
Effects
of
Prophylactic
Antibiotics
in
Vascular
Surgery
A
Prospective,
Randomized,
Double-Blind
Study
PER-OLOF
HASSELGREN,
M.D.,
PH.D.,
LARS
IVARSSON,
TORSTEN
SEEMAN,
M.D.,
PH.D.
In
a
prospective,
randomized,
double-blind
study
the
effects
on
infection
rates
of
a
1-day
and
a
3-day
course
of
cefuroxime
versus
placebo
were
studied
in
patients
undergoing
peripheral
vascular
surgery.
During
a
30-month
study
period
211
patients
were
randomized
to
one
of
three
treatment
groups:
Group
I
Placebo;
Group
II
cefuroxime
1
day;
Group
III
cefuroxime
3
days.
Cefuroxime
was
administered
intravenously
(1.5
g
every
8
hours)
and
the
first
dose
was
given
1
hour
before
surgery.
Wound
infection
rates
in
the
three
treatment
groups
were:
Group
I
16.7%;
Group
II
3.8%
(p
<
0.05
vs
placebo);
Group
III
4.3%
(p
<
0.05
vs
placebo).
One
graft
infection
occurred
in
110
patients
at
risk
(0.9%)
and
this
occurred
in
the
placebo
group.
No
allergic
reactions
or
other
side
effects
were
noted
in
any
of
the
treatment
groups.
No
cefuroxime-resistant
bacteria
were
found
in
Group
II
or
III.
In
conclusion,
prophylactic
administration
of
cefuroxime
during
1
day
significantly
reduced
the
incidence
of
infectious
complications
following
peripheral
vascular
surgery.
Extension
of
the
prophylaxis
beyond
the
day
of
surgery
offered
no
additional
effect.
The
study
supports
the
use
of
short-term
prophylactic
antibiotics
in
vascular
surgery.
IITOUND
AND
GRAFT
INFECTIONS
are
severe
compli-
VY
cations
in
vascular
surgery
and
may
result
in
sig-
nificant
morbidity
and
even
mortality."2
Therefore,
every
effort
should
be
made
to
reduce
the
incidence
of
septic
complications
in
these
patients.
The
role
of
prophylactic
antibiotics
in
vascular
surgery
has
been
debated
for
many
years
and
only
two
prospective,
randomized,
blinded
studies
exist
that
support
their
ef-
ficacy.3'4
On
the
other
hand,
large
series
of
patients
have
been
reported
with
low
infection
rates
without
the
routine
use
of
antibiotics.56
Results
have
also
been
presented
suggesting
that
infection
rates
do
not
change
with
the
use
of
prophylactic
antimicrobials.7
In
a
recent
clinical
review
on
synthetic
vascular
graft
infections8
it
was
stated
that
"
. .
the
exact
role
of
prophylactic
systemic
antibiotics
continues
to
be
debated,
predominantly
because
of
the
difficulties
in
obtaining
sufficient
statistical
numbers
in
M.D.,
PH.D.,
BO
RISBERG,
M.D.,
PH.D.,
From
the
Department
of
Surgery,
Ostra
S/ukhuset,
University
of
Goteborg,
G6teborg,
Sweden
a
prospective
randomized
series
to
be
significant."
Also,
the
length
of
prophylaxis
in
this
kind
of
surgery
has
not
been
defined.
Thus,
further
studies
on
the
effect
of
pro-
hylactic
antibiotics
in
vascular
surgery
are
desirable.
This
report
presents
the
results
from
a
prospective,
randomized,
double-blind
study
evaluating
the
effects
of
a
1-day
and
a
3-day
course
of
cefuroxime
versus
placebo
on
infection
rates
in
peripheral
vascular
surgery.
Cefuroxime,
a
second
generation
cephalosporin,
was
selected
as
a
prophylactic
agent
for
several
reasons.
First,
it
is
,B-lactamase
resistant
and
has
an
antibiotic
spectrum
covering
most
staphylococci
as
well
as
most
of
the
skin-
flora
in
the
genitoperineal
region.
Second,
its
pharma-
cokinetic
properties
are
well
suited
for
perioperative
use
since
high
interstitial
fluid
concentrations
are
rapidly
ob-
tained
following
administration.9
Finally,
being
a
ceph-
alosporin,
it
would
to
some
extent
allow
comparisons
with
previous
reports
on
cephalosporin
prophylaxis
in
vascular
surgery.
Methods
Selection
of
Patients
and
Randomization
The
study
was
carried
out
from
January
1981
through
June
1983.
Patients
who
were
scheduled
for
vascular
re-
constructive
surgery
of
the
lower
limbs
and
patients
un-
dergoing
acute
femoral
embolectomy
or
thrombectomy
were
considered
eligible
for
participation
in
the
study.
The
following
groups
of
patients
were
not
included:
1)
patients
scheduled
for
an
aortic
bifurcation
graft
(these
patients
received
prophylactic
cefuroxime),
2)
patients
having
received
antibiotics
within
1
week
prior
to
surgery,
3)
patients
with
cellulitis
or
wet
gangrene
on
lower
ex-
tremities,
and
4)
patients
with
a
history
of
penicillin
or
cephalosporin
allergy.
86
Reprint
requests:
Per-Olof
Hasselgren,
M.D.,
Department
of
Surgery,
Ostra
Sjukhuset,
S-416
85
Goteborg,
Sweden.
Submitted
for
publication:
November
28,
1983.

*
ANTIBIOTICS
IN
VASCULAR
SURGERY
87
TABLE
1.
Age,
Sex,
and
Risk
Factors
in
Study
Population
Prophylactic
Regimen
Group
I
Group
II
Group
III
(Placebo)
(Cefuroxime
1
Day)
(Cefuroxime
3
Days)
All
Groups
Study
population
Randomized
77
59
75
211
Excluded
11
7
6
24
Analyzed
66
52
69
187
Age
and
sex
Mean
age
(range)
66.4
(33-89)
67.6
(39-86)
67.8
(30-85)
67.2
(30-89)
Age
>
70
years
27
(40.9)
22
(42.3)
33
(47.8)
82
(43.9)
Male
51
(77.3)
39
(75.0)
40
(58.0)
130
(69.5)
Risk
factors
Obesity
2
(3.0)
4
(7.7)
1
(1.4)
7
(3.7)
Diabetes
11
(16.7)
10
(19.2)
12
(17.4)
33
(17.6)
Steroids
0
1
(1.9)
4
(5.8)
5
(2.7)
Rest
pain
and/or
dry
gangrene
26
(39.4)
35
(67.3)
35
(50.7)
96
(51.3)
Synthetic
graft
25
(37.9)
22
(42.3)
23
(33.3)
70
(37.4)
Operation
>
4
hr
4
(6.3)
6
(11.5)
2
(2.9)
12
(6.4)
Emergency
operation
4
(6.3)
9
(17.3)
8
(11.6)
21
(11.2)
Numbers
in
parenthesis
indicate
per
cent
except
for
mean
age
where
they
indicate
range.
The
following
criteria
were
used
for
exclusion
from
Patients
considered
eligible
for
inclusion
were
randomly
evaluation:
1)
death
from
noninfectious
cause
within
1
allocated
to
one
of
three
treatment
groups:
Group
I
Pla-
month
of
surgery,
2)
recent
antibiotic
therapy
overlooked
cebo;
Group
II
Cefuroxime
1
day;
Group
III
Cefuroxime
when
patient
was
included
in
the
study,
3)
aortic
bifur-
3
days.
During
the
30-month
study
period
211
patients
cation
graft
(these
patients
were
initially
scheduled
for
were
allocated
to
either
of
the
treatment
groups.
Informed
iliac
artery
or
distal
aortic
endarterectomy
and
cefuroxime
consent
was
obtained
from
all
patients
and
the
study
was
treatment
was
started
during
surgery
immediately
upon
approved
by
the
Ethical
Committee
at
the
University
of
the
decision
to
change
surgical
tactics),
4)
early
reoperation
Goteborg.
due
to
noninfectious
complication,
5)
early
postoperative
In
December
1982
the
codes
were
revealed
for
a
pre-
administration
of
antibiotics
inadvertently
or
because
of
liminary
analysis
of
the
results.
At
that
time
about
150
urinary
tract
or
pulmonary
infection,
and
6)
allergic
re-
patients
had
entered
the
study.
The
results
indicated
a
actions.
reduced
infection
rate
in
Group
III
as
compared
to
Group
TABLE
2.
Reasons
for
Exclusion
from
Evaluation
of
Efficacy
Prophylactic
Regimen
Group
I
Group
II
Group
III
Reason
for
Exclusion
(Placebo)
(Cefuroxime
I
Day)
(Cefuroxime
3
Days)
All
Groups
Recent
antibiotic
therapy
0
2
1
3
Aortic
bifurcation
graft
2
0
1
3
Reoperation
due
to
noninfectious
complications
2
2
1
5
Antibiotics
administered
after
surgery
1
0
0
I
Death
within
I
month
from
noninfectious
cause
6
2
3
11
Allergy
0
1
0
1
TABLE
3.
Wound
Infections
Among
Patients
Receiving
Placebo
or
Cefuroxime
Prophylactic
Regimen
Group
I
Group
II
Group
III
(Placebo)
(Cefuroxime
I
Day)
(Cefuroxime
3
Days)
All
Groups
Infections/patients
11/66
2/52
3/69
16/187
Patients
infected
(%)
16.7
3.8*
4.3*
8.6
*
p
<
0.05
vs.
placebo.

88
HASSELGREN
AND
OTHERS
Ann.
Surg
*
July
1984
4)~~~~~c
2
.
7
i
c
X
X
B
o
a
B
i
§}i
E~~~~~~~~~~~~~~~~~>
o
0~~
,}
-
cJ°°
°.2e!
00
0~~~~~~~~~
'
0
E
0
~~~~0.
0
ZJ~
C
~
J
~
:
Z
Zci
0
.~~~~~~~~~~~~~~~~~~~~~~0c
o
e
0
0
_
00
N
N
0
0
N
0
0
'6
0
0
>.
0
~
0
>.
>.
0
.)
0
0
02~
0
.2
2
2
~~~~~~~~~4912
01
10C~O
2
CU)
WI,
4)W
)
.-

ANTIBIOTICS
IN
VASCULAR
SURGERY
4)&
10
I
.o
2
4)
e
.~~~~~~~~4
~~,
~ ~
r
,,
Cu0
,
3
*
Co
co
co
co
co
4-
-
co
*,
-
*
-
.
00
0
0
v
E
*
-
*-
e;
*
y
°
i
E
z
'3'
*a
Lx.0
Lx.
r-
1.0
r-
e1
0o
>b
*0
en
2
-
4)
4-
.
0
E
x
2
I
Ai
89
I
but
the
difference
was
not
statistically
significant.
In
Group
II,
however,
four
of
52
patients
(7.7%)
were
clas-
sified
as
infected,
which
did
not
seem
to
be
different
from
the
infection
rate
in
Group
I
at
that
time.
It
was
then
considered
unethical
to
further
allocate
patients
to
Group
II.
The
randomization
procedure
was
subsequently
changed
and
allocation
only
to
Groups
I
and
III
was
used
during
the
rest
of
the
study.
This
decision
was
made
together
with
an
independent
study
monitor
and
resulted
in
larger
study
Groups
I
and
III
than
Group
II
(see
Re-
sults).
In
the
final
analysis
of
the
results
it
became
evident
that
two
patients
in
Group
II
draining
sanguineous
fluid
had
been
wrongly
classified
as
infected
in
the
preliminary
analysis
since
aerobic
and
anaerobic
cultures
were
sterile.
A
similar
mistake
was
made
in
one
patient
in
Group
I
who
was
also
classified
as
infected
in
the
preliminary
analysis
of
the
results
but
had
sterile
cultures.
All
patients
scheduled
for
elective
surgery
were
washed
with
4%
chlorhexidine
soap
(Hibiclens,
whole
body
shower
including
hairwash)
three
times
on
the
day
before
operation.
Shaving
of
the
patients
was
performed
im-
mediately
prior
to
surgery.
When
femoropopliteal
bypass
was
performed
two
techniques
were
used
for
harvesting
the
saphenous
vein;
either
one
long
continuous
incision
from
the
groin
to
the
knee
region
or
multiple
small
in-
cisions.
Except
for
this
difference
the
surgical
technique
was
standardized
and
equal
among
the
participating
sur-
geons.
Administration
of
Antibiotics
A
coded
box
containing
nine
numbered
vials
was
as-
signed
to
each
patient.
In
Group
I
all
vials
contained
20
ml
of
saline;
in
Group
11
1.5
g
of
cefuroxime
was
dissolved
in
vials
number
one
to
three
while
the
rest
of
the
vials
contained
only
saline;
in
Group
III
all
vials
contained
1.5
g
of
cefuroxime
dissolved
in
20
ml
of
saline.
The
vials
were
indistinguishable
by
gross
inspection.
The
content
of
vial
number
one
was
administered
intravenously
with
the
on-call
medications
(about
1
hour
before
surgery)
and
the
rest
of
the
vials
were
given
by
number
every
8
hours
during
3
days.
Evaluation
of
Patients
Each
patient
was
evaluated
daily
for
signs
of
allergic
reactions,
fever,
and
wound
infection.
Wound
infection
was
defined
as
accumulation
of
pus
that
drained
spon-
taneously
or
after
debridement.
Graft
infection
was
de-
fined
as
any
persistent
wound
infection
communicating
with
graft
material.
Incisions
that
drained
lymph
or
san-
gineous
fluid
that
was
sterile
were
not
classified
as
infected.
Specimens
were
taken
from
infected
wounds
and
were
cultured
using
standard
bacteriologic
methods.
The
an-
aerobic
bacteria
were
classified
using
gas
chromatography.
Vol.
200
*
No.
I
(A
cd

Ann.
Surg.
*
July
1984
TABLE
5.
Incidence
of
Wound
Infections
by
Surgical
Procedure
and
Prophylactic
Regimen
Infections/Patients
(%)
Group
I
Group
II
Group
III
Procedure
(Placebo)
(Cefuroxime
1
Day)
(Cefuroxime
3
Days)
All
Groups
Iliacofemoral
bypass
1/4
(25.0)
0/0
0/1
1/5
(20.0)
Iliac
artery
endarterectomy
1/6
(16.7)
0/6
0/6
1/18
(5.6)
Femoropopliteal
bypass
8/34
(23.5)
1/20
(5.0)
3/29
(10.3)
12/83
(14.5)
Axillofemoral
and
femorofemoral
bypass
1/4
(25.0)
0/5
0/4
1/13
(7.7)
Femoral/popliteal
endarterectomy
0/5
0/5
0/8
0/18
Femoral-lower
leg
bypass
0/2
0/2
0/5
0/9
Tromb/embolectomy
0/8
1/12
(8.3)
0/13
1/33
(3.0)
Exploration
0/3
0/2 0/3
0/8
Each
instance
of
possible
infection
was
evaluated
by
at
least
two
of
the
authors
prior
to
assignment
to
the
infected
or
noninfected
category.
The
code
was
not
revealed
on
any
of
the
patients
until
the
status
of
the
wound
had
been
decided.
In
three
patients,
however,
the status
of
the
wound
was
reevaluated
due
to
sterile
cultures
as
described
above.
All
patients
were
followed
up
for
at
least
30
days,
which
means
that
most
patients
were
also
evaluated
fol-
lowing
discharge
from
hospital.
Statistics
Fisher's
Exact
Test
(two-tailed)
was
used
for
statistical
evaluation.
Results
Age
and
sex
distribution
in
the
three
treatment
groups
and
the
incidence
of
various
risk
factors
known
to
be
associated
with
high
infection
rates
are
shown
in
Table
1.
For
reasons
given
above
the
number
of
patients
was
less
in
Group
II
than
in
Group
I
and
III.
However,
mean
age
and
relative
distribution
of
old
patients
and
risk
factors
did
not
differ
significantly
between
the
three
study
groups.
Of
21
1
patients
randomized
in
the
study,
24
were
excluded
for
reasons
presented
in
Table
2.
The
patient
excluded
because
of
allergy
in
Group
II
did
not
actually
show
an
allergic
reaction
but
wanted
to
withdraw
from
the
study
on
the
first
postoperative
day
due
to
a
previously
forgotten
skin
rash
experienced
following
penicillin
several
years
ago.
The
patient
was
excluded
from
the
study
when
this
information
was
obtained.
No
infectious
complication
occurred.
No
patients
experienced
allergic
reactions
or
other
side
effects
in
any
of
the
treatment
groups
during
the
present
study.
Wound
infection
rates
in
187
patients
eligible
for
eval-
uation
of
prophylaxis
efficacy
are
shown
in
Table
3.
The
incidence
of
wound
infections
was
significantly
lower
in
both
groups
of
cefuroxime-treated
patients
than
in
the
placebo
group.
No
further
reduction
of
wound
infection
rate
was
achieved
when
the
course
of
prophylaxis
was
prolonged
from
1
to
3
days.
There
was
only
one
graft
infection
in
110
patients
at
risk
(0.9%)
and
this
occurred
in
the
placebo
group
(1/44,
2.3%).
Details
regarding
the
patients
with
infectious
compli-
cations
are
listed
in
Table
4.
The
mean
interval
from
operation
to
discovery
of
wound
infection
was
13
days
in
the
placebo
group,
16
days
in
Group
II,
and
13
days
in
Group
III.
Staphylococcus
aureus
was
found
in
seven
of
13
infected
wounds
(54%)
from
which
specimens
were
taken
for
culture.
In
one
placebo
patient
cefuroxime-
resistant
enterobacteria
were
found.
No
cefuroxime-re-
sistant
bacteria
were
found
in
Groups
II
or
III.
Three
patients
were
seen
in
the
emergency
room
because
of
wound
infection
discovered
after
discharge
from
the
hos-
pital,
and
in
these
cases
specimens
were
unfortunately
not
taken
for
bacteriologic
culture.
The
incidence
of
wound
infection
by
surgical
procedure
is
presented
in
Table
5.
The
highest
infection
rates
oc-
curred
following
iliacofemoral
and
femoropopliteal
bypass
operations.
As
can
also
be
noted
in
Table
5
the
different
kinds
of
surgical
procedures
were
evenly
distributed
among
the
treatment
groups.
Infection
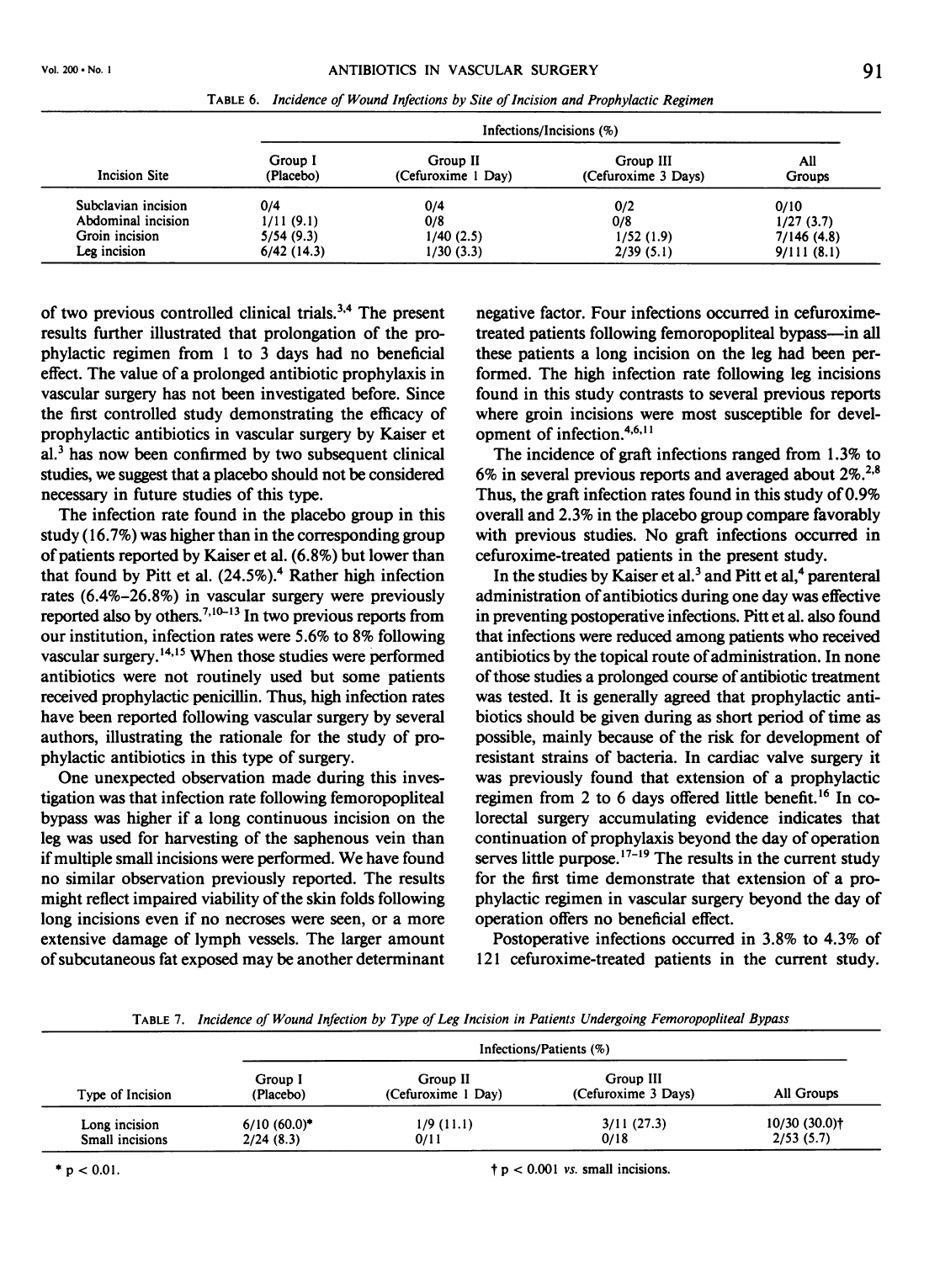
rates
analyzed
by
site
of
skin
incision
are
presented
in
Table
6.
The
highest
infection
rate
was
found
in
leg
incisions.
Infection
rate
for
groin
incisions
was
4.8%.
Analysis
of
the
results
showed
that
wound
infection
rate
following
femoropopliteal
bypass
was
higher
if
a
long
incision
on
the
leg
was
used
for
harvesting
the
saphenous
vein
than
if
multiple
small
incisions
were
performed
(Ta-
ble
7).
In
Group
I
a
long
leg
incision
was
used
in
29%
of
the
femoropopliteal
bypasses.
The
corresponding
figure
in
Group
II
was
38%
and
in
Group
III
45%.
Thus,
the
lower
infection
rates
following
femoropopliteal
bypass
in
Groups
II
and
III
as
compared
to
Group
I
could
not
be
explained
from
a
lower
proportion
of
operations
with
long
leg
incision
in
these
groups.
Discussion
This
study
demonstrated
the
efficacy
of
prophylactic
antibiotics
in
vascular
surgery,
thus
confirming
the
results
90
HASSELGREN
AND
OTHERS
ANTIBIOTICS
IN
VASCULAR
SURGERY
TABLE
6.
Incidence
of
Wound
Infections
by
Site
of
Incision
and
Prophylactic
Regimen
Infections/Incisions
(%)
Group
I
Group
II
Group
III
All
Incision
Site
(Placebo)
(Cefuroxime
1
Day)
(Cefuroxime
3
Days)
Groups
Subclavian
incision
0/4
0/4
0/2
0/10
Abdominal
incision
1/11
(9.1)
0/8
0/8
1/27
(3.7)
Groin
incision
5/54
(9.3)
1/40
(2.5)
1/52
(1.9)
7/146
(4.8)
Leg
incision
6/42
(14.3)
1/30
(3.3)
2/39
(5.1)
9/111
(8.1)
of
two
previous
controlled
clinical
trials.3
4
The
present
results
further
illustrated
that
prolongation
of
the
pro-
phylactic
regimen
from
1
to
3
days
had
no
beneficial
effect.
The
value
of
a
prolonged
antibiotic
prophylaxis
in
vascular
surgery
has
not
been
investigated
before.
Since
the
first
controlled
study
demonstrating
the
efficacy
of
prophylactic
antibiotics
in
vascular
surgery
by
Kaiser
et
al.3
has
now
been
confirmed
by
two
subsequent
clinical
studies,
we
suggest
that
a
placebo
should
not
be
considered
necessary
in
future
studies
of
this
type.
The
infection
rate
found
in
the
placebo
group
in
this
study
(16.7%)
was
higher
than
in
the
corresponding
group
of
patients
reported
by
Kaiser
et
al.
(6.8%)
but
lower
than
that
found
by
Pitt
et
al.
(24.5%).4
Rather
high
infection
rates
(6.4%-26.8%)
in
vascular
surgery
were
previously
reported
also
by
others.7"l'3
In
two
previous
reports
from
our
institution,
infection
rates
were
5.6%
to
8%
following
vascular
surgery.'4"5
When
those
studies
were
performed
antibiotics
were
not
routinely
used
but
some
patients
received
prophylactic
penicillin.
Thus,
high
infection
rates
have
been
reported
following
vascular
surgery
by
several
authors,
illustrating
the
rationale
for
the
study
of
pro-
phylactic
antibiotics
in
this
type
of
surgery.
One
unexpected
observation
made
during
this
inves-
tigation
was
that
infection
rate
following
femoropopliteal
bypass
was
higher
if
a
long
continuous
incision
on
the
leg
was
used
for
harvesting
of
the
saphenous
vein
than
if
multiple
small
incisions
were
performed.
We
have
found
no
similar
observation
previously
reported.
The
results
might
reflect
impaired
viability
of
the
skin
folds
following
long
incisions
even
if
no
necroses
were
seen,
or
a
more
extensive
damage
of
lymph
vessels.
The
larger
amount
of
subcutaneous
fat
exposed
may
be
another
determinant
negative
factor.
Four
infections
occurred
in
cefuroxime-
treated
patients
following
femoropopliteal
bypass-in
all
these
patients
a
long
incision
on
the
leg
had
been
per-
formed.
The
high
infection
rate
following
leg
incisions
found
in
this
study
contrasts
to
several
previous
reports
where
groin
incisions
were
most
susceptible
for
devel-
opment
of
infection.4'6"l1
The
incidence
of
graft
infections
ranged
from
1.3%
to
6%
in
several
previous
reports
and
averaged
about
2%.2.8
Thus,
the
graft
infection
rates
found
in
this
study
of
0.9%
overall
and
2.3%
in
the
placebo
group
compare
favorably
with
previous
studies.
No
graft
infections
occurred
in
cefuroxime-treated
patients
in
the
present
study.
In
the
studies
by
Kaiser
et
al.3
and
Pitt
et
al,4
parenteral
administration
of
antibiotics
during
one
day
was
effective
in
preventing
postoperative
infections.
Pitt
et
al.
also
found
that
infections
were
reduced
among
patients
who
received
antibiotics
by
the
topical
route
of
administration.
In
none
of
those
studies
a
prolonged
course
of
antibiotic
treatment
was
tested.
It
is
generally
agreed
that
prophylactic
anti-
biotics
should
be
given
during
as
short
period
of
time
as
possible,
mainly
because
of
the
risk
for
development
of
resistant
strains
of
bacteria.
In
cardiac
valve
surgery
it
was
previously
found
that
extension
of
a
prophylactic
regimen
from
2
to
6
days
offered
little
benefit.'6
In
co-
lorectal
surgery
accumulating
evidence
indicates
that
continuation
of
prophylaxis
beyond
the
day
of
operation
serves
little
purpose.'7
'9
The
results
in
the
current
study
for
the
first
time
demonstrate
that
extension
of
a
pro-
phylactic
regimen
in
vascular
surgery
beyond
the
day
of
operation
offers
no
beneficial
effect.
Postoperative
infections
occurred
in
3.8%
to
4.3%
of
121
cefuroxime-treated
patients
in
the
current
study.
TABLE
7.
Incidence
of
Wound
Infection
by
Type
of
Leg
Incision
in
Patients
Undergoing
Femoropopliteal
Bypass
Infections/Patients
(%)
Group
I
Group
II
Group
III
Type
of
Incision
(Placebo)
(Cefuroxime
1
Day)
(Cefuroxime
3
Days)
All
Groups
Long
incision
6/10
(60.0)* 1/9
(11.1)
3/11
(27.3)
10/30
(30.0)t
Small
incisions
2/24
(8.3)
0/11
0/18
2/53
(5.7)
91
Vol.
200
-No.
I
*
p
<
0.01.
t
p
<
0.001
vs.
small
incisions.

92
HASSELGREN
AND
OTHERS
Ann.
Surg
July
1984
Kaiser
et
al.3
used
cefazolin
for
prophylaxis
and
the
in-
fection
rate
among
225
patients
was
0.9%.
The
corre-
sponding
figure
was
0%
of
55
cephradine-treated
patients
in
the
study
by
Pitt
et
al.4
Comparison
of
results
in
dif-
ferent
studies,
however,
give
limited
information
since
they
are
influenced
by
criteria
for
patient
inclusion
and
exclusion,
definitions
of
infectious
complications,
time
of
follow-up,
type
of
surgery
performed,
etc.
To
evaluate
if
one
type
of
antibiotics
is
more
effective
than
another
in
reducing
rate
of
postoperative
infections
a
controlled
study
would
of
course
be
necessary
to
perform.
One
im-
portant
factor
influencing
the
outcome
of
different
pro-
phylactic
regimens
is
the
study
population.
Mean
age
among
our
patients
was
about
8
years
higher
than
in
the
study
by
Pitt
et
al.4
The
frequency
of
patients
older
than
70
years
was
about
twice
as
high
in
our
study
population
and
most
risk
factors,
with
the
exception
of
obesity,
were
more
frequent
in
our
patients.
In
the
study
by
Pitt
et
al.
patients
operated
on
for
varicose
veins
were
included
and
in
fact
constituted
the
largest
single
group
of
patients
in
that
study.
This
further
indicates
that
the
present
study
population
and
that
of
Pitt
et
al.
differed
in
too
many
respects
to
enable
a
strict
comparison.
In
the
study
by
Kaiser
et
al.,3
age,
sex
distribution,
and
frequency
of
dif-
ferent
risk
factors
in
the
study
population
were
not
pre-
sented
so
comparisons
cannot be
made.
In
conclusion,
prophylactic
administration
of
cefurox-
ime
during
1
day
significantly
reduced
the
incidence
of
infectious
complications
following
peripheral
vascular
surgery.
Extension
of
the
prophylactic
regimen
beyond
the
day
of
operation
offered
no
additional
effect.
This
study
strongly
supports
the
use
of
short-term
prophylactic
antibiotics
in
vascular
surgery.
References
1.
Goldstone
J,
Moore WS.
Infection
in
vascular
prostheses:
clinical
manifestations
and
surgical
managements.
Am
J
Surg
1974;
128:225-233.
2.
Casali
RE,
Tucker
WE,
Thompson
BW,
Read
RC.
Infected
prosthetic
grafts.
Arch
Surg
1980;
115:577-580.
3.
Kaiser
AB,
Clayson
KR,
Mulherin
JL,
et
al.
Antibiotic
prophylaxis
in
vascular
surgery.
Ann
Surg
1978;
188:283-289.
4.
Pitt
HA,
Postier
RG,
MacGowan
WAL,
et
al.
Prophylactic
antibiotics
in
vascular
surgery.
Topical,
systemic,
or
both?
Ann
Surg
1980;
192:356-364.
5.
Fry
WJ,
Lindenauer
SM.
Infections
complicating
the
use
of
plastic
arterial
implants.
Arch
Surg
1967;
94:600-608.
6.
Szilagyi
DE,
Smith
RF,
Elliot
JP,
et
al.
Infection
in
arterial
recon-
struction
with
synthetic
grafts.
Ann
Surg
1972;
176:321-333.
7.
Evans
C,
Pollock
AV. The
reduction
of
surgical
wound
infections
by
prophylactic
parenteral
cephaloridine.
Br
J
Surg
1973;
60:434-
437.
8.
Bunt
TJ.
Clinical
review.
Synthetic
vascular
graft
infections:
I.
Graft
infections.
Surgery
1983;
93:733-746.
9.
Browning
AK,
House
CA.
Pharmacokinetics
of
cefuroxime
com-
pared
to
other
cephalosporins.
In
Wood
C,
Rue
Y,
eds.
Cefu-
roxime
Update.
London:
Academic
Press,
1981;
87-99.
10.
Evans
C,
Pollock
AV,
Rosenberg
IL.
The
reduction
of
surgical
wound
infections
by
topical
cephaloridine:
a
controlled
trial.
Am
J
Surg
1974;
61:133-135.
11.
Christenson,
J,
Eklof
B.
Synthetic
arterial
grafts:
II.
Infection
com-
plications.
Scand
J
Thorac
Cardiovasc
Surg
1977;
11:43-50.
12.
Hammarsten
J,
Holm
J,
Schersten
T.
Infections
in
vascular
surgery.
J
Cardiovasc
Surg
1977;
18:543-545.
13.
Szilagyi
DE,
Elliot
JP.
Antibiotic
prophylaxis
in
vascular
grafting.
In
Duma
RJ,
ed.
Infections
of
Prosthetic
heart
valves
and
vascular
grafts.
Baltimore:
University
Park
Press,
1977;
323-342.
14.
Hasselgren
PO,
Sliljo
A,
Fornander
J,
et
al.
Postoperative
wound
infections-A
prospective
study
in
a
newly
opened
hospital.
Ann
Chir
Gynaecol
1980;
69:269-272.
15.
Hasselgren
PO,
Siljo
A,
Fornander
J,
et
al.
Postoperative
wound
infections
in
patients
with
long
preoperative
hospital
stay.
Acta
Chir
Scand
1982;
148:473-477.
16.
Goldman
DA,
Hopkins
CC,
Karchmer
AW,
et
al.
Cephalothin
prophylaxis
in
cardiac
valve
surgery:
a
prospective
double-blind
comparison
oftwo-day
and
six-day
regimens.
J
Thorac
Cardiovasc
Surg
1977;
73:470-479.
17.
Stone
HH,
Haney
BB,
Kolb
LD,
et
al.
Prophylactic
and
preventive
antibiotic
therapy.
Ann
Surg
1979;
189:691-699.
18.
Darell
JH,
Galland
RB.
Infections
following
abdominal
operations:
its
diagnosis,
prevention
and
treatment.
In
Taylor
S,
ed.
Recent
Advances
in
Surgery:
10.
Edinburgh:
Churchill-Livingstone,
1980;
202-223.
19.
Ivarsson
L,
Darle
N,
Kewenter
JG,
et
al.
Short-term
systemic
pro-
phylaxis
with
cefoxitin
and
doxycycline
in
colorectal
surgery.
A
prospective,
randomized
study.
Am
J
Surg
1982;
144:257-261.
