 29. NUMBER AND PERCENTAGE OF HOSPITALS WITH REPORTED UNCOMPENSATED CARE AS A
PERCENTAGE OF TOTAL REVENUE, BY COMMUNITY TYPE ............................................................... 48
FIGURE 30. DISTRIBUTION OF HOSPITALS BY COMMUNITY TYPE BASED ON PERCENTAGE OF TOTAL
REVENUE SPENT ON UNCOMPENSATED CARE (AVERAGES) ........................................................... 48
FIGURE 31. DISTRIBUTION OF HOSPITALS BY COMMUNITY TYPE BASED ON PERCENTAGE OF TOTAL
REVENUE SPENT ON UNCOMPENSATED CARE (AVERAGES) ........................................................... 49
FIGURE 32. PERCENTAGE OF HOSPITALS REPORTING UNCOMPENSATED CARE EXPENDITURES AT OR
LESS THAN SPECIFIED PERCENTAGE OF REVENUE LEVELS............................................................. 50
FIGURE 33. PERCENTAGE OF TOTAL REVENUE SPENT ON MEDICAL RESEARCH BY COMMUNITY TYPE
(AVERAGES AND MEDIANS)................................................................................................................ 51
FIGURE 34. DISTRIBUTION OF HOSPITALS BY COMMUNITY TYPE BASED ON PERCENTAGE OF TOTAL
REVENUES SPENT ON MEDICAL RESEARCH...................................................................................... 52
FIGURE 35. PERCENTAGE OF TOTAL REVENUE SPENT ON MEDICAL EDUCATION AND TRAINING BY
COMMUNITY TYPE (AVERAGES AND MEDIANS) ................................................................................ 53
FIGURE 36. DISTRIBUTION OF HOSPITALS BY COMMUNITY TYPE BASED ON PERCENTAGE OF REVENUES
SPENT ON MEDICAL EDUCATION AND TRAINING (AVERAGES) ......................................................... 54
FIGURE 37. AMOUNTS AND PERCENTAGES OF COMMUNITY PROGRAM EXPENDITURES, BY EXPENDITURE
CATEGORY AND COMMUNITY TYPE.................................................................................................... 55
FIGURE 38. PERCENTAGES OF COMMUNITY PROGRAM EXPENDITURES BY EXPENDITURE CATEGORY AND
COMMUNITY TYPE .............................................................................................................................. 56
FIGURE 39. PERCENTAGE OF TOTAL REVENUES SPENT ON COMMUNITY PROGRAMS BY COMMUNITY
TYPE (AVERAGES AND MEDIANS) ...................................................................................................... 57
FIGURE 40. AMOUNTS AND PERCENTAGES OF TOTAL COMMUNITY BENEFIT EXPENDITURES BY
EXPENDITURE CATEGORY AND COMMUNITY TYPE............................................................................ 58
FIGURE 41. PERCENTAGE OF COMMUNITY BENEFIT EXPENDITURES BY EXPENDITURE CATEGORY AND
COMMUNITY TYPE .............................................................................................................................. 59
FIGURE 42. AVERAGE AND MEDIAN PERCENTAGE OF TOTAL REVENUE SPENT ON COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE CATEGORY AND COMMUNITY TYPE ............................................ 60
FIGURE 43. AVERAGE AND MEDIAN OF TOTAL REVENUE SPENT ON COMMUNITY BENEFIT EXPENDITURES
BY
COMMUNITY TYPE (AVERAGES AND MEDIANS) ........................................................................... 60
173
FIGURE 44. PERCENTAGE OF TOTAL REVENUE SPENT ON VARIOUS COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE AND COMMUNITY TYPE (AVERAGES) .......................................... 61
FIGURE 45. PERCENTAGE OF TOTAL REVENUES SPENT ON VARIOUS COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE AND COMMUNITY TYPE (MEDIANS) .......................................... 62
FIGURE 46. NUMBER AND PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT
EXPENDITURES AS PERCENTAGE OF TOTAL REVENUE, BY COMMUNITY TYPE ............................... 63
FIGURE 47. PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT EXPENDITURES AS
PERCENTAGE OF TOTAL REVENUE BY COMMUNITY TYPE ................................................................ 63
FIGURE 48. PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT EXPENDITURES AS
PERCENTAGE OF TOTAL REVENUE BY COMMUNITY TYPE ................................................................ 64
FIGURE 49. PERCENTAGE OF HOSPITALS REPORTING COMMUNITY BENEFIT EXPENDITURES LESS THAN
SPECIFIED PERCENTAGE OF REVENUE LEVELS ................................................................................ 64
FIGURE 50. DISTRIBUTION OF HEALTH INSURANCE COVERAGE BY REVENUE SIZE CATEGORIES ........... 68
FIGURE 51. PERCENTAGE OF PATIENTS WITH INSURANCE COVERAGE BY TOTAL REVENUE CATEGORY,
BY
TYPE OF COVERAGE...................................................................................................................... 69
FIGURE 52. PERCENTAGE OF PATIENTS BY TYPE OF INSURANCE COVERAGE, BY TOTAL REVENUE SIZE
............................................................................................................................................................ 70
FIGURE 53. NUMBER AND PERCENTAGE OF HOSPITALS REPORTING COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE CATEGORY AND REVENUE SIZE.................................................. 71
FIGURE 54. PERCENTAGE OF PATIENTS RECEIVING UNCOMPENSATED CARE BY REVENUE SIZE .......... 72
FIGURE 55. PERCENTAGE OF TOTAL REVENUE SPENT ON UNCOMPENSATED CARE BY REVENUE SIZE
(AVERAGE AND MEDIAN) .................................................................................................................... 73
FIGURE 56. PERCENTAGE OF TOTAL REVENUE SPENT ON UNCOMPENSATED CARE (AVERAGE AND
MEDIAN).............................................................................................................................................. 73
FIGURE 57. NUMBER AND PERCENTAGE OF HOSPITALS WITH REPORTED UNCOMPENSATED CARE AS A
PERCENTAGE OF TOTAL REVENUE BY REVENUE SIZE...................................................................... 74
FIGURE 58. DISTRIBUTION OF HOSPITALS BY REVENUE SIZE BASED ON PERCENTAGE OF TOTAL
REVENUES SPENT ON UNCOMPENSATED CARE (AVERAGES) .......................................................... 74
FIGURE 59. DISTRIBUTION OF HOSPITALS BY REVENUE SIZE BASED ON PERCENTAGE OF TOTAL
REVENUE SPENT ON UNCOMPENSATED CARE (AVERAGES) ........................................................... 75
FIGURE 60. PERCENTAGE OF HOSPITALS REPORTING UNCOMPENSATED CARE EXPENDITURES AT OR
LESS THAN SPECIFIED PERCENTAGES OF REVENUE LEVELS........................................................... 75
FIGURE 61. PERCENTAGE OF TOTAL REVENUE SPENT ON MEDICAL RESEARCH BY REVENUE SIZE
(AVERAGES AND MEDIANS)................................................................................................................ 77
FIGURE 62. DISTRIBUTION OF HOSPITALS BY REVENUE SIZE BASED ON PERCENTAGE OF TOTAL
REVENUE SPENT ON MEDICAL RESEARCH ........................................................................................ 78
FIGURE 63. PERCENTAGE OF TOTAL REVENUE SPENT ON MEDICAL EDUCATION AND TRAINING BY
REVENUE SIZE (AVERAGES AND MEDIANS)....................................................................................... 79
FIGURE 64. DISTRIBUTION OF HOSPITALS BY REVENUE SIZE BASED ON PERCENTAGE OF TOTAL
REVENUE SPENT ON MEDICAL EDUCATION AND TRAINING (AVERAGES) ........................................ 80
FIGURE 65. AMOUNT AND PERCENTAGE OF COMMUNITY PROGRAM EXPENDITURES BY EXPENDITURE
CATEGORY AND REVENUE SIZE ......................................................................................................... 81
FIGURE 66. PERCENTAGE OF COMMUNITY PROGRAM EXPENDITURES BY EXPENDITURE CATEGORY AND
REVENUE SIZE.................................................................................................................................... 82
FIGURE 67. PERCENTAGE OF TOTAL REVENUE SPENT ON COMMUNITY PROGRAMS BY REVENUE SIZE 83
FIGURE 68. AMOUNT AND PERCENTAGE OF TOTAL COMMUNITY BENEFIT EXPENDITURES BY
EXPENDITURE CATEGORY AND REVENUE SIZE ................................................................................. 84
FIGURE 69. PERCENTAGE OF COMMUNITY BENEFIT EXPENDITURES BY EXPENDITURE CATEGORY AND
REVENUE SIZE.................................................................................................................................... 85
FIGURE 70. AVERAGE AND MEDIAN PERCENTAGE OF TOTAL REVENUE SPENT ON COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE CATEGORY AND REVENUE SIZE.................................................. 86
FIGURE 71. AVERAGE AND MEDIAN TOTAL REVENUE SPENT ON COMMUNITY BENEFIT EXPENDITURES BY
EXPENDITURE AND REVENUE SIZE .................................................................................................... 87
FIGURE 72. PERCENTAGE OF TOTAL REVENUE SPENT ON VARIOUS COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE AND REVENUE SIZE CATEGORIES (AVERAGES) ........................ 88
174
FIGURE 73. PERCENTAGE OF TOTAL REVENUE SPENT ON VARIOUS COMMUNITY BENEFIT
EXPENDITURES BY EXPENDITURE AND REVENUE SIZE CATEGORIES (MEDIANS) ........................... 89
FIGURE 74. NUMBER AND PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT
EXPENDITURES AS A PERCENTAGE OF TOTAL REVENUE BY REVENUE SIZE.................................... 90
FIGURE 75. PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT EXPENDITURES AS A
PERCENTAGE OF TOTAL REVENUE BY REVENUE SIZE...................................................................... 90
FIGURE 76. PERCENTAGE OF HOSPITALS WITH REPORTED COMMUNITY BENEFIT EXPENDITURES AS A
PERCENTAGE OF TOTAL REVENUE BY REVENUE SIZE...................................................................... 91
FIGURE 77. PERCENTAGE OF HOSPITALS REPORTING COMMUNITY BENEFIT EXPENDITURES AT OR LESS
THAN SPECIFIED PERCENTAGES OF REVENUE LEVELS .................................................................... 91
FIGURE 78. COMMUNITY BENEFIT EXPENDITURE MIX ............................................................................... 96
FIGURE 79. ANNUAL TOTAL REVENUES, TOTAL EXPENSES, AND EXCESS/DEFICIT REVENUES .............. 97
FIGURE 80. PERCENTAGE OF HOSPITALS THAT INCLUDE VARIOUS SHORTFALL AMOUNTS OR BAD DEBT
IN
UNCOMPENSATED CARE BY COMMUNITY TYPE ............................................................................ 98
FIGURE 81. PERCENTAGE OF HOSPITALS THAT INCLUDE VARIOUS SHORTFALL AMOUNTS OR BAD DEBT
IN
UNCOMPENSATED CARE BY TYPE OF COVERAGE......................................................................... 99
FIGURE 82. PERCENTAGE OF HOSPITALS THAT INCLUDE VARIOUS SHORTFALL AMOUNTS OR BAD DEBT
IN
UNCOMPENSATED CARE BY REVENUE SIZE................................................................................ 101
FIGURE 83. PERCENTAGE OF HOSPITALS THAT INCLUDE VARIOUS SHORTFALL AMOUNTS OR BAD DEBT
IN
UNCOMPENSATED CARE BY TYPE OF SHORTFALL OR BAD DEBT............................................... 102
FIGURE 84. REPORTING DIFFERENCES WHEN SHORTFALLS AND BAD DEBT ARE INCLUDED IN
UNCOMPENSATED CARE (MEDIAN % OF REVENUE SPENT) .......................................................... 104
FIGURE 85. REPORTING DIFFERENCES WHEN SHORTFALLS AND BAD DEBTS ARE INCLUDED IN
UNCOMPENSATED CARE (AVERAGE % OF REVENUE SPENT)........................................................ 105
FIGURE 86. STATE PER CAPITA INCOME METHOD PERCENTAGE OF TOTAL REVENUES SPENT ON
COMMUNITY BENEFIT EXPENDITURES ACROSS VARIOUS PER CAPITA INCOME CATEGORIES
(AVERAGES AND MEDIANS).............................................................................................................. 108
FIGURE 87. STATE PER CAPITA INCOME METHOD DISTRIBUTION OF COMMUNITY BENEFIT
EXPENDITURES ACROSS PER CAPITA INCOME CATEGORIES ......................................................... 109
FIGURE 88. U.S. PER CAPITA INCOME METHOD PERCENTAGE OF ANNUAL TOTAL REVENUES
SPENT ON COMMUNITY BENEFIT EXPENDITURES ACROSS VARIOUS PER CAPITA INCOME
CATEGORIES (AVERAGES AND MEDIANS)....................................................................................... 111
FIGURE 89. U.S. PER CAPITA INCOME METHOD DISTRIBUTION OF COMMUNITY BENEFIT
EXPENDITURES ACROSS PER CAPITA INCOME CATEGORIES ......................................................... 113
FIGURE 90. COUNTY UNINSURED RATE METHOD PERCENTAGE OF ANNUAL TOTAL REVENUES
SPENT ON COMMUNITY BENEFIT EXPENDITURES ACROSS HEALTH COVERAGE CATEGORIES
(AVERAGES AND MEDIANS).............................................................................................................. 115
FIGURE 91. COUNTY UNINSURED RATE METHOD DISTRIBUTION OF COMMUNITY BENEFIT
EXPENDITURES ACROSS HEALTH COVERAGE CATEGORIES........................................................... 116
FIGURE 92. NATIONWIDE COMPARISON METHOD PERCENTAGE OF ANNUAL TOTAL REVENUE
SPENT ON COMMUNITY BENEFIT EXPENDITURES ACROSS HEALTH COVERAGE CATEGORIES
(AVERAGES AND MEDIANS).............................................................................................................. 118
FIGURE 93. NATIONWIDE COMPARISON METHOD DISTRIBUTION OF COMMUNITY BENEFIT
EXPENDITURES ACROSS HEALTH COVERAGE CATEGORIES........................................................... 119
FIGURE 94. DISTRIBUTION OF HOSPITALS AS CATEGORIZED BY THE STATE PER CAPITA INCOME
METHOD AND HEALTH INSURANCE COVERAGE CATEGORIES......................................................... 120
FIGURE 95. DISTRIBUTION OF HOSPITALS AS CATEGORIZED BY THE U.S. PER CAPITA INCOME METHOD
AND
HEALTH INSURANCE COVERAGE CATEGORIES ........................................................................ 121
FIGURE 96. SALARY AND OTHER COMPENSATION REPORTED FOR THE TOP MANAGEMENT OFFICIAL BY
COMMUNITY TYPE (AVERAGE AND MEDIAN).................................................................................... 125
FIGURE 97. SALARY AND OTHER COMPENSATION REPORTED FOR TOP MANAGEMENT OFFICIAL BY
REVENUE SIZE (AVERAGE AND MEDIAN) ........................................................................................ 125
FIGURE 98. TOTAL COMPENSATION REPORTED FOR THE TOP MANAGEMENT OFFICIAL BY COMMUNITY
TYPE (AVERAGE AND MEDIAN)......................................................................................................... 126
FIGURE 99. TOTAL COMPENSATION REPORTED FOR TOP MANAGEMENT OFFICIAL BY REVENUE SIZE
(AVERAGE AND MEDIAN) .................................................................................................................. 127
175
FIGURE 100. PERCENTAGE OF HOSPITALS THAT REPORTED HAVING A WRITTEN COMPENSATION POLICY
BY
COMMUNITY TYPE ....................................................................................................................... 128
FIGURE 101. PERCENTAGE OF HOSPITALS THAT REPORTED HAVING A WRITTEN COMPENSATION POLICY
BY
REVENUE SIZE............................................................................................................................. 129
FIGURE 102. INDIVIDUAL OR ENTITY REPORTED TO DETERMINE COMPENSATION ................................ 130
FIGURE 103. DISTRIBUTION OF INDIVIDUAL OR ENTITY REPORTED TO DETERMINE COMPENSATION BY
COMMUNITY TYPE ............................................................................................................................ 131
FIGURE 104. DISTRIBUTION OF INDIVIDUAL OR ENTITY REPORTED TO DETERMINE COMPENSATION BY
REVENUE SIZE.................................................................................................................................. 132
FIGURE 105. TOOLS USED TO DETERMINE COMPENSATION................................................................... 133
FIGURE 106. DISTRIBUTION OF REPORTED USE OF TOOLS TO DETERMINE COMPENSATION AMOUNTS
BY
COMMUNITY TYPE ....................................................................................................................... 134
FIGURE 107. DISTRIBUTION OF REPORTED USE OF TOOLS TO DETERMINE COMPENSATION AMOUNTS
BY
REVENUE SIZE............................................................................................................................. 135
FIGURE 108. FACTORS INCLUDED IN COMPARABILITY DATA................................................................... 136
FIGURE 109. PERCENTAGE OF HOSPITALS THAT CONSIDERED ALL COMPARABILITY FACTORS BY
COMMUNITY TYPE ............................................................................................................................ 137
FIGURE 110. PERCENTAGE OF HOSPITALS THAT CONSIDERED ALL COMPARABILITY FACTORS BY
REVENUE SIZE.................................................................................................................................. 137
FIGURE 111. PERCENTAGE OF HOSPITALS THAT CONSIDERED COMPARABILITY FACTORS BY
COMMUNITY TYPE ............................................................................................................................ 138
FIGURE 112. PERCENTAGE OF HOSPITALS THAT CONSIDERED COMPARABILITY FACTORS BY REVENUE
SIZE................................................................................................................................................... 138
FIGURE 113. PERCENTAGE OF HOSPITALS REPORTING A BUSINESS RELATIONSHIP WITH ITS OFFICERS,
DIRECTORS, TRUSTEES, OR KEY EMPLOYEES BY COMMUNITY TYPE ............................................ 139
FIGURE 114. PERCENTAGE OF HOSPITALS REPORTING A BUSINESS RELATIONSHIP WITH ITS OFFICERS,
DIRECTORS, TRUSTEES, OR KEY EMPLOYEES BY REVENUE SIZE.................................................. 140
FIGURE 115. TOTAL COMPENSATION PAID TO IDENTIFIED HIGHLY COMPENSATED INDIVIDUALS OF
EXAMINED HOSPITALS...................................................................................................................... 142
FIGURE 116. TOTAL COMPENSATION TO IDENTIFIED HIGHLY COMPENSATED INDIVIDUALS OF EXAMINED
HOSPITALS BY POSITION TITLE ........................................................................................................ 143
FIGURE 117. EXAMINATION RESULTS - TOOLS USED TO DETERMINE COMPENSATION ......................... 144
FIGURE 118. SUMMARY OF REPORTED DATA - DEMOGRAPHIC INFORMATION....................................... 167
FIGURE 119. SUMMARY OF REPORTED INFORMATION - COMMUNITY BENEFIT EXPENDITURE DATA..... 168
176
APPENDIX B
FORM 13790, Compliance Check Questionnaire Tax-Exempt Hospitals
177

Form 13790
(May 2006)
COMPLIANCE CHECK QUESTIONNAIRE
TAX-EXEMPT HOSPITALS
OMB No.
1545-2015
This questionnaire asks for information about your hospital and how it operates. Answer the questions based on
your hospital’s most recently completed tax period. If additional space is needed, attach additional sheets.
Please complete the questionnaire and follow the instructions in the letter for returning the information to us.
PART I – ORGANIZATION
Name of Hospital: EIN:
Most Recently Completed Tax Period:
PART II – OPERATIONS
1)
Please indicate the category below that best described your hospital or the type of service it provided to the majority of
admissions. Check only one box.
General medical and surgical
Hospital unit of an institution (prison, college etc)
Hospital unit within an institution for the mentally retarded
Surgical
Psychiatric
Tuberculosis and other respiratory diseases
Cancer
Heart
Alcoholism and other chemical dependency
Organization is not a §501(c)(3) hospital. If you checked
this box, stop here and return the questionnaire to us.
Obstetrics and gynecology
Eye, ear, nose and throat
Rehabilitation
Orthopedic
Chronic disease
Institution for the mentally retarded
Acute long-term care
Other — Specify:
Patients
Inpatients Outpatients
Emergency Room
Patients
2) What were the total number of:
3)
How many had private insurance?
4) How many had Medicare?
5) How many had Medicaid?
6) How many had other public insurance?
7) How many had no insurance?
8) Did your hospital deny medical services to any individuals with:
a) private insurance? Yes No
If yes, please explain.
b) Medicare? Yes No
If yes, please explain.
c) Medicaid? Yes No
If yes, please explain.
Form 13790 (5-2006)
Page 1 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

d) other public health insurance? Yes No
If yes, please explain.
e) no insurance? Yes No
If yes, please explain.
Emergency Room
9)
Did your hospital operate an emergency room? Yes No
If no, please explain.
10)
What were the emergency room’s hours of operation?
24 hours a day, 365 days a year
Other — please explain.
11) Did your hospital’s emergency room have a trauma center? Yes No
12) If yes, what was the trauma center’s level of certification?
Level I
Level II
Level III
Level IV
Level V
Other — please describe.
13) Did your hospital’s emergency room provide services to all members of the community regardless of their ability to pay?
Yes No
If no, please explain.
14)
Did your hospital’s emergency room deny services to any individuals that requested such services? Yes No
If yes, please explain.
Board of Directors
15) How many directors were on your hospital’s board?
16)
What was the professional background of each director?
Please indicate the number of directors in each category listed below.
Accounting
Government
Philanthropy
Banking/Finance
Insurance
Public/Elected Official
Business
Law Religion
Community Service
Management
Retail
Education/Academia
Manufacturing
Social Services
Fine Arts
Medicine/Health Care
Other (specify)
17)
How often did the board of directors meet?
Monthly Quarterly Annually
Other — please describe.
18) On average, how many of the directors were present at each meeting?
Form 13790 (5-2006)
Page 2 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

Medical Staff Privileges
19) Were all qualified physicians in your community eligible for medical staff privileges at your hospital? Yes No
If no, please explain.
20) Have you denied any qualified physician’s application for medical staff privileges? Yes No
If yes, please explain.
Medical Research
21)
Did your hospital conduct any medical research programs? Yes No
If yes, please answer questions 22 through 24. If no, go to question 25.
22)
How much did your hospital spend on medical research programs? $
23)
How much of your hospital’s funding for medical research came from:
a) public sources (for example, government grants) $
b) private sources (for example, contracts with for-profit corporations) $
24) Did your hospital limit public access to the findings or results from any of its medical research programs? Yes No
If yes, please explain.
25) How much did your hospital provide in grants to individuals or organizations to fund
medical research programs? $
26) Was public access limited to the findings or results from any medical research programs for which your hospital provided
grants? Yes No
If yes, please explain.
27)
Did your hospital conduct any medical trial studies? Yes No
If yes, answer questions 28 and 29. If no, go to question 30.
28)
How much of your hospital’s funding for medical trial studies came from:
a) public sources (for example, government grants) $
b) private sources (for example, contracts with for-profit corporations) $
29) Did your hospital limit public access to the findings or results from any of its medical trial studies? Yes No
If yes, please explain.
Professional Medical Education and Training
30)
Did your hospital conduct any professional medical education and training programs?
If yes, answer questions 31 and 32. If no, go to question 33.
Yes No
31)
How much did your hospital spend on professional medical education and training programs? $
32)
How much of your funding for professional medical education and training came from:
a) public sources (for example, government grants) $
b) private sources (for example, contracts with for-profit corporations) $
Form 13790 (5-2006)
Page 3 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

33) Did your hospital provide grants to individuals or organizations to fund professional medical education and
training programs? Yes No
If yes, how much did it spend? $
Uncompensated Care
34)
Did your hospital have a written policy stating the circumstances under which it would provide
uncompensated care? Yes No
Please explain.
35) How many individuals received uncompensated care from your hospital?
36)
How much did your hospital spend on uncompensated care? $
37) Did your hospital treat as uncompensated care the excess of what it charged for services and the amount:
a) private insurance paid or allowed for such services
(including any patient co-payments and deductibles)? Yes No
If yes, please explain.
b) Medicare paid or allowed for such services (including any patient co-payments and deductibles)? Yes No
If yes, please explain.
c) Medicaid paid or allowed for such services (including any patient co-payments and deductibles)? Yes No
If yes, please explain.
d) other public insurance paid or allowed for such services
(including any patient co-payments and deductibles)? Yes No
If yes, please explain.
e) individuals without insurance paid your hospital for such services? Yes No
Please explain.
38)
Did your hospital treat bad debts as uncompensated care? Yes No
Please explain.
39)
Did your hospital treat any other items or costs as uncompensated care? Yes No
If yes, please explain.
40) Did your hospital report its expenditures for uncompensated care to a state government? Yes No
If yes, what amount did it report? $
Form 13790 (5-2006)
Page 4 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

41) Did your hospital provide:
a) inpatient services to any individual without compensation? Yes No
If yes, please describe your policy.
b) outpatient services to any individual without compensation? Yes No
If yes, please describe your policy.
c) emergency room services to any individual without compensation? Yes No
If yes, please describe your policy.
42)
If you answered yes to 41 a, b, or c, indicate below, for each category of patient, when your hospital determined that it
would provide services to any individual without compensation? Check all that apply.
At or Less than 30 30 to 90 More than 90 When Other
before days after days
after days after insurance (explain
providing providing providing providing denied all or below)
services services services services part of claim
Inpatient
Outpatient
Emergency
Room
If you checked the other box, please describe:
Billing Practices
43) Did your hospital require all individuals to pay, or make arrangements to pay, prior to, or at the time it provided:
a) inpatient services? Yes No
b) outpatient services? Yes No
c) emergency room services? Yes No
44) In the space provided below, please explain your payment policies for:
a) inpatients
b) outpatients
Form 13790 (5-2006)
Page 5 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

c) emergency room patients
45)
How many days after your hospital provided services did it send the patient a bill?
46)
How many days after the billing date did the patient have to pay for services?
47) If a patient failed to pay for services, how many notices did your hospital send before it began collection actions?
48) Did your hospital refer all past due bills to collection agencies? Yes No
49) Did your hospital enter into installment agreements or other extended payment arrangements
with patients who were unable to pay? Yes No
50)
Please describe the circumstances in which you would enter into installment agreements or other extended payment
arrangements with patients who were unable to pay.
51) How many days after a patient had not paid all or part of a bill did your hospital classify it as a bad debt?
52) Did your hospital charge all patients the same price for the same services? Yes No
If yes, go to question 57. If no, answer questions 53-56.
53) Did your hospital charge patients with private insurance higher prices for hospital services than patients with public
insurance (including Medicare and Medicaid)? Yes No
Please explain.
54) Did your hospital charge patients with no insurance higher prices for hospital services than patients with public insurance
(including Medicare and Medicaid)? Yes No
Please explain.
55) Did your hospital charge patients with no insurance higher prices for hospital services than patients with
private insurance? Yes No
Please explain.
56) Did your hospital charge individuals different prices for hospital services based on their income, assets or
ability to pay for such services? Yes No
Please explain.
Form 13790 (5-2006)
Page 6 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

Community Programs
57) Did your hospital provide medical screening programs for the community? Yes No
If yes, answer questions 58 through 60. If no, go to question 61.
58)
How much did your hospital spend on medical screening programs for the community? $
59) Were all members of the community eligible for your hospital’s medical screening programs? Yes No
If no, please explain.
60) Did the hospital charge a fee for any community medical screening programs? Yes No
If yes, please explain.
61)
Did your hospital provide immunization programs for the community? Yes No
If yes, answer questions 62 through 64. If no, go to question 65.
62)
How much did your hospital spend on immunization programs for the community? $
63) Were all members of the community eligible for your hospital’s immunization programs? Yes No
If no, please explain.
64) Did your hospital charge a fee for its community immunization programs? Yes No
If yes, please explain.
65)
Did your hospital provide any lectures, seminars or other educational programs for the community? Yes No
If yes, answer questions 66 through 68. If no, go to question 69.
66)
How much did your hospital spend on lectures, seminars and other educational programs
for the community? $
67)
Were all members of the community eligible for your hospital’s community educational programs? Yes No
If no, please explain.
68)
Did your hospital charge a fee for its community education programs? Yes No
If yes, please explain.
69) Did your hospital conduct studies on the unmet health care needs of the community? Yes No
If yes, how much did your hospital spend on these studies? $
70)
Did your hospital have programs to improve access to health care for individuals who lacked insurance? Yes No
If yes, how much did your hospital spend on these programs? $
71) Did your hospital produce or distribute newsletters or publications that provided information to the community
on health care issues? Yes No
If yes, how much did your hospital spend on these newsletters or publications? $
Form 13790 (5-2006)
Page 7 Catalog Number 48381U Department of the Treasury — Internal Revenue Service
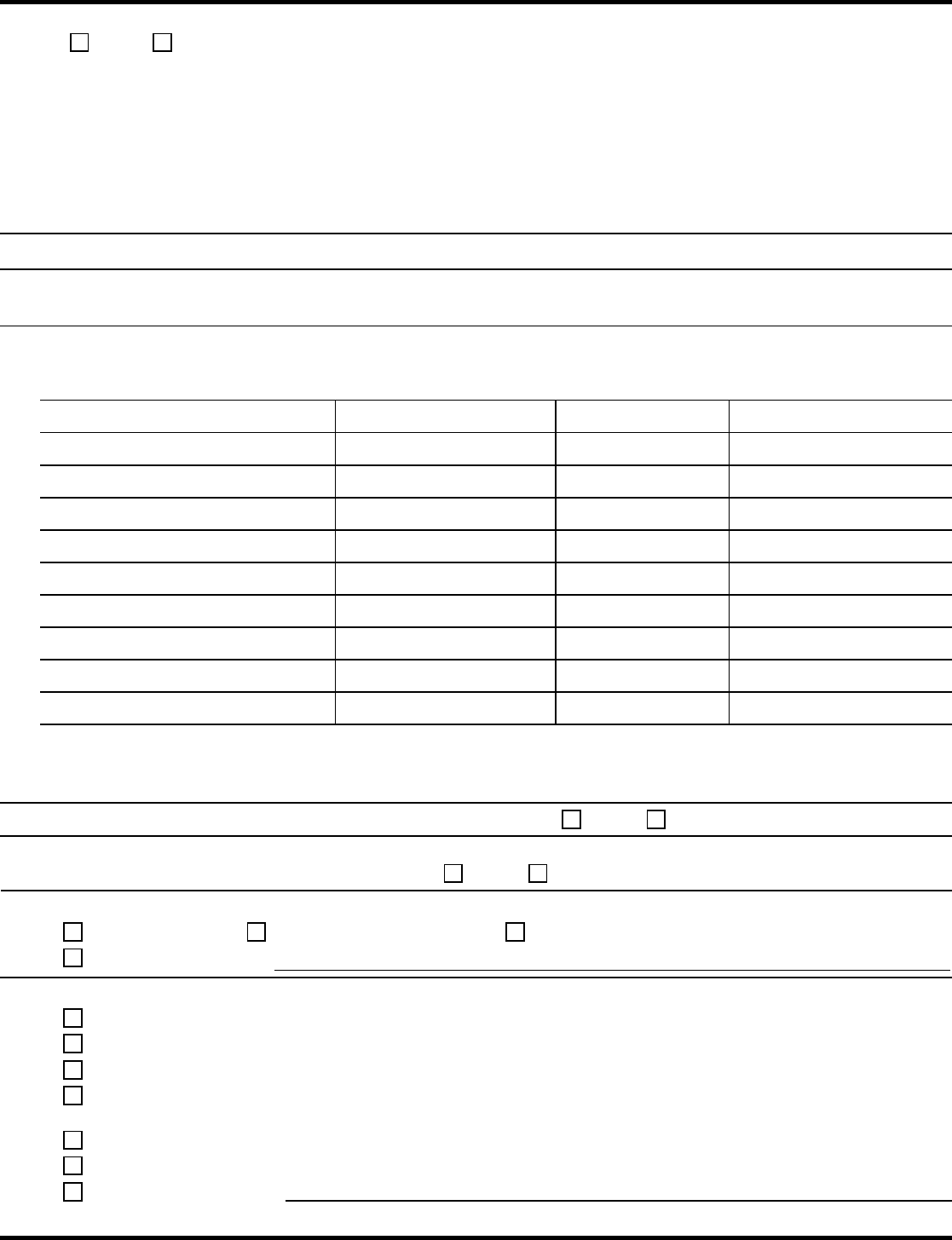
72) Did your hospital have any other programs or activities that promoted health for the benefit of the community?
Yes No
If yes, please explain and indicate how much was spent on these programs and activities.
PART III – COMPENSATION PRACTICES
Please answer the questions in this part as it pertains to employees in your hospital who are disqualified persons within the
meaning of Internal Revenue Code (IRC) Section 4958(f)(1).
1) Please provide the names and titles of your hospital’s officers, directors, trustees and key employees and amounts
of salary and other compensation paid by your hospital to such officers, directors, trustees and key employees.
Add additional sheets if necessary.
Name Title
Salary
1
Other Compensation
2
1
Salary includes all forms of cash and non-cash compensation received whether paid currently or deferred.
2
Other Compensation includes contributions to employee benefit plans and deferred compensation plans, and
expense allowances from non-accountable plans.
2) Did your hospital have a formal written compensation policy? Yes No
3)
Was compensation approved, in advance, by individuals that did not have a conflict of interest with the
compensation arrangement being approved? Yes No
4) Who in your hospital set the compensation for officers, directors, trustees, and key employees? Check all that apply.
Officers Board of Directors Compensation Committee
Other — please explain:
5)
Please check any of the following that your hospital used to determine compensation amounts:
Published surveys of compensation at similar institutions;
Internet research on compensation at similar institutions conducted by your employees;
Phone survey(s) of compensation at similar institutions conducted by your hospital’s employees;
Outside expert report prepared specifically for your hospital by an expert employed by your hospital for this
purpose;
Outside expert report prepared by an expert employed by an unrelated organization;
Written offers of employment from similar institutions; and
Other — please describe:
Form 13790 (5-2006)
Page 8 Catalog Number 48381U Department of the Treasury — Internal Revenue Service

6)
Please check the appropriate boxes, in the following chart, regarding factors included in the comparability data used by
your hospital:
COMPARABILITY FACTORS:
YES NO
Was factor checked used for all
§ 4958
(f)(1) employees? *
Yes No*
Level of Employee Education and Experience
Specific Responsibilities of Position
Same Geographic or Metropolitan Area
Services of a Similar Nature Provided
Similar Number of Beds, Admissions, or Outpatient Visits
Other Factors. Please explain.
*If no, please explain.
7)
Did your hospital’s comparability data include information from other tax-exempt hospitals? Yes No
If no, please explain.
8) Was your hospital’s actual compensation set within the range of comparability data? Yes No
If no, please explain.
9) Did your hospital have a business relationship with any of its officers, directors, trustees or
key employees other than through their position as officers, directors, trustees, or key employees? Yes No
If yes, identify the individuals and describe the business relationship below.
Name Title Description of Business Relationship
Privacy Act and Paperwork Reduction Act Notice. We ask for the information on this form to carry out the Internal Revenue laws of the
United States. We need it to ensure that you are complying with these laws.
The IRS may not conduct or sponsor, and an organization is not required to pr
ovide the information requested on a form that is subject to
the Paperwork Reduction Act unless the form displays a valid OMB number. Books or records relating to a collection of information must be
retained as long as their contents may become material in the administration of any Internal Revenue law. Generally, tax returns and tax
return information are confidential, as required by 26 U.S.C. 6103 and 6104.
Form
13790 (5-2006)
Page 9 Catalog Number 48381U Department of the Treasury — Internal Revenue Service
Clear Button
