
Tactical Combat Casualty Care
quick reference guide
First edition
Copyright 2017

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
EDITOR:
HAROLD R. MONTGOMERY, ATP
MSG(RET), U.S. ARMY
FRANK K. BUTLER, MD
CAPT(RET), U.S. NAVY
STEPHEN D. GIEBNER, MD, MPH
CAPT(RET), U.S. NAVY
WIN KERR, ATP
CURTIS C. CONKLIN, ATP
MSG, U.S. ARMY
DANIEL M. MORISSETTE, ATP
MSG, U.S. ARMY
Copyright Statement:
The copyright holder of this publication assigns unlimited royalty-free
reproduction licensing exclusively to the United States Government and NATO
member governments. U.S. Government Printing Offices, specifically
Department of Defense installation printing services are authorized to
reproduce this publication for use by military personnel.
The copyright holder retains reproduction and royalty licensing for all other
individuals or organizations except the U.S. Government. No part of the
material protected by this copyright may be reproduced or utilized in any form,
electronic or mechanical, including photography, recording, or by any
information storage and retrieval system, without written permission from the
copyright owner.
MICHAEL A. REMLEY, ATP
SFC, U.S. ARMY
TRAVIS A. SHAW, NREMT-P
MSGT, U.S. AIR FORCE
JEREMY K. TORRISI
SCPO, U.S. NAVY
THOMAS A. RICH, NREMT-P
CMSGT, U.S. AIR FORCE
CONSULTANTS & REVIEWERS
Copyright, 2017 by HR Montgomery
ISBN: 978-0-692-90697-2

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TABLE OF CONTENTS
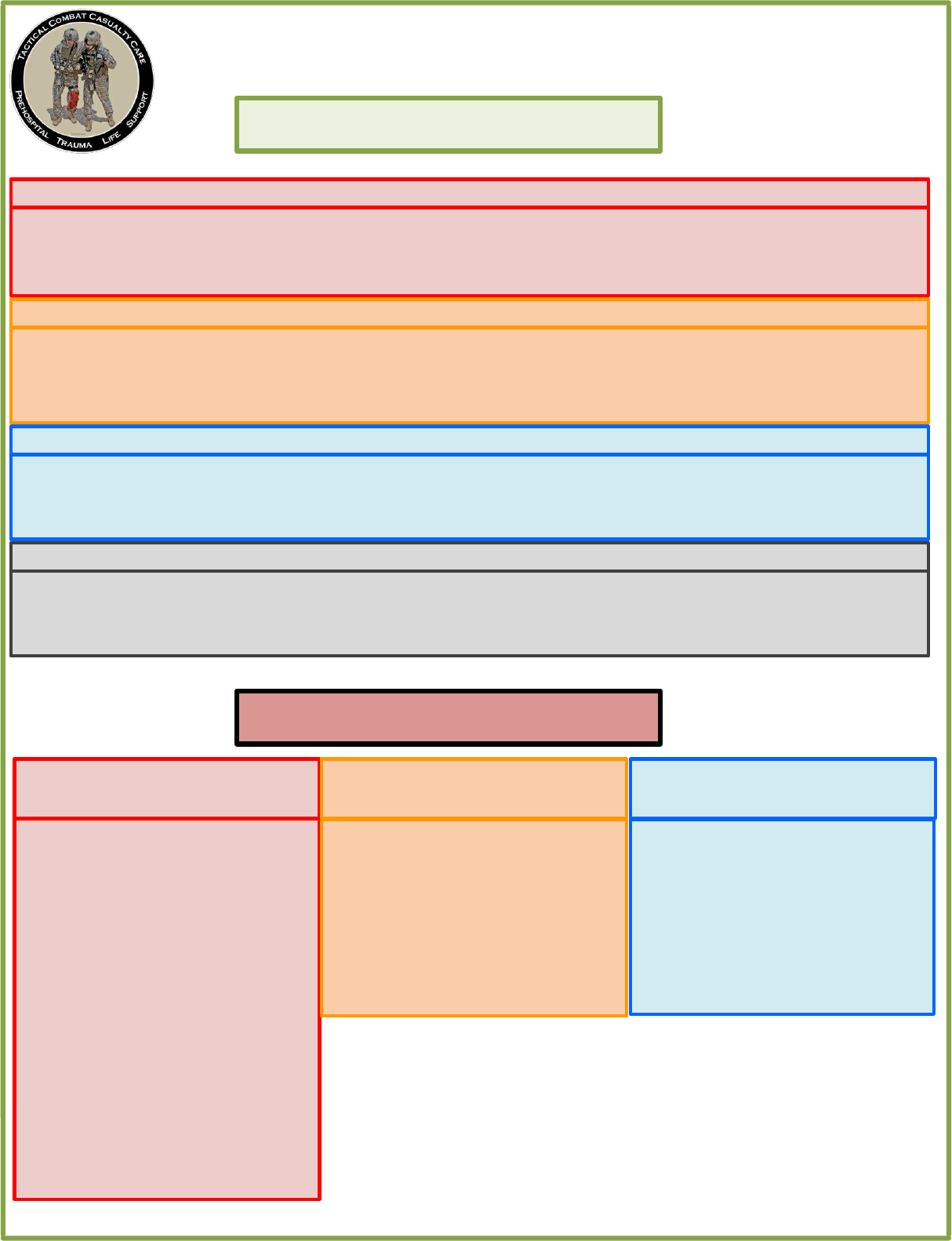
ABBREVIATED TCCC GUIDELINES…………………………………………………………………..PAGE 4
COTCCC RECOMMENDED ITEMS…………………………………………………………………..PAGE 40
DD1380 TCCC CARD………….…………………………………………………………………..PAGE 33
CASUALTY AAR SUBMISSION…...…………………………………………………………………..PAGE 37
TRIAGE & EVACUATION CATEGORIES……………………………………………………………..PAGE 34
MEDEVAC REQUEST FORMAT..…………………………………………………………………..PAGE 35
PLANNING FOR CASUALTY RESPONSE..…………………………………………………………..PAGE 46
GLOSSARY……………………...…………………………………………………………………..PAGE 51
CONVERSIONS…………………..…………………………………………………………………..PAGE 52
DRUG QUICK REFERENCE……...…………………………………………………………………..PAGE 53
KEY REFERENCES & RECOMMENDED READING…………………………………………………..PAGE 47
CARE UNDER FIRE ALGORITHM………………………………...……………………………….…..PAGE 9
TACTICAL FIELD CARE ALGORITHMS………………………………………………………………..PAGE 10
TACTICAL EVACUATION CARE ALGORITHMS………………………………………………………..PAGE 21
TCCC PHARMACOLOGY...……...…………………………………………………………………..PAGE 41
Massive Hemorrhage
11
Airway Management
12
Respiration/Breathing
13
C
- Bleeding
13
C
- IV Access
14
C
- TXA
14
C
- Fluid Resuscitation
15
Hypothermia Prev
16
Monitoring
16
Pain Management
17
Antibiotics
17
Wounds
18
Burns
18
Splints
18
Communications
19
CPR
19
Documentation
19
Prep for Evacuation
20
Transition of Care
21
Massive Hemorrhage
22
Airway Management
23
Respiration/Breathing
24
C
- Bleeding
25
C
- IV Access
26
C
- TXA
26
C
- Fluid Resuscitation
27
Trauma Brain Injury
28
Hypothermia Prev
29
Eye Trauma
29
Monitoring
29
Pain Management
30
Antibiotics
30
Wounds
31
Burns
31
Splints
31
Communications
32
CPR
32
Documentation
32

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
FORWARD
Tactical Combat Casualty Care (TCCC) has saved hundreds of lives during our nation's conflicts in Iraq and
Afghanistan. Nearly 90% of combat fatalities occur before the casualty reaches a Medical treatment facility, it
is clear that the prehospital phase of care is the focus of efforts to reduce deaths in combat. Very few military
physicians, however, have had training in this area. As a result, at the onset of hostilities, most combat
Medics, corpsmen, and para-rescue personnel (PJs) in the US Military were trained to perform battlefield
trauma care through the use of civilian-based trauma courses that were not designed for the prehospital
combat environment and did not reflect contemporary knowledge in this area.
This challenge was met by the Committee on TCCC (CoTCCC) voting members and its many liaison members
that collectively comprise the TCCC Working Group. This remarkably eclectic group includes trauma surgeons,
emergency medicine physicians, internists, family medicine physicians, operational physicians and physician
assistants, combat medical educators, trauma researchers, pathologists, combat medical doctrine developers,
medical equipment specialists, and combat medics, corpsmen, and PJs. All of the US Armed Services are well-
represented in the group's membership and 100% of the CoTCCC voting members have been to war. The
CoTCCC and the TCCC Working Group represents different services, disciplines, and military experiences, all
brought to bear on a single goal - reducing preventable deaths on the battlefield.
No such group existed when the Twin Towers fell. The US Special Operations Command initially funded the
group as a research effort, then ownership of the group was successively assumed by the Naval Operational
Medicine Institute, the Defense Health Board, and now the Joint Trau-ma System.
This group has taken the TCCC Guidelines as they existed in 2001 and continually updated them throughout
the 15 years of war, based on input from the Joint Trauma System Performance Improvement trauma
teleconferences, published case reports and case series from the war zones, breakthroughs in military Medical
research, and new publications from the civilian medical literature that bear on combat trauma. It has
processed a continual steam of input from the battlefield throughout the war years and ensured that
battlefield trauma care lessons learned were not just noted, but acted upon.
Through the ongoing volunteer efforts of this dedicated group of individuals - which met quarterly throughout
most of the war - US Forces have had prehospital trauma care guidelines that were customized for the
battlefield and updated continuously based on real-time evaluation of outcomes from ongoing combat
operations. This is the first time in our nation's history that this has occurred.
The success of TCCC effort had been well documented. It is a great tribute to all of the members of the CoTCCC
and the TCCC Working Group, that it has been able to transcend service and Medical specialty differences,
process new information expertly, and develop evidence-based, best-practice guidelines that have completely
transformed battlefield trauma care..
It is to the Committee on TCCC and all of our valued colleagues in the TCCC Working Group that this TCCC text
is dedicated. Our country and its casualties owe you all a profound measure of thanks.
Frank Butler, MD
CAPT (Retired), MC, USN
Chairman, Committee on Tactical Combat Casualty Care

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABBREVIATED TCCC GUIDELINES
31 JAN 2017
Return Fire and take cover
Direct or expect casualty to remain engaged as a combatant if appropriate
Direct casualty to move to cover and apply self-aid if able.
Try to keep the casualty from sustaining additional wounds.
Stop life-threatening external hemorrhage if tactically feasible:
- Direct casualty to control hemorrhage by self-aid if able.
Use a CoTCCC-recommended limb tourniquet for extremity hemorrhage
- Move the casualty to cover
Airway management is generally best deferred until the Tactical Field Care phase.
Basic Management Plan for Care Under Fire
Basic Management Plan for Tactical Field Care
Establish Security Perimeter IAW Tactical SOPs. Maintain situational awareness.
Triage Casualties as required. Altered mental status is criteria to have weapons cleared/secured, communications gear
secured and sensitive items redistributed.
Massive Hemorrhage
Assess for unrecognized hemorrhage and control all life-threatening bleeding.
Use one or more CoTCCC-recommended limb tourniquets if necessary.
Use a CoTCCC approved hemostatic dressing for compressible hemorrhage not amenable to limb tourniquet
use.
Immediately apply a CoTCCC-recommended junctional tourniquet if the bleeding site is amenable to use of a
junctional tourniquet.
Airway Management
Unconscious casualty without airway obstruction:
-Chin lift or jaw thrust maneuver
-Nasopharyngeal airway
-Place the casualty in the recovery position
Casualty with airway obstruction or impending airway obstruction:
-Allow a conscious casualty to assume any position that best protects the airway, to include sitting up
-Chin lift or jaw thrust maneuver
-Nasopharyngeal airway
-Place an unconscious casualty in the recovery position
If the previous measures are unsuccessful perform a surgical cricothyroidotomy using one of the following:
-CricKey technique
-Bougie-aided open surgical technique
-Standard open surgical technique
*Use lidocaine if the casualty is conscious
4

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABBREVIATED TCCC GUIDELINES
31 JAN 2017
Basic Management Plan for Tactical Field Care continued
Circulation - IV/IO Access
Start an 18-gauge IV or Saline Lock if indicated.
If IV access is not obtainable, use an intraosseous (IO) needle.
Circulation - Bleeding
Apply a pelvic binder for suspected pelvic fracture and/or severe blunt force or blast injury.
Reassess prior tourniquet application:
-Expose the wound and determine if a tourniquet is needed; if bleeding is not controlled then tighten
tourniquet if possible.
-If the first tourniquet does not control bleeding after tightening, then add a second tourniquet side-by-
side with the first.
Convert Limb tourniquets and junctional tourniquets if the following three criteria are met:
-The casualty is not in shock.
-It is possible to monitor the wound closely for bleeding.
-The tourniquet is not being used to control bleeding from an amputation.
Convert tourniquets in less than 2 hours if bleeding can be controlled with other means.
Expose and use an indelible marker to clearly mark all tourniquet sites with the time of tourniquet application,
reapplication, conversion, or removal.
Respiration/Breathing
In a casualty with progressive respiratory distress and known or suspected torso trauma, consider a tension
pneumothorax:
-Decompress the chest on the side of the injury at the primary or alternate site.
All open and/or sucking chest wounds should be treated by:
-Applying a vented chest seal (preferred)
-Applying a non-vented chest seal
-Burp the wound if indicated for breathing difficulty
Initiate pulsoximetry monitoring.
Monitor for tension pneumothorax.
Casualties with moderate/severe TBI should be given supplemental oxygen when available to maintain an
oxygen saturation > 90%.
Circulation - TXA
If a casualty is anticipated to need a blood transfusion, then administer 1 gram of tranexamic acid (TXA) in
100ml of NS or LR over 10min ASAP but NOT beyond 3 hours post injury.
Circulation - Fluid Resuscitation
Assess for hemorrhagic shock:
-If not in shock PO fluids are permissible if casualty is conscious and can swallow.
-If in shock resuscitate with:
Whole blood (preferred) or
Plasma, RBCs and platelets (1:1:1) or
Plasma and RBCs (1:1) or
Plasma or if blood products not available,
Hextend or Lactated Ringers or Plasma-Lyte-A
Resuscitate with above fluids until a palpable radial pulse, improved mental status or
systolic BP of 80-90 mmHg is present. Discontinue fluids when one or more end points are achieved.
Reassess casualty frequently to check for recurrence of shock. If shock recurs, verify all hemorrhage is under
control and repeat fluid resuscitation as above.
5
TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABBREVIATED TCCC GUIDELINES
31 JAN 2017
Basic Management Plan for Tactical Field Care continued
Penetrating Eye Trauma - If penetrating eye injury is noted or suspected:
Perform a rapid field test of visual acuity and document findings.
Cover eye with a rigid eye shield (not a pressure patch).
Administer Combat Wound Medication Pack if possible and/or administer IV/IM antibiotics per below.
Burns
Facial burns should be aggressively monitored for airway status and potential inhalation injury.
Estimate total body surface area (TBSA) burned to nearest 10%.
Cover burned areas with dry, sterile dressings. For burns >20% TBSA, consider placing casualty immediately in
HPMK or other hypothermia prevention means.
Fluid Resuscitation (USAISR Rule of Ten):
-If burns >20% TBSA, initiate IV/IO fluids ASAP with Lactated Ringers, NS, or Hextend. If Hextend, then no
more than 1000ml followed by LR or NS as needed.
-Initial IV/IO fluid rate = %TBSA X 10ml/per hour for adults 40-80 kg (+100ml/hr for every 10kg above 80kg).
-If hemorrhagic shock is present then resuscitate IAW fluid resuscitation in Circulation section.
All TCCC interventions may be performed on or through burned skin.
Hypothermia Prevention
Minimize casualty environmental exposure and promote heat retention.
Keep personal protective gear on if feasible. Replace wet clothing if possible. Get casualty onto insulated
surface ASAP.
Use a hypothermia prevention kit with active rewarming.
If none above is available, then use dry blankets, poncho liners, or sleeping bags and keep the casualty warm
and dry.
Warm IV fluids are preferred.
Monitoring – Initiate advanced electronic monitoring of vital signs if available.
Analgesia/Pain Management
Analgesia on the battlefield should generally be achieved by one of three options:
Mild to Moderate Pain and/or Casualty can swallow and is still able to fight:
-Administer TCCC Combat Wound Medication Pack (CWMP)
Moderate to Severe Pain and casualty IS NOT in Shock
-Oral Transmucosal Fentanyl Citrate (OTFC) 800mcg
Moderate to Severe Pain and casualty is in hemorrhagic shock or respiratory distress
-Administer Ketamine 50mg IM or IN repeating q30min prn
OR
-Administer Ketamine 20mg Slow IV or IO repeating q20min prn
*Endpoint control of pain or development of nystagmus.
*Consider Ondansetron 4mg ODT/IV/IO/IM q8hours prn for nausea and vomiting.
Antibiotics
If able to take PO, then administer Moxifloxacin 400mg PO qDaily from CWPP.
If unable to take PO, administer Ertapenem 1 gram IV/IM qDaily.
Wounds
Inspect and dress known wounds.
Check for Additional Wounds.
6

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABBREVIATED TCCC GUIDELINES
31 JAN 2017
Basic Management Plan for Tactical Field Care continued
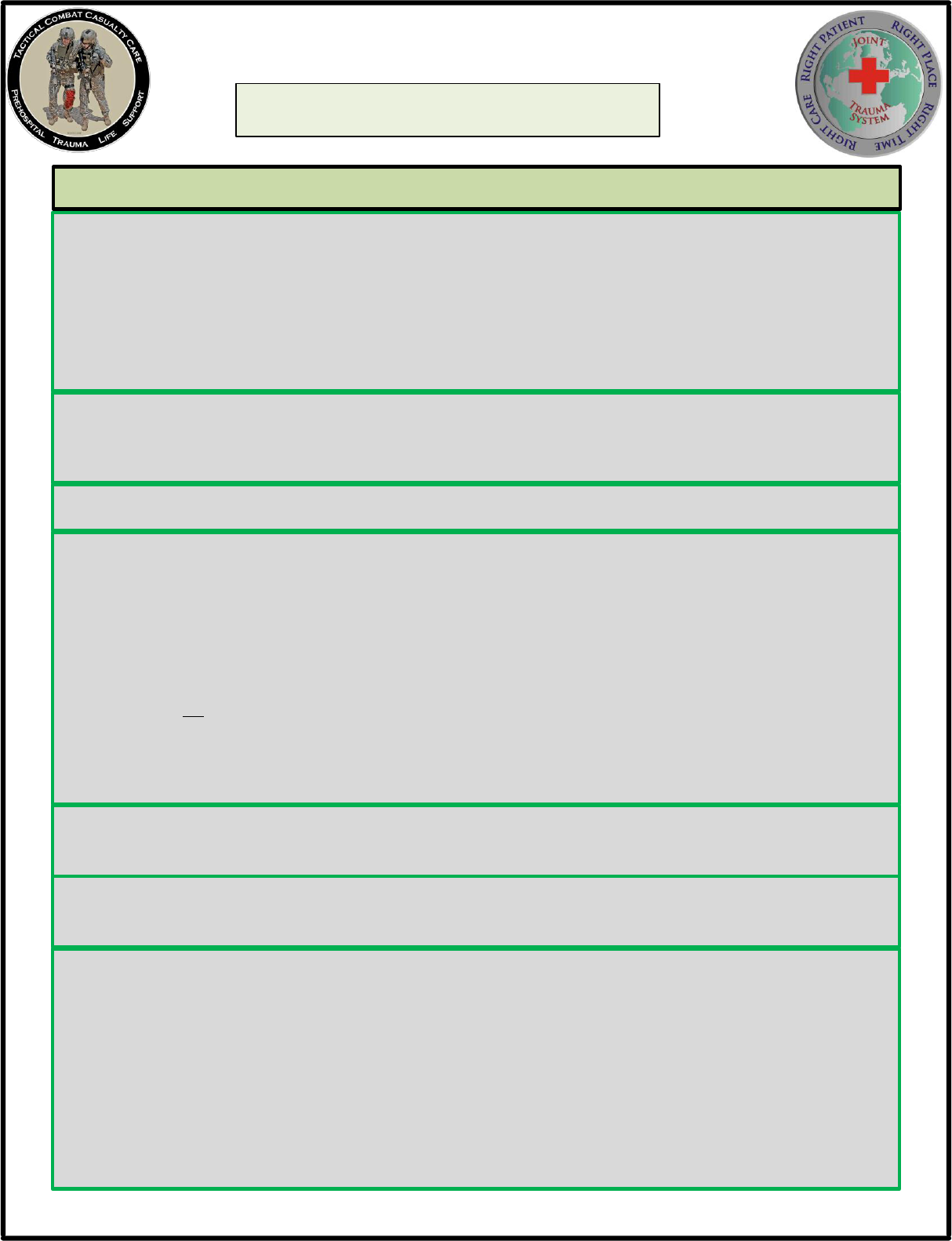
Documentation
Document clinical assessments, treatments rendered, and changes in the casualty's status on a TCCC Casualty Card (DD
Form 1380) and forward this information with the casualty to the next level of care.
Prepare for Evacuation
Complete and secure TCCC Card (DD1380) to casualty.
Secure all loose ends of bandages and wraps.
Secure hypothermia prevention wraps/blankets/straps.
Secure litter straps and consider additional padding for long evacuations.
Provide instructions to ambulatory patients as needed.
Stage Casualties for evacuation.
Maintain security at evacuation site.
Cardiopulmonary resuscitation (CPR)
Battlefield blast or penetrating trauma casualties with no pulse, no ventilations, and no other signs of life
should not be resuscitated.
Casualties with torso trauma or polytrauma with no pulse or respirations should have bilateral needle
decompression performed to confirm/deny tension pneumothorax prior to discontinuing care.
Splinting - Splint Fractures and Recheck Pulses.
Communication
Communicate with the casualty if possible. Encourage, reassure, and explain care.
Communicate with tactical leadership ASAP and throughout treatment. Provide casualty status and evac
requirements.
Communicate with the evacuation system to arrange TACEVAC.
Communicate with medical personnel on evacuation assets and relay mechanism of injury, injuries sustained,
signs/symptoms and treatments rendered.
7

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABBREVIATED TCCC GUIDELINES
31 JAN 2017
Transition of Care
Tactical force should establish evacuation point security and stage casualties for evacuation.
Tactical force personnel/medic should communicate patient status to TACEVAC personnel to include stable/
unstable, injuries identified, and treatments rendered.
TACEVAC personnel stage casualties on evac platform as required.
Secure casualties on evac platform IAW unit policies, platform configurations, and safety requirements.
TACEVAC medical personnel reassess casualties and re-evaluate all injuries and interventions.
Airway Management- Consider the following for casualty with airway obstruction or impending airway obstruction:
-Supraglottic airway, or
-Endotracheal intubation
In addition to the principles of Tactical Field Care consider the following for Tactical Evacuation Care:
Communication
Communicate with the casualty if possible. Encourage, reassure, and explain care
Communicate with next level of care and relay mechanism of injury, injuries sustained, signs/symptoms, and
treatments rendered.
Basic Management Plan for Tactical Evacuation Care (TACEVAC)
Breathing
Consider chest tube insertion if no improvement and/or long transport is anticipated.
Administer oxygen when possible for the following types of casualties:
-Low oxygen saturation by pulse oximetry
-Injuries associated with impaired oxygenation
-Unconscious casualty
-Casualty with TBI (maintain oxygen saturation > 90%)
-Casualty in shock
-Casualty at altitude
Traumatic Brain Injury-Casualties with moderate/severe TBI should be monitored for:
-Decreases in level of consciousness
-Pupillary dilation
-SBP should be >90 mmHg
-O2 sat > 90
-Hypothermia
-PCO2 (If capnography is available, maintain between 35-40 mmHg)
-Penetrating head trauma (if present, administer antibiotics)
-Assume a spinal (neck) injury until cleared
If impending herniation is suspected take the following actions:
-Administer 250 cc of 3 or 5% hypertonic saline bolus
-Elevate the casualty’s head 30 degrees
-Hyperventilate the casualty
8

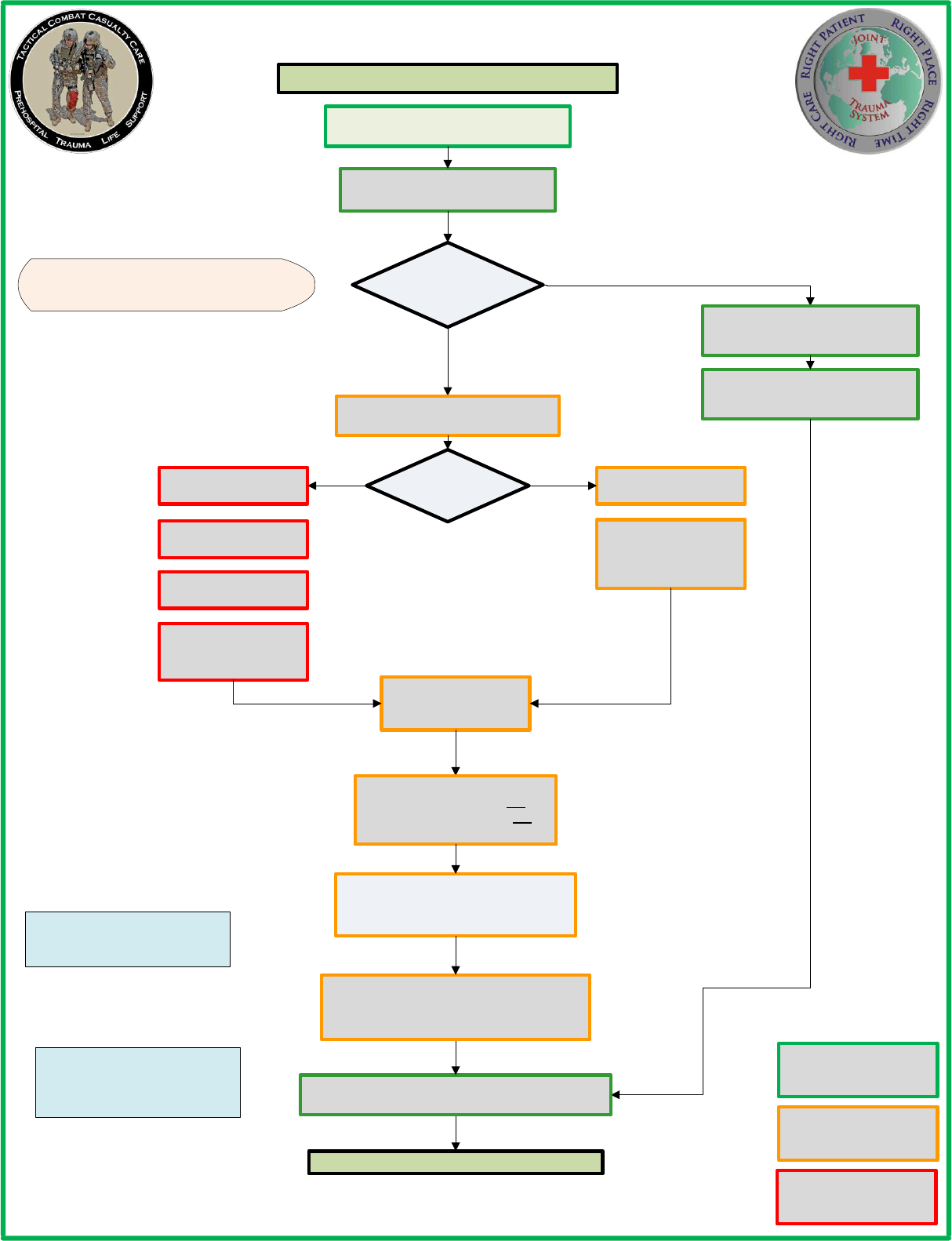
CARE UNDER FIRE
Return Fire and Take Cover
Casualty
Conscious?
Direct casualty
to move to
cover and
apply self-aid
Move casualty
to cover if
tactically
feasible
Casualty moved to cover
or extrication needed*
STOP LIFE
THREATENING
BLEEDING
Limb
Tourniquet
Indicated?
Use CoTCCC
Recommended Limb
Tourniquet applied
proximal to bleeding
site
Continue with Fight /
Mission
Move casualty to CCP or
secure area and initiate
Tactical Field Care
TACTICAL FIELD CARE
YES NO
YES
NO
LIFE THREATENING BLEEDING:
Spurting Blood or Flowing Blood
Blood soaking rapidly through uniform
or pooling on the ground
Complete Amputation
Try to keep casualty
from sustaining
additional wounds.
Try to keep casualty
from sustaining
additional wounds.
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Casualty
Sustained
Indicates Combat Medic
capability level skill
* Extrication
-Casualties should be extricated from
burning vehicles or buildings and moved
to relative safety. Do what is necessary
to stop burning process.
Casualty Movement:
- The fastest method is dragging along
the long axis of patient’s body by two
rescuers.
-Spinal precautions or stabilization should
only be considered after a casualty is
removed from the enemy threat and
indicated by mechanism of injury.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
Airway management is
generally best deferred until
the Tactical Field Care phase
TACTICAL COMBAT CASUALTY CARE
ALGORITHM
Place tourniquets “High &
Tight” if bleeding site is not
easily identifiable
9

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE
Establish Security Perimeter.
Maintain Situational Awareness.
Triage multiple casualties into
CCP or secure area as required
Casualties with altered mental status should have:
- Weapons cleared and secured
- Communications secured
- Sensitive missions items redistributed
Amenable to Limb
Tourniquet?
Tighten previously applied tourniquet or apply a
CoTCCC-recommended Limb Tourniquet. Apply a
2
nd
Tourniquet if bleeding not controlled.
Use CoTCCC-recommended
Hemostatic Dressing/Agent
Amenable to Junctional
Device?
Apply CoTCCC-recommended
Junctional Device
YES
YES
NO
NO
MASSIVE
HEMORRHAGE
Uncontrolled
Massive External
Hemorrhage or
Traumatic Amputation
Present?
YES
NO
Head Wounds
Neck Wounds
Junctional Wounds
Maintain Pressure with CoTCCC-
recommended Hemostatic Dressing/
Agent and Direct Pressure
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL FIELD CARE
Hemorrhage Controlled?
YES
NO
Hemorrhage
Controlled?
YES
NO
Assess minimal bleeding after airway
and breathing management
Triage as required.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
10

Airway Obstruction or
Impending Airway Obstruction
Unconscious without Airway
Obstruction
Chin Lift / Jaw Thrust Maneuver
Insert Nasopharyngeal Airway
Recovery Position
Previous Airway
Procedures Successful?
Perform Surgical
Cricothyroidotomy
CricKey Technique (preferred)
Bougie-assisted surgical technique
Standard open surgical technique
Assess Respiration /
Breathing
YES
NO
Assess Airway
Use lidocaine if
casualty is conscious.
TACTICAL COMBAT CASUALTY CARE
ALGORITHM
Conscious with NO
airway trauma or
problem identified
Chin Lift / Jaw Thrust Maneuver
Insert Nasopharyngeal Airway
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
If able, allow casualty to assume
any position that best protects the
airway, to include sitting up and
leaning forward.
TACTICAL FIELD CARE CONTINUED
AIRWAY
Spinal stabilization is not
necessary for casualties with
penetrating trauma.
OR
OR
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
11

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
Assess Respiration /
Breathing
Vented chest seals are
preferred over non-vented.
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
YES
NO
Decompression Needle
14-gauge, 3.25 inch needle/
catheter unit
Primary Site:
2
nd
Intercostal Space/
Midclavicular line
Alternate Site:
4
th
or 5
th
Intercostal Space /
Anterior Axillary Line
Burp or remove chest seal if applied.
Repeat as necessary.
If moderate or severe TBI is suspected, provide
supplemental O2 if available to maintain
SpO2>90%
MONITOR FOR TENSION
PNEUMOTHORAX
Initiate Pulse Oximetry
Monitoring if available
Needle Decompress Chest at
Primary or Alternate Site if indicated.
Repeat as necessary.
TENSION PNEUMOTHORAX INDICATORS:
Increasing Hypoxia
Respiratory Distress
Hypotension
Progressive Respiratory
Distress and Known or
Suspected Torso Trauma?
Suspect/Consider Tension
Pneumothorax
Needle Decompress Chest at Primary
or Alternate Site on injured side.
Repeat as necessary.
YES
NO
Open/Sucking
Chest Wound?
Apply Vented Chest Seal to all open/
sucking chest wounds
RESPIRATION / BREATHING
Tension Pneumothorax
Suspected?
YES
NO
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
12

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
Bleeding Assessment
Place second tourniquet 2-3 inches
above wound on skin.
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Reassess previously applied tourniquets.
NO
Leave previous tourniquet in place
Loosen first tourniquet once second
tourniquet is effectively placed
Bleeding Controlled?
Leave tourniquet in place – maximum 2
hours of tourniquet time until
reassessment
YES
YES
Before 2 hours, reassess: if not in shock,
able to monitor the wound closely for
bleeding, and no amputation – control
bleeding with hemostatic and/or pressure
dressing. Do not remove if TQ in place
>6 hours.
Control bleeding with
hemostatic and/or pressure
dressing.
Move original tourniquet to position next
to second tourniquet directly on skin and
tighten both until bleeding stopped and
distal pulse not palpated
NO
Monitor wound closely
for bleeding
Tourniquet not needed criteria:
-Minor lacerations w/minimal
bleeding
-Surface Abrasions
-Bleeding controlled by pressure
dressing
Expose wound and
determine if tourniquet is
needed.
Note time of tourniquet
release on tourniquet and/or
casualty card
Loosen tourniquet in <2 hours if
bleeding can be controlled by
other means. Leave tourniquet
loosely on limb for rapid
reapplication if needed. Do not
remove if TQ in place >6 hours.
Note time of tourniquet
reapplication on tourniquet
and/or casualty card
Each hemostatic works differently. If one
fails to control bleeding, it may be
removed and a fresh dressing of the same
type or a different type applied (Xstat
cannot be removed in the field)
CIRCULATION
(BLEEDING)
Pelvic Binder indicated?
NO
YES
Apply a Pelvic Binder
Pelvic Binder Indications- Severe blunt trauma or
blast injury with one or more of the following:
-Pelvic pain
-Any major lower limb amputation/near amputation
-Physical exam suggestive of pelvic fracture
-Unconsciousness or Shock
Reassess previously applied hemostatic
dressings/agents
If needed, control bleeding
with hemostatic and/or
pressure dressing.
Note time of tourniquet
release on tourniquet and/or
casualty card
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
13

Initiate 18G IV or Saline Lock
If IV is not obtainable, use IO route
TXA Criteria:
-Presents with Hemorrhagic Shock
-One or more major amputations
-Penetrating torso trauma
-Evidence of severe bleeding
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Reassess frequently for presence of shock
After initial fluid resuscitation, administer
second dose of Tranexamic Acid (TXA) 1 gm
in 100 ml of NS or LR IV over 10 min
Do NOT administer 3 hours or more after injury
TXA Needed?
Administer 1 gm of Tranexamic Acid (TXA) in
100 ml of NS or LR IV over 10min
Administer as soon as possible after injury
Do NOT administer >3hours after injury
YES
NO
TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
CIRCULATION
(INTRAVENOUS ACCESS)
CIRCULATION
(TRANEXAMIC ACID)
IV access indicated?
IV/IO Indications:
-In hemorrhagic shock or at
significant risk of shock
-Casualty needs IV/IO
medications
YES
NO
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
14
Hemorrhagic shock
present?
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Shock Criteria:
-Altered Mental Status (in absence of TBI)
-Weak/Absent Radial Pulse
Fluid Resuscitation
(in preferred order/combinations)
Blood Products
Available?
Whole Blood Transfusion
Plasma, RBCs, Platelets
1:1:1
Plasma and RBCs 1:1
Plasma (reconstituted,
liquid, or thawed) or
RBCs
Hextend 500 ml bolus
Lactated Ringers 500 ml
OR Plasma-Lyte A
500 ml bolus
Re-assess after each
unit or 500 cc bolus
administered
Fluid resuscitation and hypothermia
prevention should be executed
simultaneously if possible
YES NO
PO fluids permissible if casualty is
conscious and can swallow
Reassess frequently for presence of shock
YES
NO
OR, if not available
After initial fluid resuscitation, administer
second dose of Tranexamic Acid (TXA) 1 gm
in 100 ml of NS or LR IV over 10 min
Do NOT administer 3 hours or more after injury
If altered mental status due to suspected
TBI and has weak/absent radial pulse,
then resuscitate to restore normal radial
pulse or Systolic BP >90mmHg
Continue fluid resuscitation until:
Palpable radial pulse OR
Improved mental status OR
Systolic BP of 80-90 mmHg
If not in shock, NO IV fluids are
immediately necessary
If shock recurs, check all
hemorrhage management
interventions for effectiveness.
Repeat fluid resuscitation.
TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
CIRCULATION
(SHOCK / FLUID RESUSCITATION)
Assess for Shock
OR, if not available
OR, if not available
OR, if not available
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
15

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
HYPOTHERMIA
PREVENTION
Minimize casualty environmental exposure / promote heat retention
Keep Personal Protection Equipment (PPE) on if feasible and warranted
Replace wet clothes if possible
Use CoTCCC recommended hypothermia prevention equipment if available
Use dry blankets, poncho liner or sleeping bag. Keep casualty dry.
Warm IV fluids are preferred if possible
Hypothermia prevention and fluid
resuscitation should be executed
simultaneously if possible
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Penetrating Eye Trauma
noted or suspected?
Perform rapid field test of visual
acuity and document
Cover eye with Rigid Eye Shield
(DO NOT use pressure patch)
Ensure administration of
Moxfloxacin 400 mg from Combat
Wound Medication Pack
YES
NO
PENETRATING EYE
TRAUMA
Patient Monitoring
Patient monitoring should be
initiated as early as possible
Pulse oximetry should be utilized as a minimum adjunct to clinical
monitoring as stated in Breathing/Respiration section.
Advanced non-invasive electronic monitoring and recording of vital
signs should be initiated if possible and available.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
16

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
CONTINUE TACTICAL FIELD CARE
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Ensure Nalaxone (Narcan)
available if administering
opioid analgesics.
Administer 0.4 – 2 mg q 2-3
min PRN
Mild to Moderate Pain
(Casualty still able to fight)
Moderate to Severe Pain
Administer Combat Wound Medication Pack
Tylenol 650 mg bilayer caplet, 2 PO q8h
Meloxicam 15 mg PO qd
Disarm casualty
Document Mental Status
Is casualty in Shock or
Respiratory Distress or at
significant risk of developing
either?
Administer Oral Transmucosal Fentanyl Citrate
(OTFC) 800 ug
YES
NO
Reassess all pain management actions and
casualty reactions
END POINT:
Control of pain or Nystagmus development
OR
Monitor Airway-Breathing-Circulation
closely. Be prepared to provide
ventilatory assistance.
Consider Ondansetron 4 mg ODT/IV/IO/
IM q8h
PRN for nausea/vomiting
Add a second OTFC 800 ug
in 15 min if needed
Administer Ketamine
50 mg IM or IN
Repeat q30 min PRN
Administer Ketamine
20 mg slow IV or IO
Repeat q20 min PRN
Casualties with
moderate to
severe pain are
likely not able to
fight.
PAIN MANAGEMENT / ANALGESIA
Assess Pain
YES
NO
PO Able?
Moxifloxacin 400 mg PO qd
(CWMP)
Ertapenem 1 gm IV/IM qd
Early administration of
antiobiotics is
recommended for ALL
open combat wounds
ANTIBIOTICS
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
17

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
YES
NO
Burns?
Cover burned areas with dry sterile
dressing
Consider placing casualty in hypothermia
management equipment to cover/protect
wounds and prevent hypothermia
Facial / Neck
Burns?
Aggressively monitor airway status and
O2 saturations
Consider early surgical airway for respiratory
distress or O2 desaturation
Estimate TBSA to nearest 10% using
Rule of Nines
YES
NO
All TCCC interventions may be performed
on/through burned skin.
Burns >20%?
Initiate Fluid Resuscitation using USAISR Rule
of 10 using LR, NS or Hextend
USAISR Rule of 10 Fluid Calculation:
%TBSA X 10 ml/hour for adults 40-80 kg
(for every 10 kg above 80 kg, increase rate by
100 ml/hour
Hemorrhagic shock fluid management
takes precedence over burn fluid
resuscitation
YES
NO
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Do not exceed 1000 ml of
Hextend for burn resuscitation,
but can be followed by LR or NS.
INSPECT & DRESS KNOWN WOUNDS
CHECK FOR ADDITIONAL WOUNDS
Dress wounds to ensure hemorrhage control
and wound protection
BURNS
CONTINUE TACTICAL FIELD CARE
SPLINT FRACTURES
Splint Fractures and re-check pulses
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
18

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
Cardiopulmonary Resuscitation
(CPR)
Considerations
Battlefield blast or penetrating trauma
casualties with NO pulse, NO ventilations,
and NO other signs of life should not be
resuscitated.
However, casualties with torso or
polytrauma with no pulse or respirations
should have bilateral needle
decompression performed to confirm/
deny tension pneumothorax prior to
discontinuing care.
TACTICAL FIELD CARE CONTINUED
Communicate with
Casualty
Encourage, reassure, explain
care if possible
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
COMMUNICATION
Communicate with casualty, tactical leadership, and
medical providers in evacuation chain
Communicate with
Tactical Leadership
Provide casualty status and
evacuation requirements to
assist in evac coordination
Communicate with
Evacuation Chain
Communicate with medical
providers on evac asset if
possible.
Communicate with evacuation
system (PECC) to arrange
TACEVAC
Relay mechanism of injury,
injuries sustained, signs/
symptoms, and treatments
rendered.
Document clinical assessments, treatments rendered,
and changes on DD1380 TCCC Card and forward with
casualty to next level of care.
CONTINUE TACTICAL FIELD CARE
DOCUMENTATION
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
19

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL FIELD CARE CONTINUED
Complete & Secure TCCC
casualty card to each casualty
Secure all loose ends of bandages and wraps
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Transition of Care / Casualty Handover:
-Identify receiving care provider on evac platform
-Establish direct contact with receiving provider
(Radio Comms/Eye Contact/Hand Contact)
-Provide a SIT Status on each casualty beginning
with most serious
Stable or Unstable
Injuries (Life threats & MOI)
Treatments (Drugs & Interventions)
PREPARE FOR EVACUATION
Package Casualty for
Evacuation
Secure hypothermia prevention wraps/blankets/
straps
Secure litter straps as required
Consider additional padding for long evacuations
Provide instructions to ambulatory patients as
requried
Stage Casualties for
Evacuation
Stage casualties for evacuation IAW unit SOP
Maintain security at evac point IAW unit SOP
TACTICAL EVACUATION CARE
(TACEVAC)
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
20

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
Secure Casualties in Evacuation Platform IAW unit
policies, configuration and safety requirements
Refer to appropriate manuals for
specifics and procedures for
Helicopter Landing Zones (HLZ),
Ambulance Exchange Point (AXP),
Maritime Evacuation Point (MEP) or
as dictated by unit mission.
Re-Assess casualties and re-evaluate all injuries and
previous interventions
Triage and stage casualties on evacuation platform
as required
TRANSITION OF CARE
Tactical Force
Establish evacuation point security and stage casualties
for evacuation
Communicate patient information and status to
TACEVAC personnel as clearly as possible.
TACEVAC Personnel
Minimum information communicated:
-Stable or unstable
-Injuries identified
-Treatments rendered
Method of SIT Report:
-Identify receiving care provider on evac
platform
-Establish direct contact with receiving
provider
(Radio Comms/Eye Contact/Hand Contact*)
-Provide a SIT Status on each casualty
beginning with most serious
Stable or Unstable
Injuries (Life threats & MOI)
Treatments (Drugs & Interventions)
*if verbal communication is difficult, point to
each injury and treatment and confirm
acknowledgement.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
21
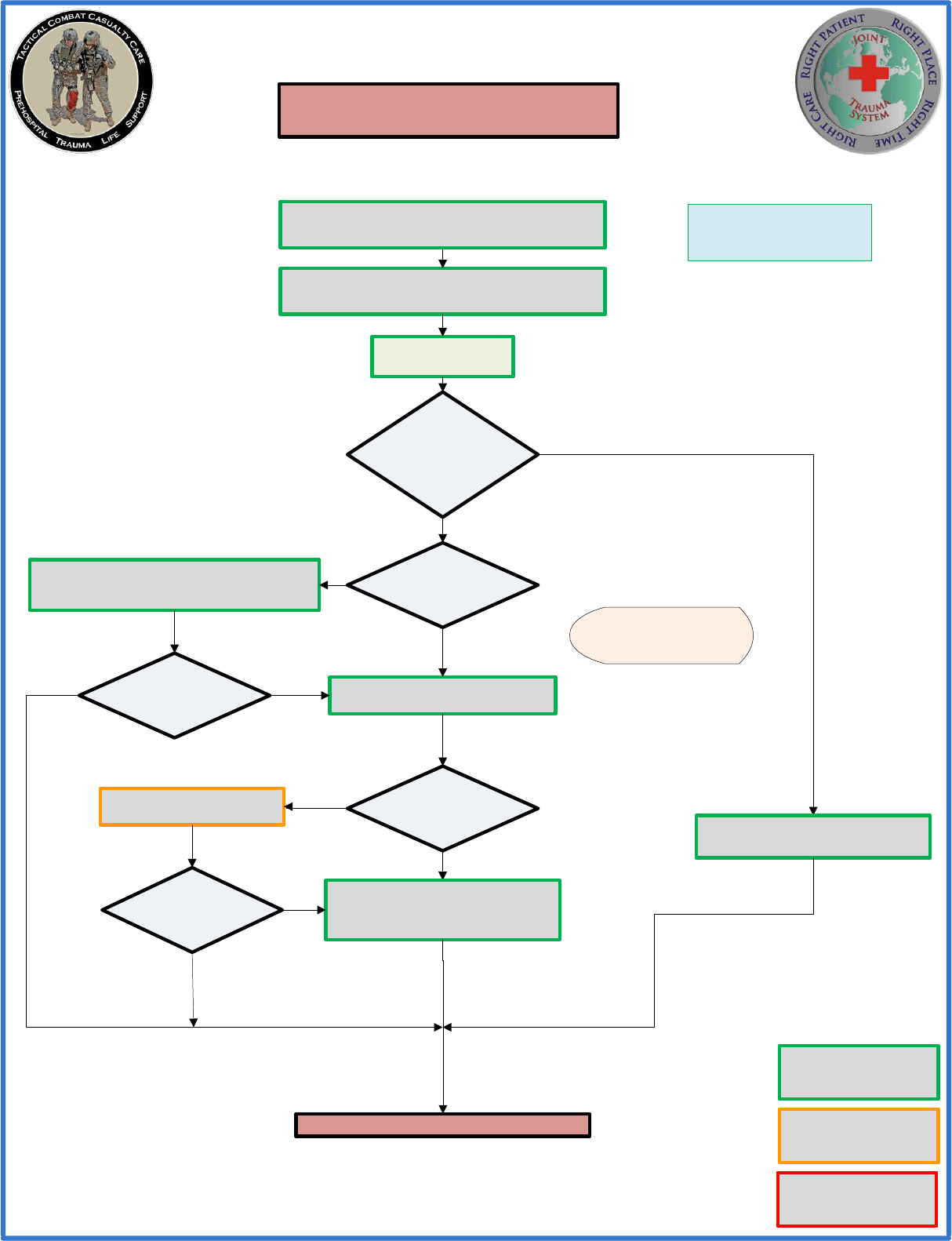
TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
Triage multiple casualties onto
evacuation platform as required
Casualties with altered mental status should should have
weapons and radios taken away
Amenable to Limb
Tourniquet?
Tighten previously applied tourniquet or apply a
CoTCCC-recommended Limb Tourniquet. Apply a
2
nd
Tourniquet if bleeding not controlled.
Use CoTCCC-recommended
Hemostatic Dressing/Agent
Amenable to Junctional
Device?
Apply CoTCCC-recommended
Junctional Device
YES
YES
NO
NO
MASSIVE
HEMORRHAGE
Uncontrolled
Massive External
Hemorrhage or
Traumatic Amputation
Present?
YES
NO
Head Wounds
Neck Wounds
Junctional Wounds
Maintain Pressure with CoTCCC-
recommended Hemostatic Dressing/
Agent and Direct Pressure
Hemorrhage Controlled?
YES
NO
Hemorrhage
Controlled?
YES
NO
Assess minimal bleeding after airway
and breathing management
Re-Assess casualties and re-evaluate all injuries and
previous interventions
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
22

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
Airway Obstruction or
Impending Airway Obstruction
Unconscious without Airway
Obstruction
Chin Lift / Jaw Thrust Maneuver
Insert Nasopharyngeal Airway
Recovery Position
Previous Airway
Procedures Successful?
CricKey Technique (preferred)
Bougie-assisted surgical technique or
Standard open surgical technique
Assess Respiration /
Breathing
YES
NO
Assess Airway
Use lidocaine if
casualty is conscious.
Conscious with NO
airway trauma or
problem identified
Chin Lift / Jaw Thrust Maneuver
Insert Nasopharyngeal Airway
If able, allow casualty to assume
any position that best protects the
airway, to include sitting up and
leaning forward.
Perform Surgical
Cricothyroidotomy
Supraglottic Airway
Endotracheal Intubation
OR
OR
Spinal stabilization is not
necessary for casualties with
penetrating trauma.
AIRWAY
OR
OR
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
23

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Assess Respiration /
Breathing
Vented chest seals are
preferred over non-vented.
YES
NO
Decompression Needle
14-gauge, 3.25 inch needle/
catheter unit
Primary Site:
2
nd
Intercostal Space/
Midclavicular line
Alternate Site:
4
th
or 5
th
Intercostal Space /
Anterior Axillary Line
Burp or remove chest seal if applied.
Repeat as necessary.
MONITOR FOR TENSION
PNEUMOTHORAX
Initiate Pulse Oximetry
Monitoring if not previously
done
Needle Decompress Chest at
Primary or Alternate Site if indicated.
Repeat as necessary.
TENSION PNEUMOTHORAX INDICATORS:
Increasing Hypoxia
Respiratory Distress
Hypotension
Progressive Respiratory
Distress and Known or
Suspected Torso Trauma?
Suspect/Consider Tension
Pneumothorax
Needle Decompress Chest at Primary
or Alternate Site on injured side.
Repeat as necessary.
YES
NO
Open/Sucking
Chest Wound?
Apply Vented Chest Seal to all open/
sucking chest wounds
Administer Oxygen when possible as indicated:
-Low oxygen saturation by pulsoximetry
-Injuries associated with impaired oxygenation
-Unconscious casualty
-Casualty in shock
-Casualty at altitude
-Known or suspected smoke inhalation
If moderate or severe TBI is suspected,
provide supplemental O2 if available to
maintain SpO2>90%
Consider chest tube insertion if no
improvement and/or long transport anticipated
CONTINUE TACTICAL EVACUATION CARE
RESPIRATION /
BREATHING
Tension Pneumothorax
Suspected?
YES
NO
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
24

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
Place second tourniquet 2-3 inches
above wound on skin.
NO
Leave previous tourniquet in place
Loosen first tourniquet once second
tourniquet is effectively placed
Bleeding Controlled?
YES
YES
Control bleeding with
hemostatic and/or pressure
dressing.
Move original tourniquet to position next
to second tourniquet directly on skin and
tighten both until bleeding stopped and
distal pulse not palpated
NO
Monitor wounds
closely for bleeding
Tourniquet not needed criteria:
-Minor lacerations w/minimal
bleeding
-Surface Abrasions
-Bleeding controlled by pressure
dressing
Expose wound and
determine if tourniquet is
needed.
Note time of tourniquet
release on tourniquet and/or
casualty card
Loosen tourniquet in <2 hours if
bleeding can be controlled by
other means. Leave tourniquet
loosely on limb for rapid
reapplication if needed. Do not
remove if TQ in place >6 hours.
Note time of tourniquet
reapplication on tourniquet
and/or casualty card
Reassess previously applied hemostatic
dressings/agents
Each hemostatic works differently. If one
fails to control bleeding, it may be
removed and a fresh dressing of the same
type or a different type applied (Xstat
cannot be removed in the field)
Bleeding Assessment
CIRCULATION
(BLEEDING)
Pelvic Binder indicated?
NO
YES
Apply a Pelvic Binder
Pelvic Binder Indications- Severe blunt trauma or
blast injury with one or more of the following:
-Pelvic pain
-Any major lower limb amputation/near amputation
-Physical exam suggestive of pelvic fracture
-Unconsciousness or Shock
Reassess previously applied tourniquets.
Leave tourniquet in place – maximum 2
hours of tourniquet time until
reassessment
Before 2 hours, reassess: if not in shock,
able to monitor the wound closely for
bleeding, and no amputation – control
bleeding with hemostatic and/or pressure
dressing. Do not remove if TQ in place
>6 hours.
If needed, control bleeding
with hemostatic and/or
pressure dressing.
Note time of tourniquet
release on tourniquet and/or
casualty card
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
25

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
Initiate 18G IV or Saline Lock
If IV is not obtainable, use IO route
TXA Criteria:
-Presents with Hemorrhagic Shock
-One or more major amputations
-Penetrating torso trauma
-Evidence of severe bleeding
Reassess frequently for presence of shock
After initial fluid resuscitation, administer
second dose of Tranexamic Acid (TXA) 1 gm
in 100 ml of NS or LR IV over 10 min
Do NOT administer 3 hours or more after injury
TXA Needed?
Administer 1 gm of Tranexamic Acid (TXA) in
100 ml of NS or LR IV over 10min
Administer as soon as possible after injury
Do NOT administer >3hours after injury
YES
NO
CIRCULATION
(INTRAVENOUS ACCESS)
CIRCULATION
(TRANEXAMIC ACID)
IV access indicated?
IV/IO Indications:
-In hemorrhagic shock or at
significant risk of shock
-Casualty needs IV/IO
medications
YES
NO
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
26

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Hemorrhagic shock
present?
Shock Criteria:
-Altered Mental Status (in absence of TBI)
-Weak/Absent Radial Pulse
Fluid Resuscitation
(in preferred order/combinations)
Blood Products
Available?
Whole Blood Transfusion
Plasma, RBCs, Platelets
1:1:1
Plasma and RBCs 1:1
Plasma (reconstituted,
liquid, or thawed) or
RBCs
Hextend 500cc bolus
Lactated Ringers 500cc
OR Plasma-Lyte A
500cc bolus
Re-assess after each
unit or 500 cc bolus
administered
Fluid resuscitation and hypothermia
prevention should be executed
simultaneously if possible
YES NO
PO fluids permissible if casualty is
conscious and can swallow
Reassess frequently for presence of shock
YES
NO
OR, if not available
After initial fluid resuscitation, administer
second dose of Tranexamic Acid (TXA) 1 gram
in 100 cc of NS or LR IV over 10 min
Do NOT administer 3 hours or more after injury
If altered mental status due to suspected
TBI and has weak/absent peripheral
pulse, then resuscitate to restore normal
radial pulse or Systolic BP >90mmHg
Continue fluid resuscitation until:
Palpable radial pulse OR
Improved mental status OR
Systolic BP of 80-90 mmHg
If not in shock, NO IV fluids are
immediately necessary
If shock recurs, check all
hemorrhage management
interventions for effectiveness.
Repeat fluid resuscitation.
CONTINUE TACTICAL EVACUATION CARE
CIRCULATION
(SHOCK / FLUID RESUSCITATION)
Assess for Shock
OR, if not available
OR, if not available
OR, if not available
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
27

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
-Administer 250 ml of 3% or 5% hypertonic
saline bolus
Assess for traumatic brain
injury (TBI)
Impending herniation
suspected?
-Elevate the casualty’s head 30 degrees
Initiate capnography if available to maintain
end-tidal CO2 between 30-35mmHg
-Hyperventilate the casualty at 20 breaths/min
with highest O2 concentration available
Monitored for:
-Decreased level of consciousness
-Pupillary dilation
-SBP should be >90 mmHg
-O2 sat>90
-Hypothermia
-PCO2 maintained between 35-40 mmHg
-Penetrating head trauma (administer antibiotics)
-Assume a spinal (neck) injury until cleared
Moderate/Severe TBI
suspected?
CONTINUE TACTICAL EVACUATION CARE
NO
YES
NO
YES
HERNIATION INDICATORS:
-Assymetric Pupils / Unilateral
pupillary dilation accompanied by
decreased level of consciousness.
-Fixed Dilated Pupil
-Extensor Posturing
-Widening Pulse Pressure
- DO NOT hyperventilate the casualty
unless signs of impending herniation
are present.
- Casualties may be hyperventilated
with O2 using the BVM.
TBI Indicators:
-Obvious mechanism of injury
-Loss of consciousness >30 min
-Confused of disoriented state
-Moderate TBI – GCS 9-13
-Severe TBI – GCS 3-8
TRAUMATIC BRAIN INJURY (TBI)
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
28

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
HYPOTHERMIA
PREVENTION
Minimize casualty environmental exposure / promote heat retention
Keep Personal Protection Equipment (PPE) on if feasible and warranted
Replace wet clothes if possible
Use CoTCCC recommended hypothermia prevention equipment if available
Use dry blankets, poncho liner or sleeping bag. Keep casualty dry.
Use portable fluid warmer to warm all IV fluids including blood.
Hypothermia prevention and fluid
resuscitation should be executed
simultaneously if possible
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Penetrating Eye Trauma
noted or suspected?
Perform rapid field test of visual
acuity and document
Cover eye with Rigid Eye Shield
(DO NOT use pressure patch)
Ensure administration of
Moxfloxacin 400 mg from Combat
Wound Medication Pack
YES
NO
PENETRATING EYE
TRAUMA
Patient Monitoring
Patient monitoring should be
initiated as early as possible
Pulse oximetry should be utilized as a minimum adjunct to clinical
monitoring as stated in Breathing/Respiration section.
Advanced non-invasive electronic monitoring and recording of vital
signs should be initiated if possible and available.
Protect the casualty from wind if doors/windows must be kept open.
CONTINUE TACTICAL EVACUATION CARE
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
29

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
Ensure Nalaxone (Narcan)
available if administering
opioid analgesics.
Administer 0.4 – 2 mg q 2-3
min PRN
Mild to Moderate Pain
(Casualty still able to fight)
Moderate to Severe Pain
Administer Combat Wound Medications Pack
Tylenol 650 mg bilayer caplet, 2 PO q8h
Meloxicam 15 mg PO qd
Disarm casualty
Document Mental Status
Is casualty in Shock or
Respiratory Distress or at
significant risk of developing
either?
Administer Oral Transmucosal Fentanyl Citrate
(OTFC) 800 ug
YES
NO
Reassess all pain management actions and
casualty reactions
END POINT:
Control of pain or Nystagmus development
OR
Monitor Airway-Breathing-Circulation
closely. Be prepared to provide
ventilatory assistance.
Consider Ondansetron 4 mg ODT/IV/IO/
IM q8h
PRN for nausea/vomiting
Add a second OTFC 800 ug
in 15 min if needed
Administer Ketamine
50 mg IM or IN
Repeat q30 min PRN
Administer Ketamine
20 mg slow IV or IO
Repeat q20 min PRN
PAIN MANAGEMENT / ANALGESIA
Assess Pain
YES
NO
PO Able?
Moxifloxacin 400 mg PO qd
(CWMP)
Ertapenem 1 gm IV/IM qd
Early administration of
antiobiotics is
recommended for ALL
open combat wounds
ANTIBIOTICS
TACTICAL EVACUATION CARE
(TACEVAC)
CONTINUE TACTICAL EVACUATION CARE
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
30

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
CONTINUE TACTICAL EVACUATION CARE
YES
NO
Burns?
Cover burned areas with dry sterile
dressing
Consider placing casualty in hypothermia
management equipment to cover/protect
wounds and prevent hypothermia
Facial / Neck
Burns?
Aggressively monitor airway status and
O2 saturations
Consider early surgical airway for respiratory
distress or O2 desaturation
Estimate TBSA to nearest 10% using
Rule of Nines
YES
NO
All TCCC interventions may be performed
on/through burned skin.
Burns >20%?
Initiate Fluid Resuscitation using USAISR Rule
of 10 using LR, NS or Hextend
USAISR Rule of 10 Fluid Calculation:
%TBSA X 10 ml/hour for adults 40-80 kg
(for every 10 kg above 80 kg, increase rate by
100 ml/hour
Hemorrhagic shock fluid management
takes precedence over burn fluid
resuscitation
YES
NO
Do not exceed 1000 ml of
Hextend for burn resuscitation,
but can be followed by LR or NS.
INSPECT & DRESS KNOWN WOUNDS
CHECK FOR ADDITIONAL WOUNDS
Dress wounds to ensure hemorrhage control
and wound protection
BURNS
SPLINT FRACTURES
Splint Fractures and re-check pulses
Extra emphasis should be placed
on hypothermia prevention and IV
warming for burn patients.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
31

TACTICAL COMBAT CASUALTY CARE
ALGORITHM
TACTICAL EVACUATION CARE
(TACEVAC)
Indicates Combat
Paramedic or SOF Medic
capability level skill
Indicates All Combatants
and Combat Lifesaver
capability level skill
Indicates Combat Medic
capability level skill
NEXT LEVEL CARE
Cardiopulmonary Resuscitation
(CPR)
Considerations
CPR may be attempted in TACEVAC if
casualty does not have obviously fatal
wounds and quickly arriving at a surgical
capability. CPR should not be attempted
if compromising the mission or denying
lifesaving treatment to other casualties.
Casualties with torso or polytrauma with
no pulse or respirations should have
bilateral needle decompression performed
to confirm/deny tension pneumothorax
prior to discontinuing care.
Communicate with
Casualty
Encourage, reassure, explain
care if possible
COMMUNICATION
Communicate with casualty and medical providers
in evacuation chain
Communicate with
Receiving Medical Facility
Communicate with medical
providers on evac asset if
possible.
Relay mechanism of injury,
injuries sustained, signs/
symptoms, and treatments
rendered.
Document clinical assessments, treatments rendered,
and changes on DD1380 TCCC Card and forward with
casualty to next level of care.
DOCUMENTATION
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
32

33
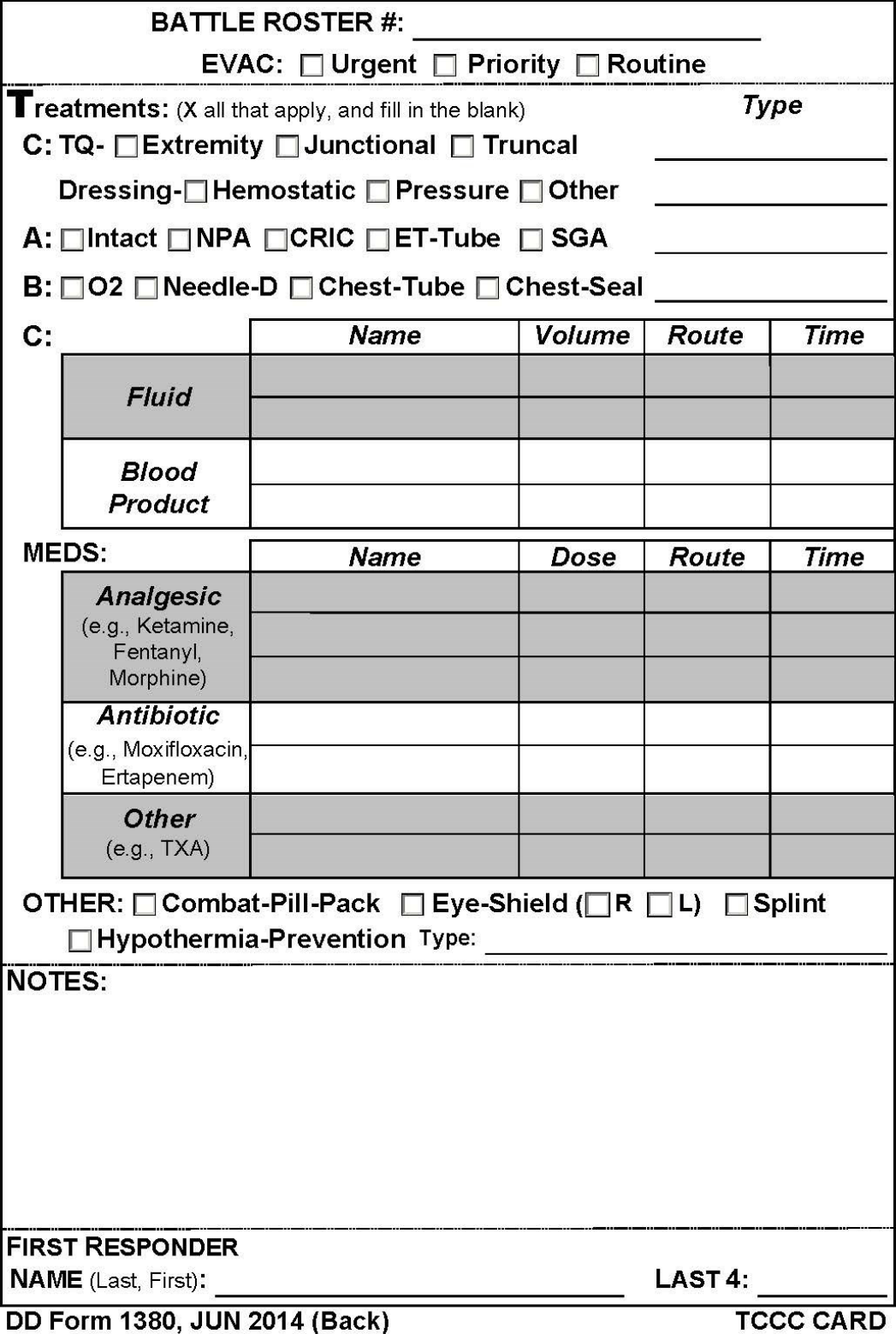
34
TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TRIAGE CATEGORIES
This category includes those casualties who require an immediate LSI and/or surgery. Put simply, if medical attention is not provided they will die.
The key to successful triage is to locate these individuals as quickly as possible. Casualties do not remain in this category for an extended
period of time. They are either found, triaged and treated, or they die! Hemodynamically unstable casualties with airway obstruction, chest or
abdominal injuries, massive external bleeding, or shock deserve this classification.
IMMEDIATE
This category includes those wounded who are likely to need surgery, but whose general condition permits delay in surgical treatment without
unduly endangering the life, limb, or eyesight of the casualty. Sustaining treatment will be required (e.g., oral or IV fluids, splinting,
administration of antibiotics and pain control), but can possibly wait. Examples of casualties in this category include those with no evidence of
shock who have; large soft tissue wounds, fractures of major bones, intra-abdominal and/or thoracic wounds, and burns to less than 20% of total
body surface area (TBSA).
DELAYED
Casualties in this category are often referred as the “walking wounded.” Although these patients may appear to be in bad shape at first, it is their
physiologic state that tells the true story. These casualties have minor injuries (e.g., small burns, lacerations, abrasions, or small fractures) that
can usually be treated with self- or buddy-aid. These casualties should be utilized for mission requirements (e.g., scene security), to help treat
and/or transport the more seriously wounded, or put back into the fight.
MINIMAL
Casualties in this category have wounds that are so extensive, that even if they were the sole casualty and had the benefit of optimal
medical resources, their survival would be highly unlikely. Even so, expectant casualties should not be neglected. They should receive
comfort measures and pain medication if possible, and they deserve re-triage as appropriate. Examples of expectant casualties are the
unresponsive with injuries such as penetrating head trauma with obvious massive damage to the brain.
EXPECTANT
EVACUATION PRECEDENCE
· Significant injuries from a dismounted
IED attack
· Gunshot wound or penetrating shrapnel to
chest, abdomen, or pelvis
· Any casualty with ongoing airway
difficulty
· Any casualty with ongoing respiratory
difficulty
· Unconscious casualty
· Casualty with known or suspected spinal
injury
· Casualty in shock
· Casualty with bleeding that is difficult to
control
· Moderate/Severe TBI
· Burns greater than 20% Total Body
Surface Area
URGENT / CATEGORY A
(WITHIN 2 HOURS) *
· Isolated, open extremity fracture with
bleeding controlled
· Any casualty with a tourniquet in place
· Penetrating or other serious eye injury
· Significant soft-tissue injury without
major bleeding
· Extremity injury with absent distal pulses
· Burns over 10-20% of Total Body Surface
Area
PRIORITY / CATEGORY B
(WITHIN 4 HOURS)
ROUTINE / CATEGORY C
(WITHIN 24 HOURS)
· Concussion (mild traumatic brain injury)
· Gunshot wound to extremity - bleeding
controlled without tourniquet
· Minor soft-tissue shrapnel injury
· Closed fracture with intact distal pulses
· Burns over < 10% Total Body Surface
Area
* Note that by Secretary of Defense directive, all casualties categorized as CAT A in the
Afghanistan theater of operations should be able to be evacuated to an MTF with a surgical
capability within 60 minutes from the time that the evacuation mission is approved.
34

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
MEDEVAC REQUEST
MEDEVAC REQUEST 9-LINE
LINE 1: LOCATION OF UNIT
LINE 2: CALLSIGN AND
FREQUENCY AT THE PZ
LINE 3: NUMBER AND
PRECEDENCE OF CASUALTIES
LINE 4: SPECIAL EQUIPMENT
REQUIRED
LINE 5: NUMBER OF
CASUALTIES BY TYPE
LINE 6: SECURITY AT PZ
LINE 7: PZ MARKING
LINE 8: CASUALTIES BY
NATIONALITY/STATUS
LINE 9: PZ TERRAIN/OBSTACLES
(CBRN CONTAMINATION IF APPLICABLE)
HLZ GRID (MGRS):
CALLSIGN:
FREQUENCY:
A: Number of Urgent Casualties
B: Number of Priority Casualties
C: Number of Routine Casualties
A: None
B: Hoist
C: Extraction
D: Ventilator
E: Other (specify)
L: Number of Litter Casualties
A: Number of Ambulatory Casualties
E: Number of Escorts
N: No enemy
P: Possible enemy
E: Enemy in area
X: Armed escort required
A: Panels
B: Pyrotechnics
C: Smoke (designate color)
D: None
E: Other (specify)
A: US/Coalition Military
B: US/Coalition Civilian
C: Non-Coalition
D: Non-Coalition Civilian
E: Opposing Forces/Detainee
F: Child
Brief description of significant obstacles on approach /
departure headings and type of predominant terrain for the
HLZ
In accordance with and excerpted from
Army Training Publication (ATP) 4-02.2
(Medical Evacuation)
35

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
MIST REPORT FORMAT
M – MECHANISM OF INJURY AND TIME OF INJURY (IF
KNOWN)
I – INJURY OR ILLNESS
S – SYMPTOMS AND VITAL SIGNS
T – TREATMENT GIVEN
MIST REPORT
Mechanism of Injury and time of injury (if known)
Injury or Illness
A – Airway status
B – Breathing rate
C – Pulse rate
D – Conscious/Unconscious
E – Other signs
Such as Tourniquet/Time Applied
Drugs administered
36

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
POINT-OF-INJURY / TCCC AFTER ACTION REPORT
The POI/TCCC AAR can be found electronically at:
www.cotccc.com
or
www.usaisr.amedd.army.mil/pdfs/POI_TCCC_AAR_26Apr2013.pdf
or
atn.army.mil.
The TCCC AAR is to be completed within 72 hours of the injury
occurring, by the POI Medical team or Role I, and sent to the DoD
Trauma Registry (DoDTR).
E-mail To:
The DoDTR is the data repository for DoD trauma-related injuries. The goal of this registry is to document, in
electronic format, information about the demographics, injury-producing incident, diagnosis and treatment, and
outcome of injuries sustained by US/Non-US military and US/ Non-US civilian personnel in wartime and peacetime
from the point of wounding to final disposition. The JTS collects data from TCCC cards (DD Form 1380, TCCC AARs
and from the Armed Forces Medical Examiner Services (AFMES). Documentation is vital to accumulate data in the
DoD Trauma registry, formerly the Joint Theater Trauma Registry (JTTR). The JTS functions as:
1. JTS Operations consisting of; Data Acquisition mines Medical records to abstract, code, and enter critical
trauma data into the DoDTR database. Data Analysis develops, queries, and provides data from the DoDTR in
response to requests for information and conducts classified and non-classified data analysis. Data Automation
supports the information technology for the DoDTR and data-related special projects.
2. Trauma Care Delivery maintains a database of operational and physiologic parameters related to
delivery of en route care and has evaluated the validity of the "Golden Hour" standard for movement of casualties
from point of injury to the first surgical capability. The addition of a military en route care registry (MERCuRY) will
capture all ground, air and ship transport care.
3. Performance Improvement (PI) coordinates improvement activities across the spectrum of trauma care
developing PI course content and training for combatant command trauma system development.
37

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
POINT-OF-INJURY / TCCC AFTER ACTION REPORT
38

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
POINT-OF-INJURY / TCCC AFTER ACTION REPORT
39

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
COTCCC RECOMMENDED DEVICES & ADJUNCTS
TOURNIQUETS
Common Name / Brand Name DLA Nomenclature NSN
Combat Application Tourniquet (CAT) Tourniquet, Nonpneumatic 6515-01-521-7976
SOF-Tactical Tourniquet (SOFTT) Tourniquet, Nonpneumatic One-Hand w Handles 6515-01-530-7015
Emergency Medical Tourniquet (EMT) Tourniquet, Pneumatic Single-hand application 6515-01-580-1645
HEMOSTATIC DRESSINGS/DEVICES
Common Name / Brand Name DLA Nomenclature NSN
Combat Gauze (CG) Z-Fold Bandage, Gauze Kaolin Impregnated 3X4" 6510-01-562-3325
Celox Gauze, Z-fold 5' Dressing, Hemostatic Celox Gauze 3"X5' folded 6510-01623-9910
ChitoGauze Dressing, Hemostatic 3X144" coated with Chitosan 6510-01-591-7740
X-Stat, Single Applicator Applicator, Hemostatic Sponges and Dispenser 6510-01-644-7335
JUNCTIONAL TOURNIQUETS & DEVICES
Common Name / Brand Name DLA Nomenclature NSN
Combat-Ready Clamp (CRoC) Clamp, Tourniquet Expandable Aluminum 6515-01-589-9135
SAM Junctional Tourniquet (SAM-JT) Tourniquet Kit Junctional Compression 6515-01-618-7475
Junctional Emergency Treatment Tool (JETT) Tourniquet, Inguinal Hemorrhage Adjustable 6515-01-616-5841
AIRWAY MANAGEMENT DEVICES & ADJUNCTS
Common Name / Brand Name DLA Nomenclature NSN
Control Cric / CricKey Cricothyrotomy System 6515-01-640-6701
DLA – Defense Logistics Agency
DLA Nomenclature is the naming convention terminology used in DoD supply systems and
often differ from common, brand, or product names.
NSN – National Stock Number. A NSN is 13-digit code identifying all standardized material
supply items recognized by NATO countries and the DoD.
In accordance with
CoTCCC Guidelines
As Of: 31 JAN 2017
40

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
PHARMACOLOGY REFERENCE
ACETAMINOPHEN (TYLENOL)
Class: CNS agent – non-narcotic, analgesic, antipyretic
TCCC Indications: For mild to moderate pain management for a casualty that is still able to fight as a component of the Combat
Wound Medication Pack (CWMP)
DOSE: 325–650 mg PO q4–6h (max: 4 g/d)
Onset / Peak / Duration: Onset Varies / Peak 1-3 hours / Duration 3-4 hours
Administration Instructions: PO
Contraindications: Acetaminophen hypersensitivity; use with alcohol; pregnancy category B
Adverse/Side Effects: Negligible with recommended dose; rash; acute poisoning: anorexia, nausea, vomiting, dizziness, lethargy,
diaphoresis, chills, epigastric or abdominal pain, diarrhea; hepatotoxicity: elevation of liver function tests; hypoglycemia, hepatic
coma, acute renal failure; chronic ingestion: neutropenia, pancytopenia, leukopenia, thrombocytopenic purpura, renal damage
Interactions: Cholestyramine may decrease absorption; barbiturates, carbamazepine, phenytoin, rifampin, and excessive alcohol
use may increase potential for hepatotoxicity
Mission Impact: None to minimal mission impact
K-9 Dosage: DO NOT GIVE
ERTAPENEM (INVANZ)
Class: Antimicrobial – antibiotic, carbapenem, beta-lactam
TCCC Indications: Recommended for all open combat wounds if unable to take PO meds
DOSE: 1 gram IV/IM q24h
Administration Instructions: For IV reconstitute with 10mL NS; for IM 3.2mL 1.0% lidocaine without epinephrine
Contraindications: Carbapenem, beta-lactam, or amide-type local anesthetic (ie. Lidocaine) hypersensitivity; pregnancy cat B
Adverse/Side Effects: Injection site phlebitis or thrombosis; asthenia, fatigue, death, fever, leg pain, anxiety, altered mental status,
dizziness, headache, insomnia; chest pain, hypo- or hypertension, tachycardia, edema; abdominal pain, diarrhea, acid reflux,
constipation, dyspepsia, nausea, vomiting, increased LFTs; cough, dyspnea, pharyngitis, rales, rhonchi, respiratory distress;
erythema, pruritus, rash
Interactions: Probenecid decreases renal excretion
Mission Impact: GROUNDING medication for personnel on flight status
The TCCC pharmacology reference provides drug information as based on administration
based solely on the TCCC Guidelines. These references should not be used for the
administration of these medications for any environment outside of tactical combat casualty
care on the battlefield or in the combat/tactical setting.
41
TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
PHARMACOLOGY REFERENCE
KETAMINE (KETALAR)
Class: Nonbarbiturate anesthetic, Dissociative
TCCC Indications: For moderate to severe pain management for a casualty that IS in hemorrhagic shock or respiratory distress or
is at significant risk of developing either condition. Also a useful adjunct to reduce the amount of opioids required to manage pain.
DOSE: 50 mg IM or IN, Repeat doeses q30min prn IM or IN (max: 4 g/d)
OR
20 mg slow IV or IO, Repeat doses q20min prn IV or IO (max: 4g/d)
Onset / Duration: IM – Onset in 3-4 minutes / Duration 12-25 minutes IV – Onset in 30 seconds / Duration 5-10 minutes
Administration Instructions: Document AVPU prior to administration. IV Ketamine should be administered slowly over 1 minute.
End points: Control of pain or development of nystagmus (rhythmic bac-and-forth movement of eyes). Be prepared to suction as
Ketamine can increase secretions. Be prepared to provide ventilatory support with a BVM.
Contraindications: Head injury (may worsen severe TBI), Hypersensitivity to ketamine, Pregnancy Category B
Adverse/Side Effects: Hypertension, Respiratory Depression, Emergence Reactions (delirium, hallucinations, confusion),
Increased Intra-cranial pressure, Increased intra-ocular pressure
Interactions: Effects of ketamine are increased when combined with other analgesics or muscle relaxants
Mission Impact: Casualty weapons, communications and sensitive equipment should be secured. GROUNDING medication for
personnel on flight status.
K-9 Dosage: 100-150mg (3-5mg/kg) IV/IM (best given in conjunction with diazepam 7.5mg or medazolam 7.5mg for profound
sedation)
Class: CNS agent - potent narcotic (opiate) agonist
TCCC Indications: For moderate to severe pain management for a casualty that IS NOT in shock or respiratory distress and IS
NOT at significant risk of developing either condition.
DOSE: 800 mcg oral transmucossally, reassess in 15 min, add a second lozenge in other cheek as necessary.
Administration Instructions: Document AVPU prior to administration. Place lozenge between the cheek and gum; do not chew
lozenge. Recommend taping lozenge-on-a-stick to casualty’s finger as an added safety OR utilizing a safety pin and rubber band to
attach the lozenge (under tension) to the patient’s uniform or plate carrier. Monitor for respiratory depression. Administer Nalaxone
as reversal if needed. Be prepared to provide ventilatory support with a BVM.
Contraindications: MAOIs; myasthenia gravis; pregnancy category C
Adverse/Side Effects: Sedation, euphoria, dizziness, diaphoresis, delirium, convulsions; bradycardia, hypotension, circulatory
depression, cardiac arrest; miosis, blurred vision; nausea, vomiting, constipation, ileus; muscle and thoracic muscle rigidity; urinary
retention, rash; laryngospasm, bronchoconstriction, respiratory depression or arrest
Interactions: Alcohol and other CNS depressants potentiate effects; MAOIs may precipitate hypertensive crisis
Mission Impact: Casualty weapons, communications and sensitive equipment should be secured. GROUNDING medication for
personnel on flight status.
FENTANYL ORAL LOZENGE / ORAL TRANSMUCOSAL FENTANYL CITRATE (OTFC)
42

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
PHARMACOLOGY REFERENCE
MORPHINE SULFATE (MSO4)
Class: CNS agent – narcotic (opiate) agonist; analgesic
TCCC Indications: Alternative to OTFC moderate to severe pain management for a casualty for a casualty that IS NOT in shock or
respiratory distress and IS NOT at significant risk of developing either condition.
DOSE: 5 mg IV/IO, Reassess in 10 min, repeat dose every 10 min as necessary to control severe pain.
Onset / Peak / Duration: IV – Onset in 5-20 minutes / Peak in 20 minutes / Duration 4-5 hours
Administration Instructions: Document AVPU prior to administration. Monitor for respiratory depression. Administer Nalaxone as
reversal if needed. Be prepared to provide ventilatory support with a BVM.
Contraindications: Opiate hypersensitivity; increased ICP; seizures; acute alcoholism; acute bronchial asthma, chronic pulmonary
disease, severe respiratory depression; chemical-irritant induced pulmonary edema; BPH; diarrhea due to poisoning until toxic
material has been eliminated; undiagnosed acute abdominal conditions; following biliary tract surgery and surgical anastomosis;
pancreatitis; acute ulcerative colitis; severe liver or renal insufficiency; hypothyroidism; pregnancy category B
Adverse/Side Effects: Pruritus, rash, urticaria, edema, anaphylactoid reaction; sweating, skeletal muscle flaccidity; cold, clammy
skin, hypothermia; euphoria, insomnia, disorientation, visual disturbances, dysphoria, paradoxic CNS stimulation (restlessness,
tremor, delirium, insomnia), convulsions; decreased cough reflex, drowsiness, dizziness, deep sleep, coma; miosis; bradycardia,
palpitations, syncope; flushing of face, neck, and upper thorax; orthostatic hypotension, cardiac arrest; constipation, anorexia, dry
mouth, biliary colic, nausea, vomiting, elevated LFTs; urinary retention or urgency, dysuria, oliguria, reduced libido or potency;
severe respiratory depression or arrest; pulmonary edema
Interactions: CNS depressants, sedatives, barbiturates, alcohol, benzodiazepines, and TCAs potentiate CNS depressant effects;
MAOIs may precipitate hypertensive crisis; phenothiazines may antagonize analgesia; herbals (Kava-kava, valerian, St. John's wort)
may increase sedation.
Mission Impact: Casualty weapons, communications and sensitive equipment should be secured. GROUNDING medication for
personnel on flight status.
K-9 Dosage: 2-3mg IV OR 10-20mg IM/SQ. Nausea/emesis and defication common. Reverse with 1mg Nalaxone IV/IM/SQ.
MELOXICAM (MOBIC)
Class: NSAID; COX2 Inhibitor, anti-inflammatory, analgesic, antipyretic
TCCC Indications: For mild to moderate pain management for a casualty that is still able to fight as a component of the Combat
Wound Medication Pack (CWMP)
DOSE: 7.5–15 mg PO daily
Administration Instructions: PO
Contraindications: NSAID or salicylate hypersensitivity; rhinitis, urticaria, angioedema, asthma; severe renal or hepatic disease;
pregnancy category C (1
st
/2
nd
trimester) and category D (3
rd
trimester)
Adverse/Side Effects: Edema, flu-like syndrome, pain; abdominal pain, diarrhea, dyspepsia, flatulence, nausea, constipation,
ulceration, GI bleed; anemia; arthralgia; dizziness, headache, insomnia; pharyngitis, upper respiratory tract infection, cough; rash,
pruritus; urinary frequency, UTI
Interactions: May decrease effect of ACE inhibitors and diuretics; may increase lithium levels and toxicity; aspirin may increase GI
bleed risk; warfarin and herbals (feverfew, garlic, ginger, ginkgo) may increase bleeding.
Mission Impact: None to minimal mission impact
K-9 Dosage: DO NOT GIVE
43

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
PHARMACOLOGY REFERENCE
NALAXONE (NARCAN)
Class: CNS agent – narcotic (opiate) antagonist
TCCC Indications: For narcotic opiate overdose and reversal of effects, including respiratory depression, sedation, and
hypotension.
DOSE: 0.4–2.0 mg IV, repeat q2–3min up to 10 mg prn
Onset / Peak / Duration: IV – Onset in 1-2 minutes / Peak in 5-15 minutes / Duration 45 minutes or longer
IM – Onset in 2-5 minutes / Peak in 5-15 minutes / Duration 45 minutes or longer
Administration Instructions: Have available when administering opioids. Titrate to effect to manage negative opioid effects, but
use caution that pain is still managed.
Contraindications: Non-opioid drug respiratory depression; pregnancy category B
Adverse/Side Effects: Analgesia reversal, tremors, hyperventilation, drowsiness, sweating; increased BP, tachycardia; nausea,
vomiting.
Interactions: Reverses analgesic effects of narcotic (opiate) agonists and agonist-antagonists.
Mission Impact: GROUNDING medication for personnel on flight status.
K-9 Dosage: 1mg (0.02-0.04mg/kg) IV/IM
MOXIFLOXACIN (AVELOX)
Class: Antimicrobial – antibiotic; fluoroquinolone
TCCC Indications: Recommended for all open combat wounds if unable to take PO meds as a component of the Combat Wound
Medication Pack (CWMP)
DOSE: 400 mg PO qd
Onset / Peak / Duration: Onset Varies / Peak 1-3 hours / Duration 3-4 hours
Administration Instructions: PO
Contraindications: Quinolone hypersensitivity; hepatic insufficiency; syphilis; arrhythmias; myocardial ischemia or infarction; QT
c
prolongation, hypokalemia, or those receiving Class IA or Class III antiarrhythmic drugs; pregnancy category C.
Adverse/Side Effects: Dizziness, headache, peripheral neuropathy, nausea, diarrhea, abdominal pain, vomiting, taste perversion,
abnormal LFTs, dyspepsia, tendon rupture.
Interactions: Iron, zinc, antacids, aluminum, magnesium, calcium, sucralfate decrease absorption; atenolol, cisapride,
erythromycin, antipsychotics, TCAs, quinidine, procainamide, amiodarone, sotalol may prolong QT
C
interval; may cause false
positive on opiate screening tests.
Mission Impact: GROUNDING medication for personnel on flight status.
K-9 Dosage: DO NOT GIVE
44
TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
PHARMACOLOGY REFERENCE
ONDASETRON ORAL DISSOLVING TABLET (ZOFRAN)
Class: GI agent – 5-HT
3
antagonist, antiemetic
TCCC Indications: For prevention and management of nausea and vomiting associated with pain management medications.
DOSE: 325–650 mg PO q4–6h (max: 4 g/d)
Administration Instructions: PO
Contraindications: Hypersensitivity to ondansetron; pregnancy category B
Adverse/Side Effects: Dizziness, light-headedness, headache, sedation; diarrhea, constipation, dry mouth
Interactions: Rifampin may decrease ondansetron levels
Mission Impact: GROUNDING medication for personnel on flight status.
TRANEXEMIC ACID (TXA, CYKLOKAPRON)
Class: Antifibrinolytic agent
TCCC Indications: For patients anticipated to need significant blood transfusion; hemorrhagic shock, one or more major
amputations, penetrating torso trauma, or evidence of severe bleeding.
DOSE: 1 gram in separate 100cc of NS or LR slow IV push over 10 min. Do not administer in same bag as blood products or
Hextend. Administer a second infusion of 1 gram after 500cc fluid challenge.
Administration Instructions: Administer as soon as possible but not later than 3 hours after injury. Ensure documentation on
casualty card and/or attach/write on patient’s chest wall.
Contraindications: subarachnoid hemorrhage, active intravascular clotting, Pregnancy Category B.
Adverse/Side Effects: Blurred vision or impaired color vision. Gastrointestinal disturbances (nausea, vomiting, diarrhea) may
occur but disappear when the dosage is reduced. Hypotension has been observed when intravenous injection is too rapid. To
avoid this response, the solution should not be injected more rapidly than 100mg per minute.
Interactions: should not be administered concomitantly with Factor IX Complex concentrates or Anti-inhibitor Coagulant
concentrates, as the risk of thrombosis may be increased.
45

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
EXAMPLE TACTICAL MEDICAL CONOP
46

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
ABOUT THE
COMMITTEE ON TACTICAL COMBAT CASUALTY CARE
AND THE JOINT TRAUMA SYSTEM
CoTCCC MISSION:
To develop on an ongoing basis the best possible
set of trauma care guidelines customized for the
tactical environment and to facilitate the transition
of these recommendations into battlefield trauma
care practice.
The Committee on Tactical Combat Casualty Care (CoTCCC) is the Prehospital arm of the Joint Trauma System for the
Department of Defense.
The CoTCCC is composed of 42 voting members specially selected as subject-matter experts in trauma, battlefield medicine,
tactical medicine, prehospital medicine and their experience in the deployed combat environment.
The TCCC Working Group is composed of the CoTCCC and hundreds of subject-matter experts across many domains and
liaisons from DoD, Government and Partner nation organizations.
The CoTCCC and the TCCC Working Group focus all of their efforts on providing the best recommendations for training and
equipment for our individual service members, combat medics, corpsman, pararescue, and med techs going into harm's way
around the world.
JTS MISSION:
The mission of the Joint Trauma System (JTS) is to provide evidence-
based process improvement of trauma and combat casualty care, to
drive morbidity and mortality to the lowest possible levels, and to
provide evidence-based recommendations on trauma care and
trauma systems across the Department of Defense (DoD).
The DoD CENTER OF EXCELLENCE FOR TRAUMA
DATA ACQUISITION: Mines the medical records to abstract, code, and enters critical trauma data into the DoDTR database for use in
support of the JTS mission.
DATA ANALYSIS: Develops queries and provides data from the DoDTR in response to requests for information. Conducts classified and
non-classified data analysis.
DATA AUTOMATION: Supports the information technology for the DoDTR and data-related special projects. Designs and implements
special-project database applications, related architecture, and documentation. Handles documentation needs for JTS to maintain Program
compliance with the Defense Health Agency.
PERFORMANCE IMPROVEMENT: Coordinates performance improvement (PI) activities across the spectrum of trauma care. Participates
in the development, maintenance, and adherence to Clinical Practice Guidelines. Develops PI course content and training, and resolves
trauma system patient care issues.
EDUCATION: Develops and conducts pre-deployment training of the Joint Theater Trauma System (JTTS) teams, DoDTR user training, and
JTS staff training. Develops educational products for combatant command trauma system development. Secures continuing education
credits and coordinates performance improvement and other trauma related courses.
47

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC REFERENCES & SELECTED READING
TACTICAL COMBAT CASUALTY CARE IN SPECIAL OPERATIONS.
BUTLER FK, HAGMANN J, BUTLER EG. MIL MED. 1996;161(SUPPL):3–16. (ORIGINAL TCCC ARTICLE)
PREHOPSITAL TRAUMA LIFE SUPPORT (PHTLS) MANUAL, 8
TH
EDITION (MILITARY)
Butler FK, Giebner SD, Pons PT, McSwain NE, eds. Burlington, MA: Jones & Bartlett Learning; 2014.
SAVING LIVES ON THE BATTLEFIELD: A JOINT TRAUMA SYSTEM REVIEW OF PRE-HOSPITAL TRAUMA CARE IN
COMBINED JOINT OPERATING AREA—AFGHANISTAN (CJOA-A) EXECUTIVE SUMMARY.
KOTWAL RS, BUTLER FK, EDGAR EP, SHACKELFORD SA, BENNETT DR, BAILEY JA. J SPEC OPER MED . 2013;13(1):77– 85.
SAVING LIVES ON THE BATTLEFIELD (PART II) - ONE YEAR LATER: A JOINT THEATER TRAUMA SYSTEM
AND JOINT TRAUMA SYSTEM REVIEW OF PREHOSPITAL TRAUMA CARE IN COMBINED JOINT OPERATIONS
AREA-AFGHANISTAN (CJOA-A).
SAUER SW, ROBINSON JB, SMITH MP, GROSS KR, KOTWAL RS, MABRY RL, BUTLER FK, STOCKINGER ZT, BAILEY JA, MAVITY ME, GILLIES
DA 2
ND
J SPEC OPER MED. 2015 SUMMER;15(2):25-41
ELIMINATING PREVENTABLE DEATH ON THE BATTLEFIELD.
KOTWAL RS, MONTGOMERY HR, KOTWAL BM, CHAMPION HR, BUTLER FK JR, MABRY RL, CAIN JS, BLACKBOURNE LH, MECHLER KK,
HOLCOMB JB. ARCH SURG. 2011 DEC;146(12):1350-8. DOI: 10.1001/ARCHSURG.2011.213. EPUB 2011 AUG 15.
TRAGEDY INTO DRAMA: AN AMERICAN HISTORY OF TOURNIQUET USE IN THE CURRENT WAR.
KRAGH JF JR, WALTERS TJ, WESTMORELAND T, MILLER RM, MABRY RL, KOTWAL RS, RITTER BA, HODGE DC, GREYDANUS DJ, CAIN JS,
PARSONS DS, EDGAR EP, HARCKE T, BAER DG, DUBICK MA, BLACKBOURNE LH,MONTGOMERY HR, HOLCOMB JB, BUTLER FK. J SPEC
OPER MED. 2013 FALL;13(3):5-25.
DEATH ON THE BATTLEFIELD (2001-2011): IMPLICATIONS FOR THE FUTURE OF COMBAT CASUALTY CARE.
EASTRIDGE BA, MABRY RL, SEGUIN P, CANTRELL J, TOPS T, URIBE P, MALLET O, ZUBKO T, OETJEN-GERDES L, RASMUSSEN TE, BUTLER
FK, KOTWAL R, HOLCOMB JB, WADE C, CHAMPION H, LAWNICK M, MOORES L, BLACKBOURNE LH. J TRAUMA ACUTE CARE SURG. 2012
VOLUME 73, NUMBER 6, SUPPLEMENT 5.
IMPLEMENTING AND PRESERVING THE ADVANCES IN COMBAT CASUALTY CARE FROM IRAQ AND
AFGHANISTAN THROUGHOUT THE US MILITARY.
BUTLER FK JR, SMITH DJ, CARMONA RH. J TRAUMA ACUTE CARE SURG. 2015 VOLUME 79, NUMBER 2.
LEADERSHIP LESSONS LEARNED IN TACTICAL COMBAT CASUALTY CARE.
BUTLER FK. J TRAUMA ACUTE CARE SURG. 2017.
TACTICAL COMBAT CASUALTY CARE: BEGINNINGS.
BUTLER FK. WILDERNESS ENVIRON MED. 2017
THE TRANSITION TO THE COMMITTEE ON TACTICAL COMBAT CASUALTY CARE.
GIEBNER SD. WILDERNESS ENVIRON MED. 2017
BATTLEFIELD TRAUMA CARE THEN AND NOW: A DECADE OF TACTICAL COMBAT CASUALTY CARE.
BUTLER FK, BLACKBOURNE LH. J TRAUMA ACUTE CARE SURG. 2012 VOLUME 73, NUMBER 6
48

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC CHANGE REFERENCES
2010-2017
TCCC GUIDELINES COMPREHENSIVE REVIEW AND UPDATE: TCCC GUIDELINES CHANGE 16-03.
MONTGOMERY HR, BUTLER FK, KERR W, CONKLIN CC, MORISSETTE DJ, REMLEY MA, SHAW TA, RICH TA. J SPEC OPER MED. 2017 SUMMER;17(2):19-36.
THE USE OF PELVIC BINDERS IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 16-02.
SHACKELFORD SA, HAMMESFAHR R, MORISSETTE D, MONTGOMERY HR, KERR W, BROUSSARD M, BENNETT BL, DORLAC WC, BREE S, BUTLER FK. J SPEC
OPER MED. 2017 SPRING;17(1):135-147.
MANAGEMENT OF EXTERNAL HEMORRHAGE IN TACTICAL COMBAT CASUALTY CARE: THE ADJUNCTIVE USE OF XSTAT
COMPRESSED HEMOSTATIC SPONGES: TCCC GUIDELINES CHANGE 15-03.
SIMS K, MONTGOMERY HR, BOWLING F, DITURO P, KHEIRABADI BS, BUTLER FK JR, J SPEC OPER MED. 2016 SPRING;16(1):19-28.
EMERGENCY CRICOTHYROIDOTOMY IN TACTICAL COMBAT CASUALTY CARE.
MABRY R, FRANKFURT A, KHAROD C, BUTLER F. J SPEC OPER MED. 2015 FALL;15(3):11-19.
REPLACEMENT OF PROMETHAZINE WITH ONDANSETRON FOR TREATMENT OF OPIOID- AND TRAUMA-RELATED NAUSEA AND
VOMITING IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 14-03.
ONIFER DJ, BUTLER FK JR, GROSS KR, OTTEN EJ, PATTON R, RUSSELL RJ, STOCKINGER Z. J SPEC OPER MED. 2015 SUMMER;15(2):9-16.
OPTIMIZING THE USE OF LIMB TOURNIQUETS IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 14-02.
SHACKELFORD SA, BUTLER FK JR, KRAGH JF JR, STEVENS RA, SEERY JM, PARSONS DL, MONTGOMERY HR, KOTWAL RS, MABRY RL, BAILEY JA. J SPEC
OPER MED. 2015 SPRING;15(1):17-31.
FLUID RESUSCITATION FOR HEMORRHAGIC SHOCK IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 14-01
BUTLER FK, HOLCOMB JB, SCHREIBER MA, KOTWAL RS, JENKINS DA, CHAMPION HR, BOWLING F, CAP AP, DUBOSE JJ, DORLAC WC, DORLAC GR, MCSWAIN
NE, TIMBY JW, BLACKBOURNE LH, STOCKINGER ZT, STRANDENES G, WEISKOPF RB, GROSS KR, BAILEY JA. –2 JUNE 2014. J SPEC OPER MED. 2014
FALL;14(3):13-38. REVIEW.
MANAGEMENT OF EXTERNAL HEMORRHAGE IN TACTICAL COMBAT CASUALTY CARE: CHITOSAN-BASED HEMOSTATIC GAUZE
DRESSINGS: TCCC GUIDELINES CHANGE 13-05
BENNETT DR, LITTLEJOHN L, KHEIRABADI BS, BUTLER FK, KOTWAL RS, DUBICK MA, BAILEY JA. J SPEC OPER MED. 2014 FALL;14(3):12-29.
A TRIPLE-OPTION ANALGESIA PLAN FOR TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 13-04
BUTLER FK, KOTWAL RS, BUCKENMAIER CC 3RD, EDGAR EP, O’CONNOR KC, MONTGOMERY HR, SHACKELFORD SA, GANDY JV 3RD, WEDMORE IS, TIMBY
JW, GROSS KR,BAILEY JA. . J SPEC OPER MED. 2014 SPRING;14(1):13-25.
MANAGEMENT OF JUNCTIONAL HEMORRHAGE IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 13-03.
KOTWAL RS, BUTLER FK, GROSS KR, KRAGH JF, KHEIRABADI BS, BAER DG, DUBICK MA, RASMUSSEN TE, WEBER MA, BAILEY JA. J SPEC OPER MED. 2013
WINTER;13(4):85-93.
MANAGEMENT OF OPEN PNEUMOTHORAX IN TACTICAL COMBAT CASUALTY CARE: TCCC GUIDELINES CHANGE 13-02.
BUTLER FK, DUBOSE JJ, OTTEN EJ, BENNETT DR, GERHARDT RT, KHEIRABADI BS, GROSS KR, CAP AP, LITTLEJOHN LF, EDGAR EP, SHACKELFORD SA,
BLACKBOURNE LH, KOTWAL RS, HOLCOMB JB, BAILEY JA. J SPEC OPER MED. 2013 FALL;13(3):81-6.
THE TACTICAL COMBAT CASUALTY CARE CASUALTY CARD TCCC GUIDELINES PROPOSED CHANGE 1301.
KOTWAL RS, BUTLER FK, MONTGOMERY HR, BRUNSTETTER TJ, DIAZ GY, KIRKPATRICK JW, SUMMERS NL, SHACKELFORD SA, HOLCOMB JB, BAILEY JA. J
SPEC OPER MED. 2013 SUMMER;13(2):82-7.
MANAGEMENT OF TRAUMATIC BRAIN INJURY IN TACTICAL COMBAT CASUALTY CARE.
DEFENSE HEALTH BOARD MEMO, 2012-04, 26 JUL 2012.
DHB RECOMMENDATION REGARDING THE ADDITION OF TRANEXAMIC AICD TO THE TACTICAL COMBAT CASUALTY CARE
GUIDELINES.
DEFENSE HEALTH BOARD MEMO, 2011-06, 23 SEP 2011.
DHB RECOMMENDATION PERTAINING TO TACTICAL COMBAT CASUALTY CARE GUIDELINES ON THE PREVENTION OF
HYPOTHERMIA.
DEFENSE HEALTH BOARD MEMO, 2010-06, 10 DEC 2010.
49

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
GLOSSARY
50
AAL
anterior axillary line
ASAP
as soon as possible
AVPU
Alert/Verbal/Pain/Unresponsive
AXP
ambulance exchange point
BAS
battalion aid s tation
BVM
bag
-valve-mask
CASEVAC
casualty evacuation
CAT
Combat Application Tourniquet®
CCP
casualty collection point
CEP
casualty evacuation point
CG
Combat Gauze®
Class VIII
class of supply for medical
CLS
combat lifesaver
COMSEC
communications security
CoTCCC
Commi ttee on Tactical Combat Casualty Care
CPG
clinical practice guidelines
CRoC
Combat Ready Clamp®
CRS
cas ualty response system
CTS
Combat Trauma System
CUF
Ca re Under Fire (phase)
CWMP
combat wound medication pack
DoDTR
department of defense trauma registry
EMT
Emergency Medical Tourniquet®
HLZ
helcopter landing zone
HPMK
Hypothermia Prevention and Management Kit®
HRS
Heat Reflective Shell®
IAW
in accordance with
IED
improvised explosive device
IM
intramuscular
IN
intranasal
IO
intraosseous
IV
intravenous
JETT
Junctional Emergency Treatment Tool®
JTS
Joint Trauma System
JTTS
joint theater trauma system
LR
Lactated Ringer's
LSI
life
-saving intervention
MASSCAL
mass casualty
MEDEVAC
medical evacuation
mmHG
millimeters of mercury
MSO4
Morphine Sulfate
MTF
medical treatment facility
NS
normal saline / sodium chloride
ODT
orally disolving tablet
OTFC
oral trnsmucosal fentanyl citrate
PCO2
partial pressure of carbon dioxide
PI
performance improvement
PO
by mouth / oral
POI
point
-of-injury
PRN
pro re nata (as needed/circumstances require)
RBC
red blood cells
SAM
-JT
SAM
-Junctional Tourniquet®
SBP
sys tolic blood pressure
SGA
supraglottic airway
SOF
special operations forces
SOFT
-T
Special Operations Forces Tactical Tourniquet®
SOP
standard operating procedure
TACEVAC
Tactical Evacuation (phase)
TBI
traumatic brain injury
TBSA
total body surface area
TCCC or TC3
Tactical Combat Casualty Care
TFC
Tactical Field Care (phase)
TQ
tourniquet
TXA
tranexamic acid
USAISR
US Army Ins titute of Surgical Research

1 oz = 30 g
1 lb = 16 oz = 0.45 kg
1 ton = 2000 lbs = 907 kg
1 grain = 65 mg
1 g = 001 kg = 0.36 oz
1 kg = 1000 g = 2.2 lbs
Weight Conversions
1 fl oz = 30 ml = 30 cc
1 US Gal = 128 fl oz = 3785
ml
1 cc = 0.001 liter
1 ml = 1 cc = 0.34 fl oz
1 liter = 1000 ml = 340 fl oz
Volume Conversions
WEIGHT LENGTH
lb = kg X 2.2 Lnches = cm X 0.394
kg = lb X 0.45 c = inches X 2.54
TEMPERATURE
F = (1.8) X C + 32
C = (F – 32) / (1.8)
Conversion Formulas
Quick Conversions
HEIGHT WEIGHT TEMPERATURE
ft/in in cm lb kg F C
4'8" 56 142 40 18.2 212 100
4'9" 57 145 50 22.7 108 42.2
4'10" 58 147 60 27.3 107 41.6
4'11" 59 150 70 31.8 106 41.1
5'0" 60 152 80 36.4 105 40.6
5'1" 61 155 90 40.9 104 40.0
5'2" 62 157 100 45.5 103 39.4
5'3" 63 160 110 50.0 102 38.9
5'4" 64 163 120 54.5 101 38.3
5'5" 65 165 130 59.1 100 37.8
5'6" 66 168 140 63.6 99 37.2
5'7" 67 170 150 68.2 98 36.7
5'8" 68 173 160 72.7 98.6 37.0
5'9" 69 175 170 77.3 97 36.1
5'10" 70 178 180 81.8 96 35.6
5'11" 71 180 190 86.4 95 35.0
6'0" 72 183 200 90.9 94 34.4
6'1" 73 185 210 95.5 93 34.0
6'2" 74 188 225 102.3 92 33.3
6'3" 75 191 250 113.6 91 32.8
6'4" 76 193 275 125.0 90 32.1
6'5" 77 196 300 136.4
IV FLUID RATES IN DROPS PER MINUTE
ml/HR 50 75 80 100 125 150 175 200 250
10GTT- 8 13 13 17 21 25 29 33 42
15GTT- 12 19 20 25 31 37 44 50 62
60GTT- 50 75 80 100 125 150 175 200 250
TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
CONVERSIONS
51

TACTICAL COMBAT CASUALTY CARE
(TCCC / TC3)
TCCC
DRUG QUICK REFERENCE
ACETAMINOPHEN (Tylenol): 325-650 mg PO q8h prn (max: 4 g/d)
ERTAPENEM (Invanz): 1g IV/IM q24h
FENTANYL ORAL LOZ (Actiq): 400-800 mcg (max: 1600 mcg/d)
HETASTARCH (Hextend): 500-1000ml IV
KETAMINE (Ketalar): 50mg IM/IN q1h OR 20mg IV/IO q30m until nystagmus or max dose of
100mg
LIDOCAINE (Xylocaine): Infiltration 0.5%-2% injection
MELOXICAM (Mobic): 15 mg PO daily
MORPHINE SULFATE (MSO4): 5-15 mg slow IV push; titrate to pain
MOXIFLOXACIN (Avelox): 400 mg PO/IV daily
NALAXONE (Narcan): 0.4-2.0 mg IV/IM; repeat q2-3m up to 10 mg prn
ONDANSETRON (Zofran): 4 mg slow IV push or IM q8h prn OR 4mg ODT PO q8h prn
TRANEXEMIC ACID (TXA): 1 gm in 100cc of NS or LR slow IV push over 10m (<3h of
wounding)
Copyright, 2017 by Harold R. Montgomery
ISBN: 978-0-692-90697-2
