

Table of Contents
Benefits Eligibility & Options…………………………………………… 1
Health Options and Coverage Details………………………………... 3
Schedule of Benefits………………………………………………........ 4
Health Premiums Per Pay Period (Before Tax)……………………... 28
Dental Options & Coverage Details…………………………………... 28
Vision Option & Coverage Details…………………………………….. 30
Health Care Flexible Spending Account……………………………… 31
Dependent Care Flexible Spending Account………………………… 33
Life and Loss Benefits
(Life and AD&D)…………………………….. 34
Income Protection Benefits
(Short-Term and Long-Term Disability). 37
Long-Term Disability (LTD)………………………………………….… 38
Paid Time Off Benefits………………………………….……………... 39
401(k) Savings Plan…………………………………………….……… 42
Voluntary ARAG Legal Services w/ ID Theft Protection…….……… 43
Supplemental Health Benefits ………………………………….……… 43
(Accident, Critical Illness and Hospital Indemnity Insurance)
Other Benefits Available to You Throughout the Year………..………44
(Nationwide Pet Insurance and Amplifon Hearing Discount Program)
Contact Information & References…………………………….……… 45
NOTE: This packet is only a summary of the Employee Benefits program. A more complete description of the program’s
provisions and benefits can be found in the Summary Plan Description
, Plan documents and underlying contracts. In the event
of a discrepancy between the Summary Plan Description and the Plan documents, the plan documents and underlying contracts
will rule. The Company reserves the right to make final decisions concerning the interpretation and application of the Employee
Benefit’s program and the benefit plans.

1
We offer a variety of benefits to help protect
what matter most to our employees.
This guide will help you understand benefits that are offered here at Mutual of Omaha. As you can tell
below in the chart, we have benefits that are separate from your health insurance and even more that
are not listed in the chart below. Throughout your career, you’ll have opportunities to make choices
that can help you reach your financial health and happiness goals. Selecting your benefits is one of
those opportunities.
Benefits Eligibility & Options
The following benefit plans are available according to your employment status, if you enroll during your
designated enrollment period:
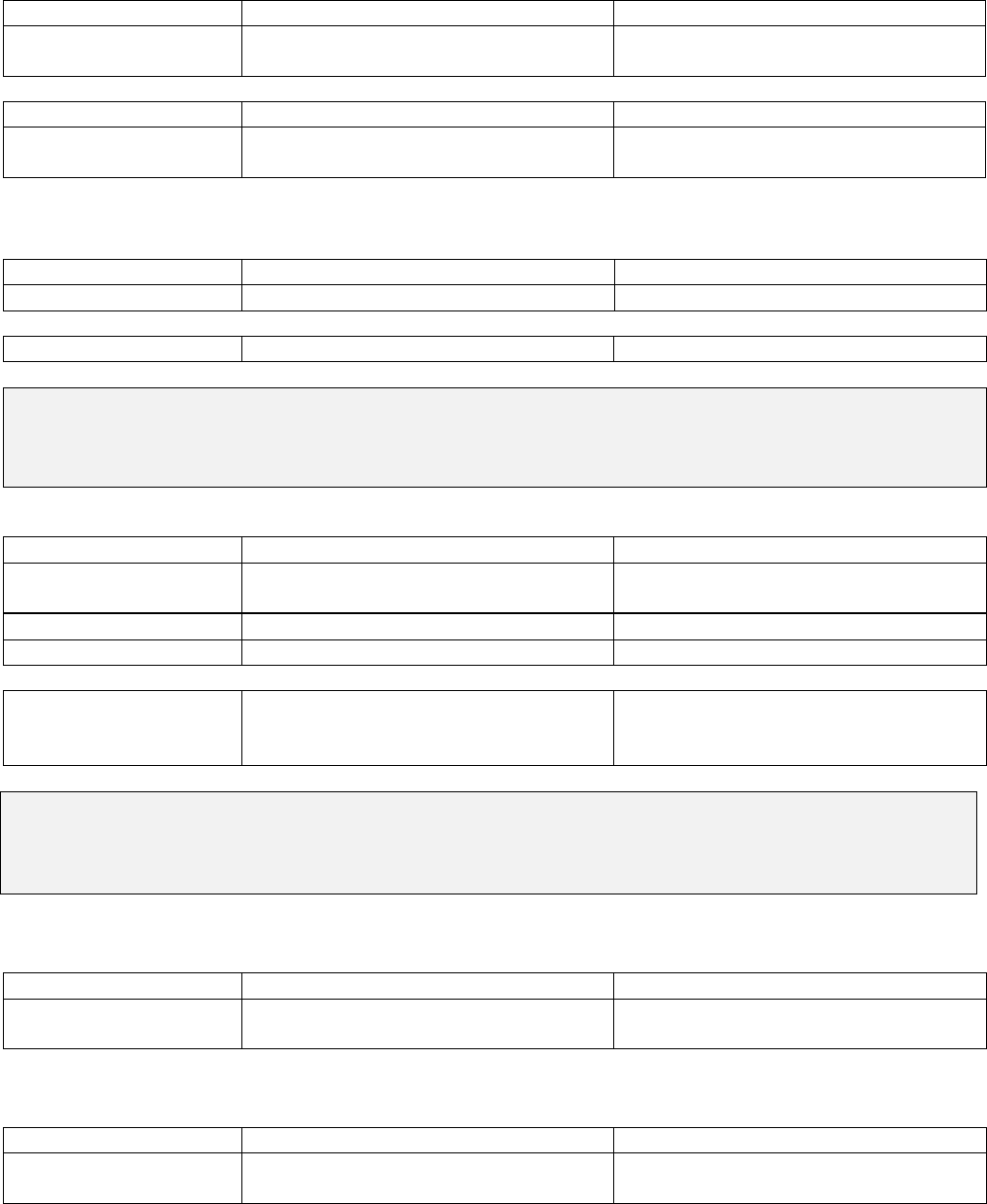
Regular Status
Temporary
Status
Benefit Plan
Coverage Effective
Date
30 hrs
or more
20 – 29
hrs
< 20 hrs 40 or less
Basic Employee Life & Basic
Long-Term Disability
Date of Hire
X
Health, Dental, Vision Benefits Effective Date
X
*
Supplemental Life, Spouse Life, Child
Life, Basic Accidental Death &
Dismemberment, Supplemental
Accidental Death & Dismemberment
Benefits Effective Date
X
Supplemental Long-Term Disability Benefits Effective Date
X
Health Care Flexible
Spending Account
Benefits Effective Date
X
Voluntary Accident Insurance Benefits Effective Date
X
Voluntary Critical Illness Insurance Benefits Effective Date
X
Voluntary Hospital Indemnity
Insurance
Benefits Effective Date
X
Dependent Care Flexible Spending
Account
Benefits Effective Date
X X X
ARAG Legal Services w/ ID Theft
Protection
Benefits Effective Date
X
X
X
Nationwide Pet Insurance Benefits Effective Date
X
X
X
X
Amplifon Hearing Discount Program Benefits Effective Date
X
X
X
X
401(k) Plan Benefits Effective Date
X
X
X
X
Vacation Accrual Benefit Effective Date
X
X
X
X
Personal Time
Date of Hire
X
X
X
X
Holidays
Date of Hire
X
X
X
X
Tuition Reimbursement
Date of Hire
X
X
*May be eligible for health only benefits if scheduled hours are 30 hours or more per week

2
Your benefit effective date is based on your hire date with the company:
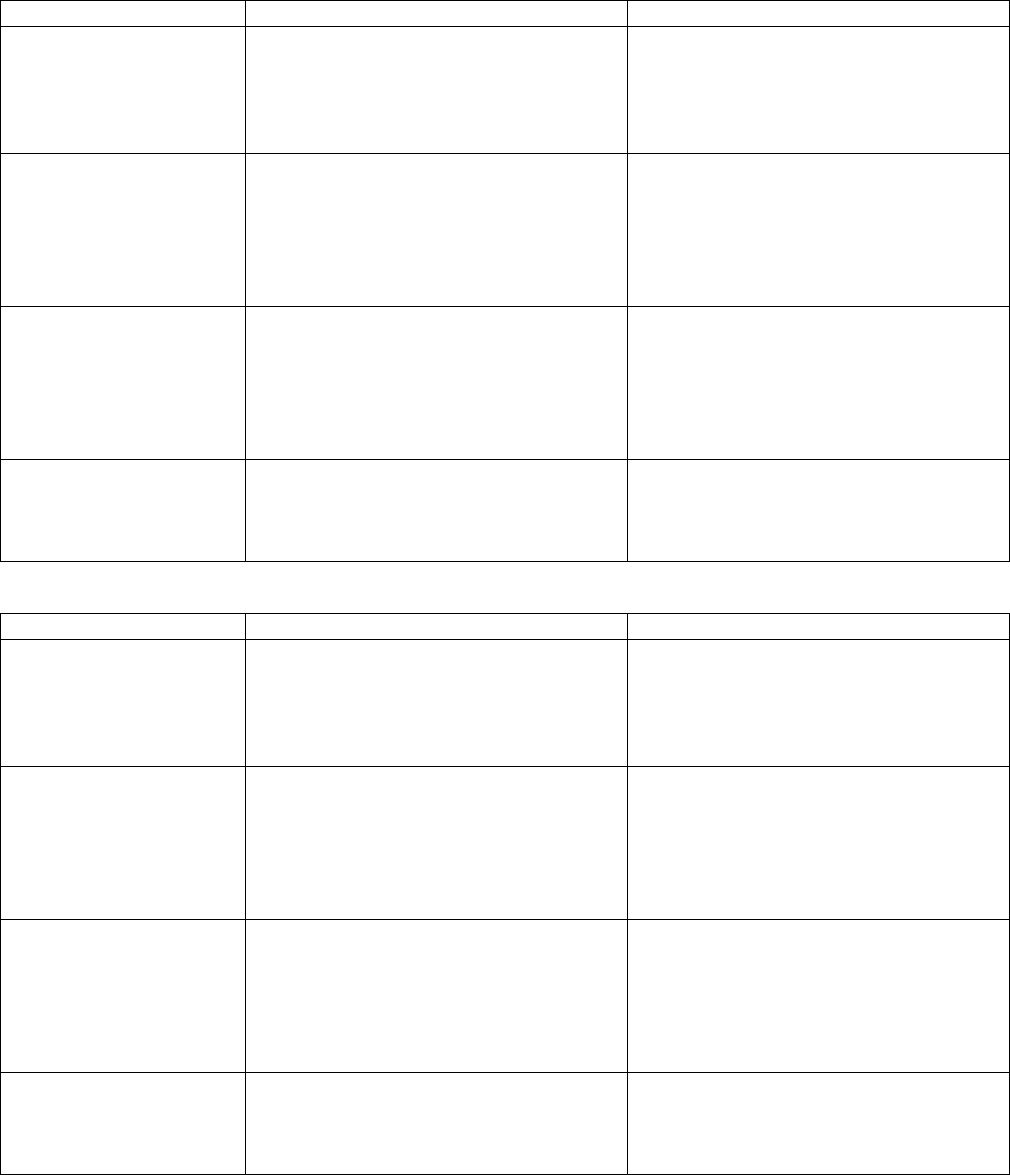
Hire Dates
Benefit Effective Date
1/1 – 1/18
2/1
1/19 – 2/16
3/1
2/17 - 3/18
4/1
3/19 - 4/17
5/1
4/18 - 5/18
6/1
5/19 - 6/17
7/1
6/18 - 7/18
8/1
7/19 - 8/18
9/1
8/19 - 9/17
10/1
9/18 - 10/18
11/1
10/19 - 11/17
12/1
11/18 - 12/18
1/1
12/19 - 12/31
2/1
Eligible Dependents
You may elect coverage for applicable benefits for yourself and any of the following dependents:
•
Your spouse
o
A person to whom you are legally married, whether of the opposite sex or the same sex, as
recognized and allowed by the laws of the state in which you become married. Copy of
certified marriage license is required to establish eligibility.
• Your Child, or Foster Child, up to age 26, unless the Child meets the requirements as an
Incapacitated Child
o
Your naturally born child; a child that you have legally adopted; your step-child; your foster
child who has been placed in your care pursuant to a judgment, decree or court order; or a
child for whom you have been appointed legal guardian.
NOTE: If you are enrolling a spouse for any coverage, you must provide a copy of your certified marriage license, if you are
married, prior to your benefits effective date. You must also provide a birth certificate for each child you are covering under
any of your benefits prior to your benefits effective date. These can be faxed to (402) 351-6192 or scanned/ emailed to
benefits.hotline@mutualofomaha.com.
Level of Coverage Options
You can elect enrollment coverage for:
•
Employee Only (You are the only person covered)
•
Employee + One (You and one eligible dependent is covered, spouse or child)
•
Employee + Family (You and two or more eligible dependents are covered)
Enrollment
Mutual of Omaha utilizes an electronic enrollment process. You will need to make elections prior to
your benefits effective date.
Coverages elected remain in effect throughout the year unless you experience a qualified life event. A
lot can happen during the year. Each fall, we offer an annual enrollment period so you can make sure
your benefits help protect your changing needs and to make your elections for the next year.
Qualified Life Events
IRS regulations determine when you can make changes to your benefit elections depending on
changes in your status. Following are some examples of what may qualify:

3
• You become married or divorced
• You acquire an eligible dependent
• Your spouse loses health coverage under an employer’s group plan because of a change in
your spouse’s job status or because the spouse’s employer terminates its group plan
• Your dependent loses his or her eligibility under this Plan or another employer’s group plan
• Your spouse or dependent obtains coverage under an employer’s group plan because of a
change in his or her job status or because his or her employer begins offering a group plan
• Your spouse makes a change during his or her employer’s annual enrollment, with an effective
date other than January 1.
In most situations, you may only add or delete dependents from your current coverage as the result of
a Life Event change in status with the proper documentation, if required. Changes to your plan options
must be consistent with the Life Event. If you increase the payroll deduction amount for Your Health
Care Flexible Spending Account with an eligible Life Event, the increased dollar amount must be used
for expenses incurred after the Life Event for services to be consistent with the Life Event.
Click here for more information on Qualified Life Events
.
To make a change in coverage due to a Life Event change in status, you must report the change in
status to Corporate Benefits and Services Department within 31 days of the event. If you do not
contact the Corporate Benefits and Service Department within 31 days of the Life Event and you are
electing to add a dependent, you will need to wait until the next annual enrollment. If you are removing
a spouse and did not contact the Corporate Benefits Service Department, you will be required to pay
the premium for that dependent for the remainder of the Benefit Year, but the dependent will be
removed from your coverages, if ineligible. To request a Life Event change online, sign into
PeopleSoft>click on the Benefits tile, and then click on Life Events.
You may also contact the Corporate Benefits and Services Department by calling the HR Hotline at
402-351-3300 and select option “1” or toll free 1-800-365-1405. You may also e-mail the Benefits
Hotline for any questions you have regarding qualified Life Event changes.
Health Options and Coverage Details
Waive Health Coverage
Waiving health coverage means that you are not electing health coverage through your employment
with Mutual of Omaha. If you waive coverage, you should have health coverage through another plan
or you may be subject to fines/ penalties for not carrying health coverage (per the Affordable Care
Act). When considering other options available to you, such as a spouse’s plan, compare your options,
look at physicians in the network, premiums and/or differences in coverage to find the best option for
you and your family.
Many plans, including those offered to Mutual of Omaha employees, have a Coordination of Benefits
plan provision. With Coordination of Benefits plan provisions, one plan will pay its full benefits first,
then the other plan may only pay up to the amount what would have paid had it been the primary plan.
You may find you are paying premium for two plans, but not receiving the anticipated benefits of both
at the same time.
If you waive health coverage and experience a Life Event, such as a loss of other group health
coverage, you can enroll in our plan by contacting us within 31 days of the event.

4
Health Coverage
Our health coverage is through Aetna. The health plan allows you complete freedom to go to any in-
network health care provider. If you use an out-of-network provider, you will have a higher out of
pocket expense. This includes direct access to specialists without prior approval from the plan. When
using in-network providers, you reduce your out-of-pocket health care expenses because providers
have agreed upon certain rates for their services, deductibles are lower, and the plan pays a larger
percentage of the expenses. If you choose out-of-network providers, you will have higher out of pocket
costs because the deductibles are higher, and the plan pays a smaller percentage of the expenses.
In-network providers can
be found online or by contacting Aetna Customer Service. This website and contact number for
customer services is referenced on the last page of this guide and is available on the ID card you’ll
receive after enrolling in the plan.
Deductible and Out-of-Pocket Maximum
The health plan has two deductible options available. A deductible is the amount of covered expenses
that you must pay before the plan will start paying benefits, except for preventive benefits.
If you reach the out-of-pocket maximum, the health plan will pay 100% of incurred allowed expenses
for the remaining portion of the calendar year.
We will recognize prior health plan deductibles for new hires and employees of an acquired company
only with respect to medical (not prescription) expenses applied to deductibles of the plan that
provided coverage during the employee’s first Plan Year (January 1 – December 31) of service with
our Company. This does not include copays and coinsurance applied towards your prior health
coverage. Explanation of Benefits (EOB’s) reflecting YTD deductibles can be faxed to Aetna; Attn:
Tammy Richardson at 860-907-3894.
Please note that our High Deductible $1250/ $2500 PPO plan is not a qualified plan for HSA account
set up. We offer a Health Care Flexible Spending Account (FSA).
For more information on your health benefits, click here
.
Schedule of Benefits
As this is an ERISA plan, you have certain rights under the Plan. Please see the Administrative
Information Section of the Summary Plan Description
for additional information.
Prepared for:
Employer: Mutual of Omaha Insurance Company
Contract number: MSA-0867953
Control number: 0847850
Plan name: Choice POS II - $750 & $1,250 Deductible Plan
Schedule of benefits: 1A & 1B
Plan effective date:
January 1, 2024
Plan issue date:
January 1, 2024
Third Party Administrative Services provided by Aetna Life Insurance Company

5
This schedule of benefits (schedule) lists the deductibles, copayments or payment percentage, if
any apply to the covered services you receive under the plan. You should review this schedule to
become aware of these and any limits that apply to these services.
How your cost share works
• The deductibles and copayments, if any, listed in the schedule below are the amounts that
you pay for covered services.
- For the covered services under your medical plan, you will be responsible for the dollar
amount
- For pharmacy benefits where a percentage cost share acts like a copayment, you will be
responsible for the percentage amount
• Payment percentage amounts, if any, listed in the schedule below are what the plan will pay
for covered services.
• Sometimes your cost share shows a combination of your dollar amount copayment that you
will be responsible for and the payment percentage that your plan will pay.
• You are responsible to pay any deductibles, copayments and remaining payment
percentage, if they apply and before the plan will pay for any covered services.
• This plan doesn’t cover every health care service. You pay the full amount of any health care
service you get that is not a covered service.
• This plan has limits for some covered services. For example, these could be visit, day or
dollar limits. They may be:
- Combined limits between in-network and out-of-network providers
- Separate limits for in-network and out-of-network providers
- Based on a Calendar Year (January 1 - December 31) under this plan
See the schedule for more information about limits.
• Your cost share may vary if the covered service is preventive or not. Ask your physician or
contact us if you have a question about what your cost share will be.
For examples of how cost share and deductible work, go to the Using your Aetna benefits section
under Individuals & Families at https://www.aetna.com/
Important note:
Covered services are subject to the deductible, maximum out-of-pocket, limits, copayment or
payment percentage unless otherwise stated in this schedule.
Under this plan, your copayment does not apply to any deductible.
How your deductible works
The deductible is the amount you pay for covered services each year before the plan starts to pay.
This is in addition to any copayment or payment percentage you pay when you get covered
services from an in-network, out-of-network provider. This schedule shows the deductible
amounts that apply to your plan. Once you have met your deductible, we will start sharing the cost
when you get covered services. You will continue to pay copayments or payment percentage, if
any, for covered services after you meet your deductible.
How your PCP or physician office visit cost share works
You will pay the PCP cost share when you get covered services from any PCP.
How your maximum out-of-pocket works
This schedule shows the maximum out-of-pocket limits that apply to your plan. Once you reach
your maximum out-of-pocket limit, your plan will pay for covered services for the remainder of that
year.

6
Contact us
We are here to answer questions. See the Contact us section in your booklet.
This schedule replaces any schedule of benefits previously in use. Keep it with your booklet.
Plan features
Precertification covered services reduction
This only applies to out-of-network covered services:
Your booklet contains a complete description of the precertification process. You will find details in
the Medical necessity and precertification section.
If precertification for covered services isn’t completed, when required, it results in the following
benefit reduction:
• A $300 benefit reduction applied separately to each type of covered service
You may have to pay an additional portion of the recognized charge because you didn’t get
precertification. This portion is not a covered service and doesn’t apply to your deductible or
maximum out-of-pocket limit, if you have one.
Deductible
You have to meet your deductible before this plan pays for benefits.
Deductible type
In-network
Out-of-network
Individual
$750/$1,250 per year
$1,000/$1,750 per year
Family
$1,500/$2,500 per year
$2,000/$3,500 per year
Deductible waiver
There is no in-network deductible for the following covered services:
• Preventive care
• Family planning services – female contraceptives
• Pharmacy
Deductible and cost share waiver for risk reducing breast cancer prescription drugs
The per prescription cost share will not apply to risk reducing breast cancer prescription drugs when
obtained at a network pharmacy. This means they will be paid at 100%.
Deductible and cost share waiver for contraceptives (birth control)
The per prescription cost share will not apply to female contraceptive methods when obtained at a
network pharmacy. This means they will be paid at 100%. This includes certain OTC and generic
contraceptive prescription drugs and devices for each of the methods identified by the FDA. If a
generic prescription drug is not available, the brand-name prescription drug for that method will
be paid at 100%.
The prescription drug cost share will apply to prescription drugs that have a generic equivalent or
alternative available within the same therapeutic drug class obtained at a network pharmacy unless we
approve a medical exception. A therapeutic drug class is a group of drugs or medications that have a
similar or identical mode of action or are used for the treatment of the same or similar disease or
injury.

7
Cost share waiver for tobacco cessation prescription and OTC drugs
The per prescription cost share will not apply to the first two 90-day treatment programs for tobacco
cessation prescription and OTC drugs when obtained at a network retail pharmacy. This means
they will be paid at 100%, as long as filled with a prescription. Your per prescription cost share will
apply after those two programs have been exhausted.
Maximum out-of-pocket limit
Includes the deductible.
Maximum
out-of-
pocket type
In-network
Out-of-network
Individual
$3,250/$3,750 per year
$6,000/$6,750 per year
Family
$6,500/$7,500 per year
$12,000/$13,500 per year
General coverage provisions
This section explains the deductible, maximum out-of-pocket limit and limitations listed in this
schedule.
Deductible provisions
Covered services apply to the in-network and out-of-network deductibles
The deductible may not apply to some covered services. You still pay the copayment or payment
percentage, if any, for these covered services.
Individual deductible
You pay for covered services each year before the plan begins to pay. This individual deductible
applies separately to you and each covered dependent. After the amount paid reaches the individual
deductible, this plan starts to pay for covered services for the rest of the year.
Family deductible
You pay for covered services each year before the plan begins to pay. After the amount paid for
covered services reaches this family deductible, this plan starts to pay for covered services for the
rest of the year. To satisfy this family deductible for the rest of the year, the combined covered
services that you and each of your covered dependents incur toward the individual deductible must
reach this family deductible in a year. When this happens in a year, the individual deductibles for
you and your covered dependents are met for the rest of the year.
Deductible credit
If you paid part or all of your deductible under other coverage for the Calendar Year that this plan
went into effect, the deductible on this plan for that Calendar Year will be reduced by the amount you
paid under your prior coverage for new hires and employees of an acquired company only.
Copayment
This is a flat fee you pay for certain visits or covered services. A copay can be a dollar amount or
percentage. This is in addition to any out-of-pocket costs you have to pay to meet your deductible, if
you have one.
Per admission copayment
This is the amount you are required to pay when you or a covered dependent have a stay in an
inpatient facility.

8
Payment Percentage
The specific percentage the plan pays after you meet your deductible. This is in addition to any out-
of-pocket costs you have to pay to meet your deductible, if you have one.
Per admission cost share or deductible
A separate cost share or deductible may apply per facility. This is in addition to any other cost share
or deductible applicable under this plan. It may apply to each stay or on a per day basis up to a per
admission maximum amount. If you are in the same type of facility more than once, and your stays
are separated by less than 10 days (regardless of cause), only one per admission cost share or
deductible will apply. Not more than three per admission cost shares or deductibles will apply for a
facility type during the year. Covered services applied to the per admission deductible can’t be
applied to any other deductible required under the plan. Covered services applied to the plan’s other
deductible will not apply to the per admission deductible.
Maximum out-of-pocket limit
The maximum out-of-pocket limit is the most you will pay per year in copayments, payment
percentage and deductible, if any, for covered services. Covered services that are subject to the
maximum out-of-pocket limit include those provided under the medical plan and the outpatient
prescription drug plan.
Covered services apply to the in-network and out-of-network maximum out-of-pocket limit.
Individual maximum out-of-pocket limit
• This plan may have an individual and family maximum out-of-pocket limit. As to the
individual maximum out-of-pocket limit, each of you must meet your maximum out-of-
pocket limit separately.
• After you or your covered dependents meet the individual maximum out-of-pocket limit, this
plan will pay 100% of the eligible charge for covered services that would apply toward the
limit for the rest of the year for that person.
Family maximum out-of-pocket limit
After you or your covered dependents meet the family maximum out-of-pocket limit, this plan will
pay 100% of the eligible charge for covered services that would apply toward the limit for the
remainder of the year for all covered family members. The family maximum out-of-pocket limit is a
cumulative maximum out-of-pocket limit for all family members.
To satisfy this maximum out-of-pocket limit for the rest of the year, the following must happen:
• The family maximum out-of-pocket limit is met by a combination of family members
• No one person within a family will contribute more than the individual maximum out-of-pocket
limit amount in a year
If the maximum out-of-pocket limit does not apply to a covered service, your cost share for that
service will not count toward satisfying the maximum out-of-pocket limit amount.
Certain costs that you have do not apply toward the maximum out-of-pocket limit. These include:
• All costs for non-covered services which are identified in the booklet and the schedule
• Charges, expenses or costs in excess of the recognized charge
• Costs for non-emergency use of the emergency room
• Costs for non-urgent use of an urgent care provider
• Amounts received from a third-party copay assistance program, like a manufacturer coupon or
rebate, for a specialty prescription drug

9
Limit provisions
Covered services will apply to the in-network and out-of-network limits.
Your financial responsibility and decisions regarding benefits
We base your financial responsibility for the cost of covered services on when the service or supply
is provided, not when payment is made. Benefits will be pro-rated to account for treatment or portions
of stays that occur in more than one year. Decisions regarding when benefits are covered are subject
to the terms and conditions of the booklet.
Outpatient prescription drug maximum out-of-pocket limit provisions
Covered services that are subject to the maximum out-of-pocket limit include covered services
provided under the medical plan and the prescription drug plan.
The maximum out-of-pocket limit is the most you will pay per year in copayments, payment
percentage and deductible, if any, for covered services. This plan may have an individual and
family maximum out-of-pocket limit.
Covered services
Acupuncture
Description
In-network
Out-of-network
Acupuncture
85% per visit after deductible
75% per visit after deductible
Visit limit per year
10
10
Limit per visit
$80
$80
Ambulance services
Description
In-network
Out-of-network
Emergency services
80% per trip, no deductible applies
Paid same as in-network
Description
In-network
Out-of-network
Non-emergency
services
80% per trip, no deductible applies
80% per trip, no deductible applies
Applied behavior analysis
Description
In-network
Out-of-network
Applied behavior
analysis
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Autism spectrum disorder
Description
In-network
Out-of-network
Diagnosis and testing
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Treatment
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Occupational (OT),
physical (PT) and
speech (ST) therapy
for autism spectrum
disorder
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received

10
Behavioral health
Mental health disorders treatment
Coverage provided is the same as for any other illness
Description
In-network
Out-of-network
Inpatient services-
room and board
including residential
treatment facility
$120 then the plan pays 85% per
admission after deductible
$120 then the plan pays 75% per
admission after deductible
Description
In-network
Out-of-network
Outpatient office visit
to a physician or
behavioral health
provider
85% per visit after deductible
75% per visit after deductible
Physician or
behavioral health
provider
telemedicine
consultation
85% per visit after deductible
75% per visit after deductible
Outpatient mental
health disorders
telemedicine
cognitive therapy
consultations by a
physician or
behavioral health
provider
Covered based on type of service
and provider from which it is
received
Covered based on type of service
and provider from which it is
received
Description
In-network
Out-of-network
Other outpatient
services including:
• Behavioral health
services in the
home
• Partial
hospitalization
treatment
• Intensive
outpatient
program
The cost share doesn’t
apply to in-network
peer counseling
support services
100% per visit, no deductible
applies
75% per visit after deductible

11
Substance related disorders treatment
Includes detoxification, rehabilitation and residential treatment facility
Coverage provided is the same as for any other illness
Description
In-network
Out-of-network
Inpatient services-
room and board
during a hospital stay
$120 then the plan pays 85% per
admission after deductible
$120 then the plan pays 75% per
admission after deductible
Description
In-network
Out-of-network
Outpatient office visit
to a physician or
behavioral health
provider
85% per visit after deductible
75% per visit after deductible
Physician or
behavioral health
provider
telemedicine
consultation
85% per visit after deductible
75% per visit after deductible
Outpatient
telemedicine
cognitive therapy
consultations by a
physician or
behavioral health
provider
Covered based on type of service
and provider from which it is
received
Covered based on type of service
and provider from which it is
received
Description
In-network
Out-of-network
Other outpatient
services including:
• Behavioral health
services in the
home
• Partial
hospitalization
treatment
• Intensive
outpatient
program
The cost share doesn’t
apply to in-network
peer counseling
support services
100% per visit, no deductible
applies
75% per visit after deductible

12
Clinical trials
Description
In-network
Out-of-network
Experimental or
investigational
therapies
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Routine patient costs
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Diabetic services, supplies, equipment, and self-care programs
Description
In-network
Out-of-network
Diabetic services
Covered based on type of service
and where it is received
Covered based on type of service and
where it is received
Diabetic supplies
Covered based on type of service
and where it is received
Covered based on type of service and
where it is received
Diabetic equipment
Covered based on type of service
and where it is received
Covered based on type of service and
where it is received
Diabetic self-care
programs
Covered based on type of service
and where it is received
Covered based on type of service and
where it is received
Durable medical equipment (DME)
Description
In-network
Out-of-network
DME
85% per item after deductible
75% per item after deductible
(including wigs)
100% per item, no deductible
applies
100% per item, no deductible applies
Emergency services
Description
In-network
Out-of-network
Emergency room
$60 then the plan pays 85% per visit
after deductible
Paid same as in-network
Non-emergency care
in a hospital
emergency room
Not covered
Not covered
Emergency services important note:
• Out-of-network providers do not have a contract with us. The provider may not accept
payment of your cost share as payment in full. You may receive a bill for the difference between
the amount billed by the provider and the amount paid by the plan. If the provider bills you for
an amount above your cost share, you are not responsible for payment of that amount. You
should send the bill to the address on your ID card, and we will resolve any payment issue with
the provider. Make sure the member ID is on the bill.
• In the case of a surprise bill from an out-of-network provider, where you had no control of their
participation in your covered services, you will pay the same cost share you would have if the
covered services were received from a network provider. The cost share will be based on the
median contracted rate. Contact us immediately if you receive such a bill.
• If you are admitted to the hospital for an inpatient stay right after you visit the emergency room,
you will not pay your emergency room cost share if you have one. You will pay the inpatient
hospital cost share, if any.
13
Habilitation therapy services
Physical (PT), occupational (OT) therapies
Description
In-network
Out-of-network
PT, OT therapies
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Speech therapy (ST)
Description
In-network
Out-of-network
ST
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Home health care
A visit is a period of 4 hours or less
Description
In-network
Out-of-network
Home health care
85% per visit after deductible
75% per visit after deductible
Visit limit per year
200
60
Home health care important note:
Intermittent visits are periodic and recurring visits that skilled nurses make to ensure your proper
care. The intermittent requirement may be waived to allow for coverage for up to 12 hours with a daily
maximum of 3 visits.
Hospice care
Description
In-network
Out-of-network
Inpatient services -
room and board
85% after deductible
75% after deductible
Description
In-network
Out-of-network
Outpatient services
85% per visit after deductible
75% per visit after deductible
Limit per lifetime for
inpatient and
outpatient care
185
185
Hospice important note:
This includes part-time or infrequent nursing care by an R.N. or L.P.N. to care for you up to 8 hours a
day. It also includes part-time or infrequent home health aide services to care for you up to 8 hours a
day.
Hospital care
Description
In-network
Out-of-network
Inpatient services –
room and board
$120 then the plan pays 85% per
admission after deductible
$120 then the plan pays 75% per
admission after deductible
Infertility services
Basic infertility
Description
In-network
Out-of-network
Treatment of basic
infertility
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received

14
Comprehensive infertility services
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Advanced reproductive technology (ART)
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Limits
Description
In-network
Out-of-network
Limit per lifetime ART
and Comprehensive
services combined
$10,000 (Limit doesn’t include
covered pharmacy expenses)
Combined for in-network and out-of-
network benefits
$10,000 (Limit doesn’t include
covered pharmacy expenses)
Combined for in-network and out-of-
network benefits
Maternity and related newborn care
Includes complications
Description
In-network
Out-of-network
Inpatient services –
room and board
$120 then the plan pays 85% per
admission after deductible
$120 then the plan pays 75% per
admission after deductible
Services performed in
physician or
specialist office or a
facility
85% per visit after deductible
75% per visit after deductible
Other services and
supplies
85% after deductible
75% after deductible
Maternity and related newborn care important note:
Any cost share collected applies only to the delivery and postpartum care services provided by an
OB, GYN or OB/GYN. Review the Maternity section of the certificate. It will give you more information
about coverage for maternity care under this plan.
Oral and maxillofacial treatment (mouth, jaws and teeth)
Description
In-network
Out-of-network
Treatment of mouth,
jaws and teeth
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
15
Outpatient prescription drugs
Generic prescription drugs
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$13, no deductible applies
$13 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$26, no deductible applies
$26 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$39, no deductible applies
$39 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$39, no deductible applies
Not covered
Preferred brand-name prescription drugs
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$35, no deductible applies
$35 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$70, no deductible applies
$70 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$105, no deductible applies
$105 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$105, no deductible applies
Not covered

16
Non-preferred brand-name prescription drugs
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$60, no deductible applies
$60 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$120, no deductible applies
$120 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$180, no deductible applies
$180 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$180, no deductible applies
Not covered
Brand-name specialty prescription drugs
Description
In-network
Out-of-network
Up to a 30-day supply
at a specialty
pharmacy or a retail
pharmacy
$120, no deductible applies
Not covered
Important note:
Your cost share for specialty prescription drugs, under the copayment assistance program, will
not count toward your deductible or maximum out-of-pocket limit. This includes cost shares that
you, the plan or the program pay.
Contraceptives (birth control)
Brand-name prescription drugs and devices are covered at 100% when a generic is not available
Description
In-network
Out-of-network
30-day supply or 12-
month supply of
generic and OTC
drugs and devices
$0, no deductible applies
Paid based on the tier of drug in the
schedule
30-day supply or 12-
month supply of
brand-name
prescription drugs
and devices
Paid based on the tier of drug in the
schedule
Paid based on the tier of drug in the
schedule

17
Generic diabetic supplies
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$0, no deductible applies
$0 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$0, no deductible applies
$0 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$0, no deductible applies
$0 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$0, no deductible applies
Not covered
Preferred brand-name diabetic supplies
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$5, no deductible applies
$5 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$10, no deductible applies
$10 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$15, no deductible applies
$15 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$15, no deductible applies
Not covered

18
Non-preferred brand-name diabetic supplies
Description
In-network
Out-of-network
Up to a 31-day supply
at a retail pharmacy
and an Extended Day
Supply (EDS) retail
pharmacy
$60, no deductible applies
$60 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
61-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$120, no deductible applies
$120 then the plan pays 50%, no
deductible applies
More than a 60-day
supply but less than a
91-day supply at an
Extended Day
Supply (EDS) retail
pharmacy
$180, no deductible applies
$180 then the plan pays 50%, no
deductible applies
More than a 31-day
supply but less than a
91-day supply at a
mail order pharmacy
$180, no deductible applies
Not covered
Maintenance Choice Opt-Out Program
Plan members will only be allowed to fill maintenance medications (90-day supply) at CVS mail order
or CVS retail locations. If plan members wish to opt out and continue or start using non-CVS locations
for a 30-day supply of maintenance medications, they must call Aetna at 1-888-792-3862.
Description
In-network
Out-of-network
Preventive care drugs
and supplements
$0, no deductible applies
Paid based on the tier of drug in the
schedule
Limits
Subject to any sex, age, medical
condition, family history and
frequency guidelines as
recommended by the U.S.
Preventive Services Task Force
(USPSTF)
For a current list of covered
preventive care drugs and
supplements or more information,
see the Contact us section
Subject to any sex, age, medical
condition, family history and
frequency guidelines as
recommended by the U.S.
Preventive Services Task Force
(USPSTF)
For a current list of covered
preventive care drugs and
supplements or more information,
see the Contact us section
Risk reducing breast cancer drugs
Description
In-network
Out-of-network
Risk reducing breast
cancer prescription
drugs
$0, no deductible applies
Paid based on the tier of drug in the
schedule
19
Limits
Subject to any sex, age, medical
condition, family history and
frequency guidelines as
recommended by the U.S.
Preventive Services Task Force
(USPSTF)
For a current list of risk reducing
breast cancer drugs or more
information, see the Contact us
section
Subject to any sex, age, medical
condition, family history and
frequency guidelines as
recommended by the U.S.
Preventive Services Task Force
(USPSTF)
For a current list of risk reducing
breast cancer drugs or more
information, see the Contact us
section

20
Tobacco cessation drugs
Description
In-network
Out-of-network
Tobacco cessation
prescription and OTC
drugs
$0, no deductible applies
Paid based on the tier of drug in the
schedule
Limits
Subject to any sex, age, medical
condition, family history and
frequency guidelines in the
recommendations of the USPSTF.
For a current list of covered tobacco
cessation drugs or more information,
see the Contact us section. See the
Other services section of this
schedule for more information.
Subject to any sex, age, medical
condition, family history and
frequency guidelines in the
recommendations of the USPSTF.
For a current list of covered tobacco
cessation drugs or more information,
see the Contact us section. See the
Other services section of this
schedule for more information.
Outpatient surgery
Description
In-network
Out-of-network
At hospital outpatient
department
85% per visit after deductible
75% per visit after deductible
Physician and specialist services
Physician services-general or family practitioner
Description
In-network
Out-of-network
Physician office hours
(not-surgical, not
preventive)
85% per visit after deductible
75% per visit after deductible
Physician surgical
services
85% per visit after deductible
75% per visit after deductible
Description
In-network
Out-of-network
Physician
telemedicine
consultation
85% per visit after deductible
75% per visit after deductible
Description
In-network
Out-of-network
Physician visit during
inpatient stay
85% per visit after deductible
75% per visit after deductible
Specialist
Description
In-network
Out-of-network
Specialist office hours
(not-surgical, not
preventive)
85% per visit after deductible
75% per visit after deductible
Specialist surgical
services
85% per visit after deductible
75% per visit after deductible

21
Description
In-network
Out-of-network
Specialist
telemedicine
consultation
85% per visit after deductible
75% per visit after deductible
All other services not shown above
Description
In-network
Out-of-network
All other services
85% per visit after deductible
75% per visit after deductible
Preventive care
Description
In-network
Out-of-network
Preventive care
services
100% per visit, no deductible
applies
75% per visit after deductible
Breast feeding
counseling and
support
100% per visit, no deductible
applies
75% per visit after deductible
Breast feeding
counseling and
support limit
6 visits in a group or individual
setting
Visits that exceed the limit are
covered under the physician
services office visit
6 visits in a group or individual
setting
Visits that exceed the limit are
covered under the physician
services office visit
Breast pump,
accessories and
supplies limit
Electric pump: 1 every 1 year
Manual pump: 1 per pregnancy
Pump supplies and accessories: 1
purchase per pregnancy if not
eligible to purchase a new pump
Electric pump: 1 every 1 year
Manual pump: 1 per pregnancy
Pump supplies and accessories: 1
purchase per pregnancy if not
eligible to purchase a new pump
Breast pump waiting
period
Electric pump: 1 year to replace an
existing electric pump
Electric pump: 1 year to replace an
existing electric pump
Counseling for alcohol
or drug misuse
100% per visit, no deductible
applies
75% per visit after deductible
Counseling for alcohol
or drug misuse visit
limit
5 visits/12 months
5 visits/12 months
Counseling for
obesity, healthy diet
100% per visit, no deductible
applies
75% per visit after deductible
Counseling for
obesity, healthy diet
visit limit
Age 22 and older: 26 visits per 12
months, of which up to 10 visits may
be used for healthy diet counseling.
Age 22 and older: 26 visits per 12
months, of which up to 10 visits may
be used for healthy diet counseling.
Counseling for
sexually transmitted
infection
100% per visit, no deductible
applies
75% per visit after deductible
Counseling for
sexually transmitted
infection visit limit
2 visits/12 months
2 visits/12 months
Counseling for
tobacco cessation
100% per visit, no deductible
applies
75% per visit after deductible

22
Counseling for
tobacco cessation visit
limit
8 visits/12 months
8 visits/12 months
Family planning
services (female
contraception
counseling)
100% per visit, no deductible
applies
75% per visit after deductible
Family planning
services (female
contraception
counseling) limit
Contraceptive counseling limited to 2
visits/12 months in a group or
individual setting
Contraceptive counseling limited to 2
visits/12 months in a group or
individual setting
Immunizations
100%, no deductible applies
75% after deductible
Immunization limit
Subject to any age limits provided for
in the comprehensive guidelines
supported by the Advisory
Committee on Immunization
Practices of the Centers for Disease
Control and Prevention
For details, contact your physician
Subject to any age limits provided for
in the comprehensive guidelines
supported by the Advisory
Committee on Immunization
Practices of the Centers for Disease
Control and Prevention
For details, contact your physician
Routine cancer
screenings
100% per visit, no deductible
applies
75% per visit after deductible
Routine cancer
screening limits
Subject to any age, family history
and frequency guidelines as set forth
in the most current:
Evidence-based items that have a
rating of A or B in the current
recommendations of the USPSTF
The comprehensive guidelines
supported by the Health Resources
and Services Administration
For more information contact your
physician or see the Contact us
section
Subject to any age, family history
and frequency guidelines as set forth
in the most current:
Evidence-based items that have a
rating of A or B in the current
recommendations of the USPSTF
The comprehensive guidelines
supported by the Health Resources
and Services Administration
For more information contact your
physician or see the Contact us
section
Lung cancer screening
100% per visit, no deductible
applies
75% per visit after deductible
Routine lung cancer
screening limit
1 screenings every 12 months
Screenings that exceed this limit
covered as outpatient diagnostic
testing
1 screenings every 12 months
Screenings that exceed this limit
covered as outpatient diagnostic
testing
Routine physical exam
100% per visit, no deductible
applies
75% per visit after deductible
Routine physical exam
limits
Subject to any age and visit limits
provided for in the comprehensive
guidelines supported by the
American Academy of
Pediatrics/Bright Futures/Health
Resources and Services
Subject to any age and visit limits
provided for in the comprehensive
guidelines supported by the
American Academy of
Pediatrics/Bright Futures/Health
Resources and Services

23
Administration for children and
adolescents
Limited to 7 exams from age 0-1
year; 3 exams every 12 months age
1-2; 3 exams every 12 months age
2-3; and 1 exam every year after that
age, up to age 22; 1 exam every
year after age 22
Administration for children and
adolescents
Limited to 7 exams from age 0-1
year; 3 exams every 12 months age
1-2; 3 exams every 12 months age
2-3; and 1 exam every year after that
age, up to age 22; 1 exam every
year after age 22
Well woman GYN
exam
100% per visit, no deductible
applies
75% per visit after deductible
Well woman GYN
exam limit
Subject to any age and visit limits
provided for in the comprehensive
guidelines supported by the Health
Resources and Services
Administration
Subject to any age and visit limits
provided for in the comprehensive
guidelines supported by the Health
Resources and Services
Administration
Limit
1 exam per year
1 exam per year
Private duty nursing
Up to eight hours equals one shift
Description
In-network
Out-of-network
Outpatient services
85% per visit after deductible
75% per visit after deductible
Visit/shift limit per year
60
60
Prosthetic Devices
Description
In-network
Out-of-network
Prosthetic devices
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Reconstructive surgery and supplies
Including breast surgery
Description
In-network
Out-of-network
Surgery and supplies
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received

24
Routine cancer screenings
Description
In-network
Out-of-network
Colonoscopy
100% per visit, no deductible
applies
75% per visit after deductible
Colonoscopy limit
Once every five years
Once every five years
Digital rectal
examination (DRE)
100% per visit, no deductible
applies
75% per visit after deductible
Digital rectal
examination (DRE)
limit
Covered for males age 40 and over
Covered for males age 40 and over
Double contrast barium
enemas (DCBE)
100% per visit, no deductible
applies
75% per visit after deductible
Double contrast barium
enemas (DCBE) limit
Once every five years
Once every five years
Fecal occult blood test
(FOBT)
100% per visit, no deductible
applies
75% per visit after deductible
Fecal occult blood test
(FOBT) limit
Covered age 40 and over
Covered age 40 and over
Mammogram
100% per visit, no deductible
applies
75% per visit after deductible
Mammogram limits
One per year for covered females
One per year for covered females
Prostate specific
antigen (PSA) test
100% per visit, no deductible
applies
75% per visit after deductible
Sigmoidoscopy
100% per visit, no deductible
applies
75% per visit after deductible
Sigmoidoscopy limit
Once every five years
Once every five years

25
Short-term rehabilitation services
Cardiac rehabilitation
Description
In-network
Out-of-network
Cardiac rehabilitation
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Pulmonary rehabilitation
Description
In-network
Out-of-network
Pulmonary
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Cognitive rehabilitation
Description
In-network
Out-of-network
Cognitive rehabilitation
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Physical and occupational therapies
Description
In-network
Out-of-network
At the physician
office
85% per visit after deductible
75% per visit after deductible
Speech therapy (ST)
Description
In-network
Out-of-network
At the physician
office
85% per visit after deductible
75% per visit after deductible
Physical and occupational therapies
Description
In-network
Out-of-network
Visit limit per year
60
60
Speech therapy (ST)
Description
In-network
Out-of-network
Visit limit per year
30
30
Spinal manipulation
Description
In-network
Out-of-network
At the physician
office
85% per visit after deductible
75% per visit after deductible
Visit limit per year
30
30
Skilled nursing facility
Description
In-network
Out-of-network
Inpatient services -
room and board
$120 then the plan pays 85% per
admission after deductible
$120 then the plan pays 75% per
admission after deductible
Other inpatient
services and supplies
85% per admission after deductible
75% per admission after deductible
Day limit per year
100
100

26
Tests, images and labs – outpatient
Diagnostic complex imaging services
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Diagnostic lab work
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Diagnostic x-ray and other radiological services
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Therapies
Chemotherapy
Description
In-network
Out-of-network
Chemotherapy
services
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Gene-based, cellular and other innovative therapies (GCIT)
Description
In-network (GCIT-designated
facility/provider)
Out-of-network
(Including providers who are
otherwise part of Aetna’s network
but are not GCIT-designated
facilities/providers)
Services and supplies
Covered based on type of service
and where it is received
Not covered
Gene therapy
products,
prescription drugs
85% per visit after deductible
Not covered

27
Infusion therapy
Outpatient services
Description
In-network
Out-of-network
85% per visit after deductible
75% per visit after deductible
Radiation therapy
Description
In-network
Out-of-network
Radiation therapy
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Respiratory therapy
Description
In-network
Out-of-network
Respiratory therapy
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Transplant services
Description
In-network (IOE facility)
Out-of-network
(Includes providers who are
otherwise part of Aetna’s network but
are non-IOE providers)
Inpatient services and
supplies
$120 then the plan pays 85% per
transplant after deductible
$120 then the plan pays 75% per
transplant after deductible
Physician services
Covered based on type of service
and where it is received
Covered based on type of service
and where it is received
Urgent care services
At a freestanding facility or provider that is not a hospital
A separate urgent care cost share will apply for each visit to an urgent care facility or provider
Description
In-network
Out-of- network
Urgent care facility
85% per visit after deductible
75% per visit after deductible
Non-urgent use of an
urgent care facility or
provider
Not covered
Not covered
Walk-in clinic
Not all preventive care services are available at a walk-in clinic. All services are available from a
network physician.
Description
Designated network
Non-designated
network
Out-of-network
Non-emergency
services
100% per visit, no
deductible applies
85% per visit after
deductible
75% per visit after
deductible
Preventive care
immunizations
100% per visit, no
deductible applies
100% per visit, no
deductible applies
75% per visit after
deductible
Immunization limits
Subject to any age and
frequency limits
provided for in the
comprehensive
guidelines supported
by the Advisory
Committee on
Immunization Practices
of the Centers for
Subject to any age and
frequency limits
provided for in the
comprehensive
guidelines supported by
the Advisory Committee
on Immunization
Practices of the Centers
Subject to any age and
frequency limits
provided for in the
comprehensive
guidelines supported
by the Advisory
Committee on
Immunization Practices
of the Centers for

28
Disease Control and
Prevention
For details, contact
your physician
for Disease Control and
Prevention
For details, contact your
physician
Disease Control and
Prevention
For details, contact
your physician
Preventive screening
and counseling
services
100% per visit, no
deductible applies
100% per visit, no
deductible applies
75% per visit after
deductible
Preventive screening
and counseling limits
See the Preventive
care services section of
the schedule
See the Preventive care
services section of the
schedule
See the Preventive
care services section of
the schedule
Important Note:
Key terms
Designated network provider
A network provider listed in the directory under Best Results for your plan as a provider for your
plan.
Non-designated network provider
A provider listed in the directory under the All other results tab as a provider for your plan.
See the Contact us section if you have questions.
You will pay less cost share when you use a designated network walk-in clinic provider. Non-
designated network walk-in clinic providers are available to you, but the cost share will be at a
higher level when these providers are used.
Health Premiums Per Pay Period (Before Tax)
Health Coverage
You Pay
(Per Pay Period)
$750 Individual/$1,500 Family Deductible PPO Health Option
Employee Only
$103.00
Employee + One
$206.00
Employee + Family
$296.00
$1,250 Individual/$2,500 Family Deductible PPO Health Option
Employee Only
$52.00
Employee + One
$110.00
Employee + Family
$181.00
Dental Options and Coverage Details
Waive Dental Coverage
Waiving dental coverage means that you are not electing dental coverage through the Group Dental
Plan. Perhaps you are covered under a spouse’s dental plan. Compare your options, look at dentists

29
in the network, premiums and/or differences in coverage in order to determine the best option for you
and your family.
Many plans, including those offered to Mutual of Omaha employees, have a Coordination of Benefits
plan provision. With Coordination of Benefits plan provisions, one plan will pay its full benefits first,
then the other plan may only pay up to the amount what would have paid had it been the primary plan.
You may find you are paying premium for two plans, but not receiving the anticipated benefits of both
at the same time.
If you waive health coverage and experience a Life Event, such as a loss of other group coverage, you
may enroll in our plan by contacting us within 31 days of the Life Event.
Dental
Our Group Dental Plan covers preventive, basic services, major services and orthodontics. The Plan
Administrator for the Group Dental Plan is Mutual of Omaha Workplace Solutions. The plan balances
savings, service and customer satisfaction by providing access to the nationwide Mutually Preferred
dental network.
When using in-network Mutually Preferred providers, you reduce your out-of-pocket dental care
expenses because providers have agreed upon certain rates for their services, deductibles are lower
and the plan pays a larger percentage of the expenses. If you choose out-of-network providers, you
will have higher out of pocket costs because the deductibles are higher, and the plan pays a smaller
percentage of the expenses.
In-network providers can be found online or by contacting Customer Service at 800-927-9197. This
website and contact number for customer services is referenced on the last page of this guide and is
available on the ID card you’ll receive after enrolling in the plan.
Dental Deductibles
All benefits are subject to a calendar year deductible, except for preventive care in-network benefits. A
deductible is the amount of covered expenses that you must pay before the plan starts paying
benefits. Below are the calendar year dental deductibles:
In-network Out-of-network
$25 per person, $50 per family $75 per person, $150 per family
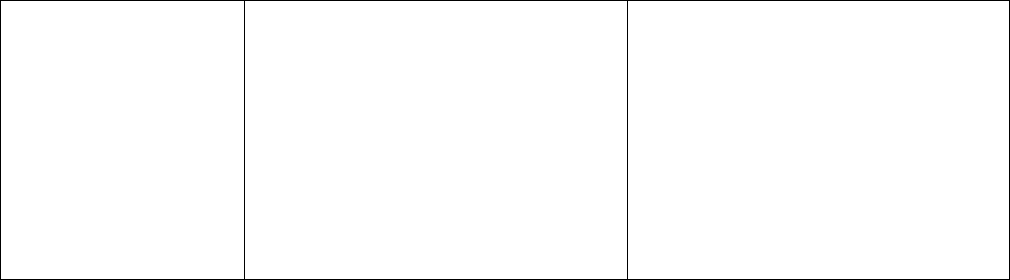
Dental Coverage
Covered Services Examples In-Network Providers
Out-of-Network
Providers
Class I Cleanings & X-rays** 100%
100% of maximum
allowance for out of
network covered services
Class II
Prefabricated Crowns,
Root Canals & Fillings
80% after calendar year
deductible
60% of maximum
allowance for out of
network covered services
Class III
Cast Restoration Crowns,
Dentures & Bridgework,
Dental Implants
60% after calendar year
deductible
50% of maximum
allowance for out of
network covered services

30
Orthodontics Braces
60% after calendar year
deductible
50% of maximum
allowance for out of
network covered services
Annual Maximum
$1,500 per person $1,500
Orthodontics Lifetime
Maximum
$1,500 per person $1,500
For detailed information on covered services, see the Summary Plan Description.
**Two dental cleanings are covered per calendar year for each covered person. Four dental cleanings
are provided per calendar year for any covered person who is pregnant, has diabetes or heart
disease.
Predetermination of Benefits
If you anticipate a dental expense is going to be over $300, we recommend you have your dentist
submit a dental Predetermination of Benefits form (Dental Claim Form), in advance, to confirm what
benefits will be payable. If available, less expensive alternative treatment plans will be presented.
For more information on your dental benefits, click here
.
Dental Premiums Per Pay Period (Before Tax)
Dental Coverage You Pay (Per Pay Period)
Dental
Employee Only
$5.00
Employee + One
$11.50
Employee + Family
$21.00
Vision Option and Coverage Details
EyeMed Vision Benefits
Mutual of Omaha offers you the ability to elect vision coverage through EyeMed Vision Care. This plan
provides vision care services such as eye exams and coverage options for glasses or contacts.
To search for an EyeMed Network participating providers, reference the last page of this
guide.
EyeMed coverage provides the following benefits, discounts and savings when utilizing a
participating provider:
Well Vision Exam: $25 copay every calendar year
Frame: $0 Copay, $150 allowance, covered once every other calendar year
Lenses: Covered every calendar year

31
$25 Copay for Single vision, bifocal, trifocal, lenticular and progressive standard lenses.
$0 Copay for Anti Reflective Coating-Standard, Scratch Coating-Standard Plastic and
Polycarbonate-Standard lenses for dependent children
Discounts and/or copayments on other lens options, including progressive lenses
Contact Lens: up to $40 copay for contact lens standard exam (fitting and evaluation)
$200 allowance toward the cost of contacts, if not electing glasses.
Covered every calendar year
For more information on your vision benefits, click here
.
EyeMed Premiums Per Pay Period (Before Tax)
EyeMed Vision Coverage
You Pay (Per Pay Period)
Vision
Employee Only
$4.82
Employee + One $6.91
Employee + Family $12.37
Health Care Flexible Spending Account
Advantages of a Health Care Flexible Spending Account (FSA)
The Health Care FSA allows you to set aside pre-tax dollars to reimburse you for eligible out of pocket
health, prescription drug, dental, and vision expenses. You may use this account for yourself and any
tax dependent. You can be reimbursed up to your annual pledge for eligible expenses you’ve incurred
during your benefits eligibility period, even before you’ve had that amount withheld from your
paychecks.
The Health Care FSA reduces your taxable income because your contributions are deposited in the
FSA on a pre-tax basis. This means that your contribution is deducted from your paycheck before
taxes are withheld. For example, if your income was $30,000 and your out-of-pocket expenses totaled
$540 and you had $45 a month deducted from your paycheck before taxes, you could save $122 in
taxes over the course of the year, because your taxable income would be reduced.
Mutual of Omaha’s Health Care Flexible Spending Account does not cover over the counter expenses,
even if prescribed by a physician, nor is prescribed marijuana a covered expense. We also don’t
cover taxes and shipping charges.
Contribution Amounts
Minimum – $60 per year
Maximum – $3,050 per year
Eligible Expenses for Reimbursement
Your FSA can help you pay for expenses that are predictable. Consider the following types of
expenses:

32
•
Health/dental out of pocket expenses
•
Deductibles
•
Coinsurance/ Copayments
•
Prescriptions
•
Expenses not covered by the plans or over plan maximums
•
Vision/hearing expenses
•
Lasik surgery to correct vision (make certain you are a candidate before enrolling in the FSA)
Setting Up Your Health Care Flexible Spending Account
Estimate how much money you will need to cover eligible expenses for yourself and your tax
dependents for the period from your benefit effective date to the end of the year. We will automatically
divide your total contribution amount evenly across your eligible paychecks. Each year during the
annual enrollment period, you will have the opportunity to re-enroll in the Health Care Flexible
Spending Account.
Important Internal Revenue Service (IRS) Requirements
• Money contributed to Flexible Spending Accounts must be used for eligible expenses incurred
during the year that it is taken from your pay. Following the reimbursement period for the year,
up to $500 of the remaining balance will be rolled over to the next year. Any remaining balance
over $500 will be forfeited.
• Eligible expenses must be incurred after the date your plan participation begins.
• Money cannot be transferred between the Health Care Flexible Spending Account and the
Dependent Care Flexible Spending Account.
• The amount paid out will be equal to the annual pledge anytime during the calendar year.
• If you or your dependents are enrolled in a health savings account through another plan,
participation in a Health Care FSA could jeopardize the ability for you or your dependents to
make contributions to the health savings account. Please contact your tax advisor for
additional information.
Submitting the Claim
Claims submitted by Monday at Noon (CST) are processed the same week. Reimbursements are
directly deposited into your existing payroll deposit account on Fridays after the claim has been
processed.
Please note, after December 31, 2024, you will have until March 31, 2025, to submit reimbursement
claims for health care expenses incurred during 2024. After this date, remaining balances up to $500
will be available for reimbursement.
Reimbursement Methods
Online Expense Reimbursement
If you are enrolled on our health, dental and/or vision plans, your reimbursement claim can be
submitted online by signing on to PeopleSoft, click on the Benefits Tile, Benefits Summary tile and
then scroll down to Health Care Reimb and click on Review. You will receive email notification alerting
you of eligible claims that have been loaded every Tuesday, that are eligible for reimbursement.
Instructions on how to submit a Health Care claim online
.

33
Paper Expense Reimbursement
Eligible expenses that are not processed through our online system will need to be submitted on a
paper claim form. These expenses may include:
•
Vision, if not covered under EyeMed
•
Lasik surgery
•
Routine hearing exams and hearing aids
•
Covered out-of-pocket health, dental, vision and prescription drug expenses
incurred while you or your eligible dependents were covered under another health,
dental or vision plan.
Paper claim forms and supporting documentation are submitted to the Benefits Department for
.
You have until March 31, 2025, to submit reimbursement claims for health care expenses incurred
during 2024.
For more information on the Health Care Flexible Spending Account (FSA) and for a paper claim form,
click here
.
Dependent Care Flexible Spending Account
Advantages of a Dependent Care Flexible Spending Account (FSA)
The Dependent Care FSA allows you to set aside before-tax dollars to pay eligible dependent care
expenses. The Dependent Care FSA reduces your taxable income because your contributions are
deposited in the FSA on a pre-tax basis. Pre-tax basis means that your contribution is deducted from
your paycheck before taxes are withheld. Consult your tax advisor to determine if participating in the
dependent care account would be to your advantage based on your combined household income and
financial situation.
Contribution Amounts
If both you and your spouse work or you are a single parent, you can contribute to the dependent care
account. The maximum listed is a combined amount for you and your spouse. This is an IRS limit so
you need to make sure you don’t exceed it, if you have been contributing to a Dependent Care
Flexible Spending Account through another employer.
Minimum – $60 per year
Maximum – $5,000 per year
Eligible Expenses
• Dependent Day Care expenses for an eligible dependent incurred while you are at work
Eligible expenses cannot exceed your spouse’s earnings, unless your spouse is a full-time student or
is disabled. If your spouse is a full-time student or disabled, their earnings are considered to be $200 a
month or $400 a month if two or more dependents are receiving care.

34
Eligible Dependents
An eligible dependent is someone you claim as a dependent on your tax return. The dependent must
be under age 13 or a mentally or physically disabled spouse or dependent who lives in your home and
is unable to care for himself or herself.
Setting Up Your Dependent Care Flexible Spending Account
Estimate how much money you will need to cover your expenses for the rest of this year to determine
your annual contribution amount. Remember vacation and school breaks (including the summer
months). When you incur an eligible expense, you pay the expense, and then you get reimbursed up
to the amount of money you have in your Dependent Care FSA.
Each year during annual enrollment period, as required by law, you will have the opportunity to re-
enroll in the Dependent Care Flexible Spending Account.
Important Internal Revenue Service (IRS) Requirements
• Money contributed to Flexible Spending Accounts must be used for eligible expenses incurred
during the year that it is taken from your pay or it will be forfeited.
• Eligible expenses must be incurred after the date your plan participation begins.
• Money cannot be transferred between the Health Care Flexible Spending Account and the
Dependent Care Flexible Spending Account.
• Expenses paid out are limited by the amount you contribute anytime during the year.
Reimbursement Method
Once you incur and pay the expense, submit the expense and a claim form to the Benefits Department
by e-mailing them to the Benef[email protected]
. If you are attaching a receipt with
your claim form, remember a canceled check cannot be accepted as a receipt.
Submitting the Claim
Claims submitted by Monday at Noon (CST) are processed the same week. Reimbursements are
directly deposited into your existing payroll deposit account on Fridays after the claim has been
processed. You have until March 31, 2025, to submit reimbursement claims for dependent care
expenses incurred during 2024.
For more information on the Dependent Care Flexible Spending Account (FSA) and for a paper claim
form, click here
.
Life and Loss Benefits
Life insurance is protection for those who you’ll leave behind. It pays a benefit at the
time of death that can help with final planning and loss of future income.

35
The Employee, Spouse and Child Life options are term life products. The premiums are paid on an
after-tax basis. As a new hire, you may elect any level of coverage without needing to provide proof of
good health. After your new hire enrollment, life restriction rules apply, meaning you will only be able
to move up one level at annual enrollment, or qualified Life Event, without proof of good health at your
own expense.
Basic Employee Life Benefits
• At no cost to you, the company provides a basic life insurance benefit equal to one times your
Annual Benefits Salary.
• This coverage is effective on your first day of employment.
• You will be asked to identify a beneficiary.
• Premiums for coverage exceeding $50,000 (basic benefit only) are considered taxable income.
As a new hire, your Annual Benefits Salary is equivalent to your annual salary, plus any transitional
salary arrangement for production sales employees. Each year, Mutual of Omaha will calculate a new
Annual Benefits Salary for the upcoming calendar year based on your salary as of August 31, plus
your eligible earnings in the 12 months preceding that date. You may reference the
Summary Plan
Description for a more detailed description.
Employee Supplemental Life Options
• As a new hire, you may elect to purchase increments of 1, 2, 3 or 4 times your Annual Benefit
Salary without needing to provide proof of good health.
• The maximum amount of employee group life insurance cannot be greater than $750,000
(Basic and Supplemental Life combined).
Employee Supplemental Life Costs
• Premiums are based on your age as of Aug 31 preceding your hire date. The amount of your
coverage will not change during the year, even if your monthly pay changes.
• Your rates will be visible when you are completing your enrollment.
• For reference, you can calculate your premiums using the premiums on the next page.
Employee Age
As of Benefits Start Date
Monthly Rate per $1,000 of Coverage
Under 30
$ .05
30-34
$ .07
35-39
$ .09
40-44
$ .10
45-49
$ .15
50-54
$ .23
55-59
$ .43
60-64
$ .53
65-69
$ .93
Over 70
$ .98

36
Spouse Life Options
You may purchase the following amounts of life insurance:
• $10,000
• $25,000
• $50,000
• $75,000
The amount of life insurance for your spouse cannot be greater than the total amount of group life
insurance carried on you, including basic and supplemental coverage.
Spouse Life Costs
Per Pay Period Premium Based on Coverage Level Elected:
Spouse's Age $10,000 $25,000 $50,000 $75,000
Younger than 40
$0.80
$2.00
$4.00
$6.00
40-44
$1.00
$2.50
$5.00
$7.50
45-49
$2.00
$5.00
$10.00
$15.00
50-54
$3.00
$7.50
$15.00
$22.50
55-59
$4.50
$11.25
$22.50
$33.75
60-64
$6.00
$15.00
$30.00
$45.00
65 and older
$13.50
$33.75
$67.50
$101.25
Child Life Options and Premiums
You may purchase the following amounts of life insurance for your eligible children whom are at least
14 days old. Children may be covered through the end of the month in which they turn 26.
One premium will cover all eligible children. Below are the per pay period after tax premiums based on
coverage level elected:
Coverage
Per Pay Period
$10,000
$0.35
$15,000
$0.70
$20,000
$1.40
Accidental Death & Dismemberment Insurance (AD&D)
Accidental Death and Dismemberment benefits will be paid if you die, become dismembered or
paralyzed as a result of an accident. This is a separate benefit from Life Insurance. An accident is
defined as a sudden and unexpected event in which you or your dependent is injured, and the injury is
not due to a disease or sickness. This benefit can help offer financial protection for those who depend
on you.

37
Basic AD&D Benefits
The company provides $25,000 of employee AD&D coverage at no cost to you.
Supplemental AD&D Options
• You may purchase additional Supplemental AD&D benefits for yourself and your eligible
dependents from $50,000 to $250,000 in $50,000 increments.
• If you enroll in family coverage, coverage for spouse or children is as follows:
Employee
Spouse (40%)
Children (10%)
$50,000
$20,000
$5,000
$100,000
$40,000
$10,000
$150,000
$60,000
$15,000
$200,000
$80,000
$20,000
$250,000
$100,000
$25,000
Supplemental AD&D Costs
Below are the per pay period after tax premiums for the following options you may purchase:
Employee
Only
Employee + One or
Employee
$50,000
$ .75
$1.00
$100,000
$1.50
$2.00
$150,000
$2.25
$3.00
$200,000
$3.00
$4.00
$250,000
$3.75
$5.00
Click here for more information on Life benefits. Click here for more information on AD&D benefits.
Income Protection Benefits
Short-Term disability and Long-Term Disability help protect your income and future. If you couldn’t
work for an extended period, how long could you and/or your family keep your lifestyle? Short-Term
disability replaces part of your income if you’re unable to work due to childbirth, illness or injury. Long-
Term Disability helps cover your day-to-day living expenses when you’re not able to work for an
extended time due to an illness or injury. Both benefits support you through non-work-related illness
or injuries.
Short-Term Disability Benefits
The Short-Term Disability (“STD”) Plan provides short-term income replacement benefits for eligible
employees who are determined by the Health Services Department to have an absence due to an
illness and are unable to perform the duties of their assigned jobs.
If you are experiencing or anticipating a short-term disability, you will be assigned a case manager

38
from Health Services to assist you with this benefit.
Eligibility – Employees are eligible for STD coverage following 12 months of continuous employment.
Amount of Benefit for Eligible Employees – In the event of an eligible absence, you will receive
70% of base pay after meeting the 5-day waiting period.
Maximum Benefit Period – Up to 125 days in a rolling 12-month time period, which includes holidays.
This period can be used to fill the waiting period for Long-Term Disability. This does include how STD
is calculated for employees who have variable pay.
For more information on Short-Term benefits, click here.
Basic Long-Term Disability Benefits
Long-Term Disability benefits replace a portion of your pay if you become disabled and are unable
to work.
• At no cost to you, the company provides basic monthly pay replacement of 60% of your Annual
Benefit Salary (not to exceed a maximum monthly benefit of $10,000)
• There is a six-month period before benefits are payable
As a new hire, your Annual Benefits Salary is equivalent to your annual salary, plus any transitional
salary arrangement for production sales employees. Each year, Mutual of Omaha will calculate a new
Annual Benefits Salary for the upcoming calendar year based on your salary as of August 31, plus
your eligible earnings in the 12 months preceding that date. You may reference the
Summary Plan
Description for a more detailed description.
Long-Term Disability Supplemental Options and Costs
• You may purchase an additional 10% of supplemental LTD coverage for a total monthly pay
replacement of 70% of your Annual Benefit Salary (not to exceed a maximum monthly benefit
of $20,000)
• If you elect the additional 10% of coverage, your portion of the cost will be paid with before tax
dollars from your pay.
• The premium rates will be visible on your enrollment. The pay period rate is equal to your
monthly Annual Benefits Salary x .0030/2.
For more information on Long-Term benefits, click here.
Paid Time Off Benefits
Paid Time Off benefits available:
• Holidays
• Personal Time
• Vacation
• Parental Leave
For more information on Time Off benefits, click here
.

39
Holidays
Employees normally scheduled to work on company observed Holiday are eligible for Holiday Pay.
Mutual of Omaha Insurance Company observes 11 Holidays each year. If all 11 Holidays are not on
the Holiday Schedule below, then the remaining Holidays will be considered Floating Holidays and
they will be added to your Personal Time balance to be used at your discretion. The Cultural
Celebration holiday will always be a floating holiday and will be added to your Personal Time balance
each year.
Holiday Schedule for 2024
Mutual of Omaha Insurance Holidays
New Year’s Day
Martin Luther King, Jr. Day
Memorial Day
Independence Day
Day after Independence Day
Labor Day
Thanksgiving Day
Day after Thanksgiving Day
Christmas Day
Two Additional Personal Days
Personal Time
All regular new hire employees will receive eight hours and a pro-rated amount of Personal Time on
your date of hire. The chart below lists the full amount (8 hours + pro-rated amount) based on the
month you are hired. Following your first year of employment, you will receive an allotment of
personal time each year in January. Personal time does not rollover from year to year.
Personal time can be used for sick time, and at your discretion, with manager’s approval, for any time
away from work.
Personal Time – New Hire amount based on Standard Hours worked:
Hire Month
40 hrs/week
30 – 39 hrs/week
1/1/2024
56
42
2/1/2024
51.50
38.50
3/1/2024
47
35
4/1/2024
42.50
31.50
5/1/2024
38
28

40
6/1/2024
33.50
24.50
7/1/2024
29
21
8/1/2024
24.50
17.50
9/1/2024
20
14
10/1/2024
15.50
10.50
11/1/2024
11
8
12/1/2024
8
8
1/1/2025
56
42
Due to how the holidays fall in 2024 and 2025, the above chart reflects the additional pro-rated
personal time granted due to unused floating holidays and based upon the number of hours an
employee is scheduled to work. Regular employees with standard hours of less than 20 will not
receive any floating holidays.
Vacation
New employees will begin to accrue vacation on their benefits effective date. Vacation time can be
used at your discretion, and with manager’s approval, for any time away from work.
Years of Service
Annual Vacation
Accrual Rate
Hourly Accrual Rate Vacation Limit
Up to 5 yrs of service
15 days per year
0.057692
20 days
5 yrs of service
18 days per year
0.069231
23 days
10 yrs of service
20.5 days per year
0.078846
25.5 days
15 yrs of service
23 days per year
0.088462
28 days
25 yrs of service
28 days per year
0.107692
33 days
Vacation balances rollover from year to year. Accrual continues unless you reach the vacation limit.
This limit is equivalent to your accrual rate plus 5 days. We will notify you if you are nearing your limit.
Vacation is earned and accrued each pay period. The amount you receive may vary based on the
number of days, or hours worked, within the pay period.
To calculate your accrual each pay period, count the workdays between the 1st and the 15th or
between the 16th and the last day of the month. The number of workdays in that pay period will
determine your accrual. Below is an example of accrual rates per pay period, if working a standard
40-hour work week.
Accrual Rate
Based on Months
of Service
9-day
Pay Period
(72 hrs worked)
10-day
Pay Period
(80 hrs worked)
11-day
Pay Period
(88 hrs worked)
12-day
Pay Period
(96 hrs worked)
0 to 59
4.15 hrs
4.62 hrs
5.08 hrs
5.54 hrs
60 to 119
4.98 hrs
5.54 hrs
6.09 hrs
6.65 hrs
120 to 179
5.68 hrs
6.31 hrs
6.94 hrs
7.57 hrs
180 to 299
6.37 hrs
7.08 hrs
7.78 hrs
8.49 hrs
300 +
7.75 hrs
8.62 hrs
9.48 hrs
10.34 hrs

41
If you work less than 40 hours per week, count the number of hours worked during the pay period and
multiply by the hourly Accrual rate.
Your vacation balance will be visible on your pay advice and can be accessed using the Vacation
Planner. You will see your first vacation balance on the paycheck received on the 25th of the month
following your benefits effective date.
Benefits Effective Date
Pay Advice w/1st
Award of Vacation
01/01
01/25
02/01
02/25
03/01
03/25
04/01
04/25
05/01
05/25
06/01
06/25
07/01
07/25
08/01
08/25
09/01
09/25
10/01
10/25
11/01
11/25
12/01
12/25
For more information on Paid Time Off benefits, click here.
Parental Leave
Parental Leave provides up to four weeks of paid parental leave based upon the number of hours the
employee is regularly scheduled to work per week (two weeks coded as Parental Leave and two
weeks as additional vacation) per maternity/adoption occurrence for eligible employees with one full
year of continuous employment. Parental Leave will need to be taken within six months of the birth or
adoption.
For more information on Parental Leave benefits, click here
.

42
401(k) Long-Term Savings Plan
Our 401(k) plans are long term savings plans set up to assist you for saving for retirement, and we
encourage you to save appropriately.
All employees are eligible to participate in the 401(k) plan upon your benefits effective date.
You may contribute a total of 0-75% of your earnings on a Pre-Tax or After-Tax basis each pay period.
Employee contributions in partial fractional percentages are not allowed.
If you were accruing benefits under the Mutual of Omaha Retirement Income Plan as of December 31,
2016, the company will match 50% of your contributions, up to the first 7% of your eligible earnings.
If you were not accruing benefits under the Mutual of Omaha Retirement Income Plan as of
December 31, 2016 or were hired or rehired as an employee on or after January 1, 2017, Mutual of
Omaha will match $1 for $1 on the first 6% of your contributions. Mutual of Omaha will also contribute
an additional 2% of your compensation earned during the Plan year just for being an employee. This
additional 2% contribution will be known as the Employer Retirement Contribution (the “ERC”).
The company matching contributions and ERC are deposited at the same time as your contributions.
You are always 100% vested in your contributions and are immediately 100% vested in company
matching contributions (subject to gains and losses). However, if you are eligible for ERC, those
contributions are subject to a three-year graded vesting schedule as shown below:
Years of Service
% Vested
One
33%
Two
66%
Three
100%
Initial Enrollment: To begin your contributions in conjunction with your benefits effective date, your
initial enrollment will be part of your electronic benefits enrollment process.
Employee Contribution Changes: You may make changes in your employee contribution
percentage after your initial enrollment by going to Associate Access
.
Changes to your employee contribution percentage are processed in conjunction with each pay period
and will be processed as soon as administratively feasible.
Investment Election Changes: You may make changes to your asset allocations of contributions,
as well as transfer your existing account balances to different investment alternatives, by logging
onto your account through the Internet or by calling Mutual of Omaha Retirement Services at
1-888-917-7191. Information and directions will be emailed to you prior to your first contribution
and can also be found on Associate Access
.
Prior to age 59½, our plan does allow for loans and hardship withdrawals as defined by the IRS.
Your employee contributions to the Plan plus any amount deferred under other qualified retirement
plans cannot exceed a maximum set by the Internal Revenue Service for each calendar year. The
maximum employee contribution limit does not include catch-up contributions, which is for employees
over age 50.
Our plans do accept rollovers from other qualified plans. You can do this at any time. There are forms

43
to be completed and information on Associate Access.
For more information on your 401(k) benefits, click here
.
Voluntary ARAG Legal Services with ID Theft
Protection
The Mutual of Omaha Voluntary Legal Services Plan offers legal expense insurance through ARAG. If
you enroll in the voluntary legal services plan, you will receive access to consult with an attorney in
person or via phone and have access to a range of online resources.
Option
Coverage Provided
UltimateAdvisor
$9.77 per pay period
Identity Theft Protection, Consumer Protection, Criminal Matters, Real
Estate Matters, Debt-Related Matters, Wills and Estate Planning,
Divorce and DIY Documents
For more information on the ARAG Legal Service and Identity Theft Protection, click here.
Supplemental Health Benefits
Supplemental health benefits can help you pay for expenses not covered by health insurance. The
expenses may come from accidents, illness, and hospital stays.
Voluntary Accident Insurance
Accident insurance provides a lump-sum cash benefit for injuries you or an insured family member
sustains as a result of an accident. This benefit can help safeguard your savings by paying out-of-
pocket medical expenses as determined by the plan, supplementing daily living expenses and
covering lost income from unpaid time off work. Voluntary Accident Insurance coverage is effective on
your benefits effective date.
Current Voluntary Accident Pay Period Premiums
Employee Only
$4.70
Employee + 1
$7.45
Employee + Family
$11.34
For more information on Voluntary Accident Insurance, click here
.
Voluntary Critical Illness Insurance
A Critical Illness insurance policy can provide the extra security you need to help lessen the financial
impact associated with the treatment and recovery from a serious illness as determined by the plan.

44
Critical Illness insurance helps take care of your bills so you can focus on what’s most important –
recovery. Voluntary Critical Illness Insurance coverage is effective on your benefits effective date.
Current Voluntary Critical Illness Pay Period Premiums
Age
$5,000
$10,000
$15,000
$30,000
0-29
$0.55
$1.10
$1.65
$2.20
30-39
$1.00
$2.00
$3.00
$4.00
40-49
$2.20
$4.40
$6.60
$8.80
50-59
$4.63
$9.25
$13.88
$18.50
60-69
$9.63
$19.25
$28.88
$38.50
Form more information on Voluntary Critical Illness Insurance, click here.
Voluntary Hospital Indemnity Insurance
Hospital Indemnity Insurance supplements an employee’s existing health insurance coverage. It pays
a benefit to the insured to use as they wish to help them pay for any out-of-pocket expenses, they may
incur due to a hospital stay.
Current Voluntary Hospital Indemnity Pay Period Premiums
Employee Only
$4.50
Employee + 1
$9.50
Employee + Family
$12.25
For more information on Voluntary Hospital Indemnity Insurance, click here.
Other Benefits Available to You Throughout
the Year
Nationwide Pet Insurance
Pets become part of your family. When something happens, you want to do everything possible to
help them, but it can be expensive. Mutual offers pet insurance to help put your mind at ease and help
you be prepared when you need it most. This is an optional benefit.
Nationwide® covers a wide range of medical problems and conditions related to accidents and
illnesses, including cancer. It’s available for dogs, cats, birds and exotic pets. There is also an
additional wellness care option for vaccinations, flea/tick prevention and more. And you can use any
veterinarian worldwide even specialists and emergency care providers.

45
Enrollment can happen anytime during the year. You can also change or cancel your pet insurance
coverage at any point. Just remember pre-existing conditions are not covered. If you have questions
about the coverage or enrollment, call Nationwide at 877-738-7874 or visit PetsNationwide.com.
For more information on Nationwide Pet Insurance, click here.
Amplifon Hearing Discount Program
Do you or a family member live with hearing loss? Mutual of Omaha offers a comprehensive,
affordable hearing care program through Amplifon Hearing Health Care, one of the nation’s largest
providers of hearing discounts. There are no premiums or no sign up needed for this program. It is
available to you at any time as an active employee.
All you have to do to get started in order to get the discounts is call 888-713-7655 and Amplifon will
find a provider near you. A patient care advocate will explain the Amplifon process, get your mailing
information and assist you in making the appointment with a hearing care professional. Amplifon will
send information to you and the provider prior to the appointment.
For more information on Amplifon benefits offered to Mutual of Omaha employees and their family
members, click here.
Tuition Reimbursement Benefits
Mutual of Omaha offers generous tuition reimbursement programs for associates. We support life-
long learning and will reimburse up to 100 percent of tuition costs, with a maximum limit of $400 per
credit hour, for courses that meet the guidelines and have been successfully completed.
For more information on Tuition Reimbursement benefits, click here.
Refer to the Summary Plan Description
, found on Associate Access for a complete explanation of all
your group benefits.
Web Sites, Links and Contact Information
References
Aetna:
www.aetnanavigator.com
1-855-210-0024
When searching for a provider, make sure you Select “Aetna Choice POS II (Open Access)”
PrudentRX (Specialty Prescription Drugs)
800-578-4403
Maintenance Choice Opt-Out Program
1-888-792-3862 (Aetna)

46
Workplace Solutions Dental (Mutually Preferred network)
www.mutualofomaha.com/dental
800-927-9197
EyeMed Provider Link (Insight network)
www.eyemed.com
866-804-0982
401(k) Account Information
www.getretirementright.com
888-917-7191
ARAG Legal Services
www.ARAGlegal.com
800-247-4184
Voluntary Accident, Critical Illness and Hospital Indemnity Insurance (Workplace Solutions)
800-877-5176
Nationwide Pet Insurance
www.PetsNationwide.com
877-738-7874
Amplifon Heating Discount Program
888-713-7655
Benefits Hotline (For questions on your benefits and FSA processing)
Local (402) 351-3300 and select option “1” or Toll Free (800) 365-1405
Payroll Hotline (For questions regarding pay and taxes
(402) 351-3300 and select option “3” or Toll Free (800) 365-1405
Tuition Reimbursement Hotline (For questions regarding tuition reimbursement or e-learning)
(402) 351-3300 and select option “4” or Toll Free (800) 365-1405
